Validating Evolutionary Medicine: From Foundational Concepts to Clinical Applications in Biomedicine
This article provides a comprehensive framework for validating evolutionary medicine approaches tailored for researchers, scientists, and drug development professionals.
Validating Evolutionary Medicine: From Foundational Concepts to Clinical Applications in Biomedicine
Abstract
This article provides a comprehensive framework for validating evolutionary medicine approaches tailored for researchers, scientists, and drug development professionals. It systematically explores the foundational principles of evolutionary medicine, examines methodological applications in cancer therapy and antimicrobial resistance, addresses critical challenges in clinical translation, and presents rigorous validation paradigms through comparative studies and clinical evidence. By synthesizing current research and future directions, this review aims to establish evolutionary medicine as an evidence-based discipline capable of sparking transformational innovation in biomedical research and therapeutic development.
The Evolutionary Framework: Core Principles and Biological Evidence
Evolutionary medicine, also known as Darwinian medicine, represents a paradigm shift in how we understand health and disease. This field applies the principles of evolutionary biology to explain why organisms are vulnerable to disease, providing a crucial complementary perspective to traditional medical research that focuses primarily on proximate mechanistic explanations [1]. Rather than viewing the body as a perfectly engineered machine, evolutionary medicine recognizes that organisms are bundles of compromises shaped by natural selection to maximize reproductive success, not health [2]. This fundamental insight challenges conventional medical thinking and offers powerful new approaches for prevention and treatment.
The formal establishment of evolutionary medicine as a distinct discipline dates to the 1990s with the pioneering work of George C. Williams and Randolph Nesse, whose seminal book "Why We Get Sick" laid the foundation for systematically applying evolutionary principles to medical science [3] [4]. Since then, the field has grown exponentially, contributing critical insights to diverse areas including infectious disease, cancer, aging, and mental health [5] [6]. This article provides a comprehensive comparison of evolutionary medicine approaches, validating their application across biomedical research domains through experimental data and methodological frameworks.
Core Principles and Conceptual Framework
Through a systematic Delphi method study involving 56 experts across anthropology, medicine, biology, and related fields, researchers have established 14 core principles that form the foundation of evolutionary medicine [6]. These principles provide a conceptual framework for understanding how evolutionary processes shape disease vulnerability and can be grouped into five overarching categories that distinguish evolutionary from traditional medical approaches.
Table 1: Core Principles of Evolutionary Medicine
| Category | Core Principle | Clinical Significance |
|---|---|---|
| Question Framing | Both proximate (mechanistic) and ultimate (evolutionary) explanations are needed for complete biological understanding | Explains why we need both molecular mechanisms AND evolutionary reasons for disease vulnerability |
| Evolution I | Natural selection maximizes reproductive success, sometimes at the expense of health and longevity | Explains aging and late-life diseases |
| Evolutionary Trade-offs | Changes that improve fitness can be linked to changes that decrease fitness | Explains why beneficial adaptations may have costly side effects |
| Reasons for Vulnerability | Disease risks increase when organisms live in environments different from their evolutionary past | Explains modern epidemics of obesity, diabetes, and heart disease |
| Culture | Cultural practices can influence evolution of humans and other species in ways affecting health | Explains antibiotic resistance and impacts of modern diet |
These principles highlight the distinctive value of evolutionary perspectives in addressing fundamental questions about disease vulnerability that remain unexplained by proximate mechanisms alone [6] [2]. Where traditional medicine might ask "how does a disease process work?", evolutionary medicine asks the complementary question "why has natural selection left us vulnerable to this disease?" This dual approach provides a more comprehensive biological understanding of health and disease [1].
Pathways to Disease Vulnerability
Evolutionary medicine identifies several key pathways through which evolutionary processes influence disease risk. Nesse and Stearns originally identified six core pathways, later expanded by Gluckman et al. to incorporate aspects of population genetics, providing a systematic framework for classifying evolutionary contributions to disease [4].
Table 2: Evolutionary Pathways to Disease
| Pathway | Conceptual Basis | Clinical Examples |
|---|---|---|
| Mismatch | Exposure to novel environments beyond evolutionary adaptation | Myopia, metabolic syndrome, cardiovascular disease |
| Life History-Associated Factors | Trade-offs and antagonistic pleiotropy across lifespan | Early life nutritional effects on adult metabolic disease |
| Excessive Defense Mechanisms | Dysregulation of normally adaptive defenses | Fever, inflammation, anxiety responses |
| Human-Pathogen Coevolution | Rapid microbial evolution relative to human evolution | Antibiotic resistance, emerging infectious diseases |
| Evolutionary Constraints | Consequences of evolutionary history on anatomical features | Back pain from bipedalism, vulnerable optic nerve placement |
| Balancing Selection | Heterozygote advantage maintaining deleterious alleles | Sickle cell anemia, cystic fibrosis |
These pathways demonstrate how evolutionary perspectives provide ultimate explanations for disease vulnerability that complement proximate mechanistic explanations [4] [2]. For instance, the persistence of sickle cell anemia alleles is explained not by beneficial effects of the disease itself, but through the protective advantage against malaria in heterozygous carriers - a classic example of balancing selection [4].
Figure 1: Evolutionary Pathways to Disease Vulnerability. This diagram illustrates key conceptual relationships between evolutionary processes and disease risk, highlighting how adaptive traits, environmental mismatch, host-pathogen dynamics, and developmental programming contribute to vulnerability.
Comparative Analysis of Research Methodologies
Evolutionary medicine employs distinct methodological approaches that differentiate it from traditional biomedical research while complementing its findings. These methodologies enable researchers to test evolutionary hypotheses and apply them to clinical challenges.
Phylogenetic Comparative Methods
Phylogenetic comparative methods (PCMs) represent a powerful toolkit for evolutionary medicine, allowing researchers to analyze trait evolution across species while accounting for shared evolutionary history [7]. These methods transform biomedical research by enabling systematic comparisons across diverse species to understand the evolutionary origins of disease vulnerabilities.
Table 3: Phylogenetic Comparative Methods in Evolutionary Medicine
| Method | Theoretical Basis | Research Applications |
|---|---|---|
| Brownian Motion Model | Traits evolve via random walk | Neutral evolution null hypothesis |
| Ornstein-Uhlenbeck (OU) Model | Traits experience stabilizing selection toward optimum | Adaptation to specific environmental conditions |
| Rate Trend Model | Evolutionary rates change over time | Detecting accelerated/decelerated trait evolution |
| Mean Trend Model | Directional change in traits over time | Investigating persistent selective pressures |
| Pagel's λ | Measures phylogenetic signal | Quantifying evolutionary constraints on traits |
These PCMs have been particularly transformative in comparative oncology, revealing how cancer risk varies across the tree of life and challenging conventional assumptions about carcinogenesis [7]. For example, applying PCMs to cross-species cancer data has demonstrated that cancer susceptibility is linked to life history strategies, with fast-lived species showing different cancer defense investments than slow-lived species, independent of body size [7].
Experimental Approaches in Evolutionary Medicine
Evolutionary medicine employs distinctive experimental protocols that differ from traditional biomedical approaches both in methodology and conceptual framework. These approaches are characterized by their emphasis on evolutionary dynamics rather than static mechanisms.
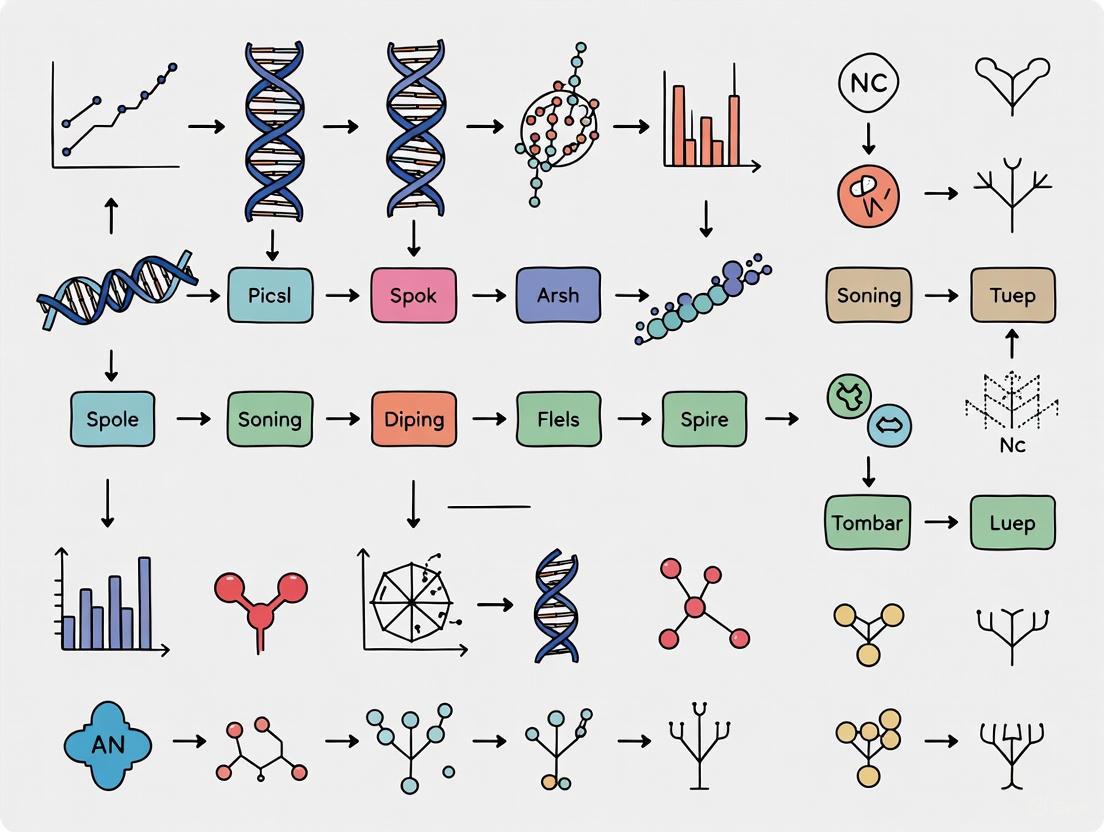
Figure 2: Experimental Workflow in Evolutionary Medicine Research. This diagram outlines the systematic approach from question formulation through method selection to clinical application, highlighting distinctive methodological pathways.
Protocol 1: Testing Evolutionary Mismatch Hypotheses
- Objective: Determine if disease prevalence results from mismatch between evolved traits and modern environments [4]
- Methodology: Comparative analysis of populations with different environmental exposures
- Controls: Populations maintaining ancestral lifestyle patterns
- Parameters: Biomarkers of metabolic health, immune function, cardiovascular status
- Validation: Consistency with paleontological and anthropological evidence
- Applications: Understanding obesity, diabetes, autoimmune diseases [5]
Protocol 2: Experimental Evolution of Drug Resistance
- Objective: Model and manipulate evolution of treatment resistance in pathogens and cancers [8] [5]
- Methodology: In vitro or in vivo serial passage under therapeutic pressure
- Controls: Lines propagated without selective pressure
- Parameters: Mutation rates, fitness costs, cross-resistance profiles
- Interventions: Alternative drug schedules, combination therapies, evolutionary steering
- Applications: Optimizing antibiotic and chemotherapy protocols [8]
Protocol 3: Phylogenetic Trait Mapping
- Objective: Identify evolutionary origins of disease vulnerability and protective mechanisms [7]
- Methodology: Comparative analysis of trait distribution across phylogeny
- Data Requirements: Phenotypic traits, genomic data, phylogenetic relationships
- Analytical Tools: Maximum likelihood, Bayesian inference, phylogenetic independent contrasts
- Outputs: Evolutionary correlations, ancestral state reconstructions, selection tests
- Applications: Discovering natural models of disease resistance [5] [7]
Comparative Analysis of Evolutionary Applications
Infectious Disease Management
Evolutionary approaches have fundamentally transformed infectious disease research and management, particularly in understanding and combating antibiotic resistance. Where traditional approaches focus on killing pathogens, evolutionary medicine emphasizes managing the evolutionary dynamics of resistance development [8].
Research by Read and Huijben on malaria demonstrates how evolutionary principles can inform drug treatment protocols to slow resistance development [8]. Their work challenges conventional thinking by showing that current drug use protocols are "dangerously suboptimal from an evolutionary standpoint" and proposes alternative strategies based on evolutionary theory [8]. Similarly, experimental systems using bacteria and phage have revealed how co-infection dynamics significantly affect pathogen evolution, with important implications for disease control strategies [8].
Cancer Biology and Treatment
Evolutionary medicine reframes cancer as an ecological and evolutionary problem of controlling cellular "cheaters" within the cooperative system of multicellular life [5]. This perspective has inspired innovative therapeutic approaches that explicitly target the evolutionary dynamics of treatment resistance.
Table 4: Evolutionary Approaches to Cancer Therapy
| Approach | Mechanism | Experimental Evidence |
|---|---|---|
| Adaptive Therapy | Maintains treatment-sensitive cells to suppress resistant competitors | Mathematical modeling and in vivo studies show prolonged disease control |
| Extinction Therapy | Uses evolutionary principles to eradicate resistant subclones | Combination therapies designed to prevent escape pathways |
| Evolutionary Steering | Directs tumor evolution toward less aggressive phenotypes | In silico models and early clinical trials demonstrate feasibility |
| Life History Analysis | Exploits trade-offs in cancer cell energetics | Cross-species comparisons inform vulnerability identification |
Recent research leveraging phylogenetic comparative methods has further revealed how cancer risk varies across species in relation to life history strategies, providing insights into natural cancer suppression mechanisms that could be therapeutically harnessed [7]. For example, comparing cancer prevalence across the animal kingdom has identified species with exceptional cancer resistance, offering models for understanding natural protection mechanisms [5].
Metabolic and Cardiovascular Diseases
Evolutionary perspectives provide powerful explanations for the epidemic of metabolic and cardiovascular diseases in modern populations [3] [4]. The concept of evolutionary mismatch explains how traits that were advantageous in ancestral environments become detrimental in contemporary contexts.
Research on insulin resistance illustrates this principle, showing how a "thrifty genotype" that enabled efficient fat storage during feast-famine cycles now predisposes to obesity and type 2 diabetes in environments of constant caloric abundance [3]. Similarly, evolutionary cardiology has identified how antagonistic pleiotropy contributes to cardiovascular aging, with genes beneficial in early life becoming detrimental in post-reproductive years [3].
Experimental approaches in evolutionary cardiology investigate mechanisms like antagonistic pleiotropy, where genes such as those in the renin-angiotensin-aldosterone system (RAAS) provide early-life benefits but contribute to hypertension and atherosclerosis later in life [3]. This evolutionary framework recasts common cardiovascular conditions not as simple mechanical failures but as consequences of evolved trade-offs.
Research Tools and Reagent Solutions
Evolutionary medicine employs specialized research tools that enable the testing of evolutionary hypotheses and the application of evolutionary principles to biomedical challenges.
Table 5: Essential Research Toolkit for Evolutionary Medicine
| Tool Category | Specific Tools/Reagents | Research Applications |
|---|---|---|
| Phylogenetic Analysis | BEAST, RevBayes, PHYLIP, phylogenetic comparative methods | Reconstructing evolutionary relationships and trait evolution [7] |
| Experimental Evolution | Chemostats, animal models, serial passage systems | Studying real-time evolution of pathogens and cancer cells [8] |
| Genomic Tools | Whole genome sequencing, population genetics software | Identifying selection signatures, evolutionary constraints [3] |
| Mathematical Modeling | Evolutionary game theory, population dynamics models | Predicting evolutionary trajectories, treatment optimization [8] |
| Comparative Physiology | Cross-species phenotypic assays | Identifying natural models of disease resistance [5] |
These tools enable researchers to address fundamental questions about evolutionary constraints, trade-offs, and vulnerabilities that cannot be adequately investigated using traditional biomedical approaches alone. For example, phylogenetic comparative methods allow researchers to test hypotheses about the relationship between life history traits and disease vulnerability across species, controlling for shared evolutionary history [7].
Validation and Clinical Translation
The validation of evolutionary medicine approaches relies on both theoretical consistency and empirical evidence across multiple research domains. Several key areas demonstrate the successful translation of evolutionary principles into clinical insights and interventions.
Pandemic Preparedness and Management
The COVID-19 pandemic dramatically illustrated the critical importance of evolutionary principles in managing public health crises [5]. Evolutionary dynamics guided understanding of viral virulence and transmissibility, informed vaccine development strategies, and predicted the emergence of variants. This application provided real-world validation of evolutionary medicine's capacity to address global health challenges.
Research during the pandemic demonstrated how evolutionary principles could also be used to understand and address human behaviors that impede public health efforts, such as vaccine hesitancy [5]. This highlights the broader applicability of evolutionary thinking beyond purely biological mechanisms to encompass behavioral and cultural dimensions of health.
Drug Development and Resistance Management
Evolutionary approaches have produced validated strategies for addressing one of modern medicine's most pressing challenges: antimicrobial resistance [8] [5]. Research by Read and Huijben has demonstrated how evolutionary principles can inform drug treatment protocols for malaria to slow resistance development [8]. Similarly, evolutionary insights have inspired innovative approaches to cancer therapy that explicitly target the evolutionary dynamics of treatment resistance [5].
Experimental systems using bacteria and phage have revealed fundamental principles about pathogen evolution that have direct clinical applications [8]. For example, work by Joseph et al. demonstrated that bacteria infected with phage can become more susceptible to further infection, revealing evolutionary vulnerabilities that could be therapeutically exploited [8].
Preventive Medicine and Public Health
Evolutionary perspectives have successfully informed preventive approaches to modern metabolic and cardiovascular diseases by identifying mismatch between evolved human physiology and contemporary environments [4] [2]. The recognition that many modern pathologies result from disparities between ancestral and current lifestyles has provided a theoretical foundation for lifestyle interventions and public health recommendations.
Life-history evolution has similarly shed important light on patterns of disease burden, particularly in reproductive health [5]. This has enabled more evolutionarily-informed approaches to women's health across the lifespan, recognizing how trade-offs between reproduction and somatic maintenance influence disease risk.
Evolutionary medicine provides an essential framework that complements traditional biomedical approaches by addressing the ultimate causes of disease vulnerability rather than solely focusing on proximate mechanisms [1]. The validation of evolutionary medicine approaches across diverse domains - from infectious disease and cancer to metabolic disorders and public health - demonstrates the transformative potential of integrating evolutionary perspectives into biomedical research and clinical practice.
The distinctive methodologies of evolutionary medicine, including phylogenetic comparative methods, experimental evolution, and mismatch analysis, enable researchers to address fundamental questions about why organisms are vulnerable to disease that cannot be adequately answered through traditional approaches alone [7] [1]. As the field continues to develop, evolutionary medicine promises to spark further innovation in biomedical research, clinical care, and public health by applying the powerful explanatory framework of evolutionary theory to the challenges of human health and disease [5].
The growing recognition of evolutionary medicine's value is reflected in recommendations from leading scientific organizations, including the Association of American Medical Colleges and the Howard Hughes Medical Institute, which have listed evolutionary thinking as a core competency for pre-medical education [6]. As research continues to validate evolutionary approaches and demonstrate their clinical utility, evolutionary medicine is poised to become an increasingly integral component of comprehensive biomedical science.
The rising global burden of non-communicable diseases (NCDs) presents a critical challenge to modern healthcare systems. Conditions such as obesity, cardiovascular disease, type 2 diabetes, and autoimmune disorders are among the long list of "lifestyle" diseases that were rare throughout most of human history but are now common causes of mortality and morbidity worldwide [9]. The evolutionary mismatch hypothesis provides a powerful framework for understanding this phenomenon, positing that humans evolved in environments that radically differ from those we currently experience [10]. Consequently, biological traits that were once advantageous in ancestral environments may now be "mismatched" to modern contexts, becoming disease-causing factors [9] [11].
This paradigm represents a significant expansion of evolutionary medicine, which applies modern evolutionary theory to understanding health and disease [2]. Rather than focusing solely on proximate mechanistic causes of disease, evolutionary medicine asks why evolution has shaped our physiological mechanisms in ways that leave us susceptible to disease [2]. The core premise is that natural selection maximizes reproductive success, not health or longevity, and this occurs within numerous biological constraints and trade-offs [2]. The concept of mismatch has gained substantial traction in recent years as researchers recognize that many contemporary health challenges stem from the discordance between our ancient biology and modern environments [12].
The global impact of NCDs underscores the importance of this approach. According to World Health Organization estimates, non-communicable diseases were responsible for 41 million deaths annually—representing 71% of all global deaths [13]. Cardiovascular diseases accounted for 17.9 million deaths, cancers for 9.0 million, chronic respiratory diseases for 3.8 million, and diabetes for 1.6 million [13]. This substantial worldwide impact highlights the necessity for more holistic, evolutionarily-informed approaches to comprehend and manage these conditions.
Theoretical Foundations and Key Principles
Defining Evolutionary Mismatch
Evolutionary mismatch can be formally defined as the phenomenon by which previously adaptive traits are no longer favored in a new environment, leading to negative health consequences [11] [12]. This occurs when organisms, including humans, possess traits that were shaped by natural selection in ancestral environments but prove inadequate or maladaptive in novel contexts [12]. The mismatch framework operates across space and time, explaining how rapid environmental changes can outpace biological adaptation, resulting in increased disease susceptibility [9].
Several core criteria must be satisfied to establish a condition as an evolutionary mismatch [9]. First, the disease-related phenotype must be more common or severe in novel environments compared to ancestral conditions. Second, these phenotypes must be attributable to specific environmental variables that differ significantly between ancestral and modern contexts. Third, there must be a plausible mechanism explaining how the environmental shift generates variation in disease-related phenotypes, often manifesting as genotype-by-environment (GxE) interactions where genetic variants have different health effects depending on environmental context [9].
The Environment of Evolutionary Adaptedness
Central to the mismatch concept is the Environment of Evolutionary Adaptedness (EEA), typically identified as the African savannah approximately 50,000 years ago and earlier, where humans evolved as small nomadic hunter-gatherers in tribal bands [10] [12]. Our species spent hundreds of millennia adapting to the selection pressures of this foraging lifestyle, with relatively little time evolving since the advent of agriculture (10,000 years ago) and civilization (5,000 years ago) [10]. Consequently, Homo sapiens remain primarily adapted to Pleistocene conditions, creating a fundamental mismatch when our ancient biology encounters modern environments [12].
Anthropological evidence indicates that human genetics and anatomy have remained largely unchanged for approximately 100,000 years, while our cultural and technological environment has transformed dramatically, especially within the past few generations [10]. This disparity creates what researchers term "adaptation delays" or "maladaptations," where human culture and technology evolve faster than biological evolution can track, leading to inevitable mismatches [13].
Extended Evolutionary Synthesis and Cultural Evolution
Contemporary evolutionary theory, particularly the Extended Evolutionary Synthesis, provides a sophisticated framework for understanding mismatch phenomena [13]. This postmodern evolutionary perspective extends beyond the traditional gene-centered view to incorporate cultural evolution, niche construction, and multiple forms of inheritance [13]. Unlike biological evolution driven by genetic mutation and natural selection, cultural evolution operates through the transmission of information via learning, imitation, and social interaction [13].
Cultural evolution can produce both adaptive innovations (such as medical advances) and maladaptive outcomes (mismatches) when cultural practices become misaligned with our evolutionary heritage [13]. The rapid pace of socio-techno-cultural change in the Anthropocene makes biological adaptation almost impossible, given that natural selection operates over thousands to millions of years, while cultural and technological innovations can transform human environments within generations [13]. This fundamental difference in timescales creates the conditions for widespread evolutionary mismatches affecting human health.
Comparative Analysis of Mismatch-Related Diseases
Table 1: Health Conditions Linked to Evolutionary Mismatch
| Disease/Condition | Ancestral Environment Context | Modern Environment Trigger | Key Mismatch Mechanism |
|---|---|---|---|
| Obesity & Metabolic Disease | Feast-or-famine food availability; high physical activity required for subsistence | Abundant, calorie-dense processed foods; sedentary lifestyle | "Thrifty" genotype favoring energy storage mismatched to environment of caloric abundance [9] [11] [10] |
| Autoimmune & Inflammatory Diseases | High parasite/microbe exposure; co-evolution with helminths | Extreme hygiene; microbiome depletion | Immune system regulation dependent on missing microbial cues [11] [2] |
| Cardiovascular Disease | High physical activity; unprocessed, high-fiber diet | Sedentary behavior; atherogenic diet | Mismatch between evolved physiology and novel risk factors [13] [9] |
| Myopia | Outdoor activity with varied visual distances | Prolonged near-work; limited outdoor time | Lack of developmental stimuli for proper eye growth [12] |
| Mental Health Disorders (Depression/Anxiety) | Tight-knit social communities; immediate survival goals; meaningful ritual | Social isolation; abstract goals; loss of traditional meaning structures | Mismatch between evolved social needs and contemporary living patterns [10] |
Table 2: Quantitative Evidence for Evolutionary Mismatch Across Populations
| Study/Population | Traditional Lifestyle Metrics | Industrialized/Westernized Metrics | Health Outcome Difference |
|---|---|---|---|
| Global Transition | Historical hunter-gatherer societies | Contemporary industrialized societies | NCDs account for 71% of global deaths vs. rare in ancestral contexts [13] |
| Turkana Health & Genomics Project [9] | Pastoralist lifestyle | Urbanized community members | Rapid emergence of metabolic, cardiovascular, and autoimmune conditions with urbanization |
| Tsimane Health & Life History Project [9] | Subsistence hunting-gathering-farming | Increasing market integration | Graded increase in NCD risk factors with lifestyle modernization |
| Vitamin C Intake | ~500 mg/day in contemporary hunter-gatherers [12] | ~90 mg/day U.S. recommended daily minimum [12] | Scurvy in extreme cases; potential suboptimal immune function in modern contexts |
Research Methodologies for Studying Evolutionary Mismatch
Experimental Framework and Study Designs
Research into evolutionary mismatch employs specialized methodological approaches designed to detect genotype-by-environment (GxE) interactions and their health consequences. These methodologies typically involve partnerships with subsistence-level populations experiencing rapid lifestyle change, creating natural experiments for studying the transition from traditional to modern lifeways [9]. These partnerships leverage long-term anthropological work that has already characterized the ecology and culture of these groups, setting the stage for genomic integration [9].
The key methodological approaches include:
- Cross-sectional comparisons of individuals from the same genetic background living at different points along the "matched" to "mismatched" spectrum [9]
- Longitudinal studies tracking health outcomes as populations undergo lifestyle transitions [9]
- Genome-wide association studies specifically designed to detect GxE interactions in populations with extreme environmental variation [9]
- Physiological measurements comparing metabolic, immune, and cardiovascular function across lifestyle gradients [9]
These approaches explicitly sample environmental extremes, thereby boosting statistical power to detect GxE interactions that have been challenging to identify in more homogeneous postindustrial populations [9].
Research Workflow for Evolutionary Mismatch Studies
Table 3: Key Research Reagents and Resources for Mismatch Studies
| Resource Category | Specific Examples | Research Application |
|---|---|---|
| Genomic Analysis Tools | Whole-genome sequencing arrays, SNP genotyping panels, epigenetic clocks, microbiome sequencing kits | Genetic variant identification, ancestry determination, epigenetic aging assessment, microbial community characterization [9] |
| Physiological Assessment | Accelerometers, continuous glucose monitors, ambulatory blood pressure monitors, DEXA scanners, metabolic carts | Objective measurement of physical activity, metabolic responses, body composition, and energy expenditure [9] |
| Environmental Exposure Assessment | Food frequency questionnaires, GPS trackers, environmental sensors, air and water quality monitors | Quantification of dietary patterns, movement ecology, and environmental exposures [9] |
| Biomarker Analysis | ELISA kits, mass spectrometry, flow cytometry, inflammatory marker panels, lipid profiles | Measurement of immune function, metabolic health, cardiovascular risk factors, and stress responses [9] |
| Computational Resources | GxE interaction analysis pipelines, phylogenetic reconstruction software, landscape phylogeography tools | Statistical analysis of genotype-environment interactions, evolutionary history reconstruction, spatial spread analysis [14] [9] |
Key Experimental Findings and Mechanistic Insights
Genetic Loci with Mismatch Effects
Research combining anthropological and genomic methods has begun to identify specific genetic loci exhibiting mismatch effects—where alleles with neutral or beneficial effects in traditional environments become detrimental in modern contexts. These loci typically show strong GxE interactions, with different health impacts depending on environmental context [9]. For example, genes related to energy metabolism and storage that were likely advantageous in environments with fluctuating food availability now contribute to obesity and diabetes risk in calorically abundant environments [9] [11].
The "thrifty genotype" hypothesis, first proposed by James Neel in 1962, suggested that genes promoting efficient fat storage would have been advantageous in ancestral environments with periodic food scarcity but become detrimental with constant food abundance [11]. Contemporary research has expanded this concept to numerous physiological systems beyond metabolism, including immune regulation, stress response, and neurodevelopment [9] [2].
The Hygiene Hypothesis and Immune Mismatch
The hygiene hypothesis represents a well-supported example of evolutionary mismatch in immune function. Humans evolved in environments rich with biodiversity, including helminthic worms that co-evolved to regulate our immune systems [11] [2]. The near-elimination of these organisms from modern industrialized environments, due to improved sanitation and medical practices, has been implicated in various hyper-inflammatory conditions, including multiple sclerosis, inflammatory bowel disease, and allergic disorders [11] [2].
This mismatch arises because the human immune system developed a dependency on certain microorganisms, particularly during early development, to properly calibrate its responses [2]. Without these regulatory influences, the immune system may become prone to excessive inflammation or autoimmunity [11]. This mechanistic understanding has led to novel therapeutic approaches, including helminthic therapy trials that attempt to "reunite" the human immune system with components of its evolutionary environment [11].
Immune System Mismatch Mechanism
Cultural Evolution and Mismatch Dynamics
Cultural evolutionary processes create distinct mismatch dynamics that operate alongside genetic evolutionary mechanisms. Unlike biological evolution, cultural evolution can produce rapid environmental changes through processes such as technological innovation, social learning, and information transmission [13]. These changes can occur within generations, far outpacing the slow pace of genetic adaptation [13].
Maladaptive cultural evolution occurs when cultural practices, beliefs, or innovations that were intended to improve living standards instead produce unintended negative health consequences [13]. Examples include the development of hyperpalatable foods that exploit our evolved taste preferences, sedentary technologies that reduce physical activity, and social media platforms that hijack our evolved social validation systems [13] [10]. These cultural innovations create novel environments that differ dramatically from those in which our ancestors evolved, generating new forms of evolutionary mismatch [13].
Implications for Therapeutic Development and Public Health
Evolution-Informed Drug Discovery and Development
The evolutionary mismatch framework offers valuable insights for pharmaceutical research and development. By understanding the evolutionary context of disease mechanisms, drug developers can identify more relevant therapeutic targets and improve preclinical models [9]. For example, recognizing that many modern inflammatory conditions result from the absence of evolutionary expected microbial exposures suggests novel approaches to immunomodulation that work with, rather than against, our evolved biology [11].
Additionally, understanding GxE interactions can help stratify patient populations for clinical trials, potentially identifying subgroups most likely to respond to specific interventions based on their genetic profiles and environmental contexts [9]. This approach may be particularly valuable for conditions like obesity, where individual responses to pharmacological interventions vary significantly based on genetic factors that evolved in different environmental contexts [9].
Public Health and Preventive Medicine Applications
Evolutionary mismatch theory provides a powerful framework for redesigning public health approaches to chronic disease prevention. Rather than focusing solely on individual behavior change, an evolutionary perspective emphasizes creating environments that are better aligned with human biology [10]. This might include:
- Designing food environments that leverage, rather than exploit, our evolved taste preferences
- Creating built environments that naturally encourage physical activity through walkability and access to nature
- Developing social policies that support the maintenance of strong community bonds and meaning structures [10]
Healthcare professionals can use mismatch concepts to help patients reframe self-blame for health conditions, understanding that many modern health challenges arise from biology-environment mismatches rather than personal failings [10]. This perspective can foster self-compassion while simultaneously motivating environmentally-focused solutions [10].
The evolutionary mismatch framework represents a paradigm shift in how we understand human health and disease. By integrating insights from evolutionary biology, anthropology, genetics, and medicine, researchers and clinicians can develop more effective, compassionate approaches to preventing and treating the chronic diseases that dominate modern healthcare. As the field continues to evolve, partnerships with diverse populations and interdisciplinary collaboration will be essential for unraveling the complex interactions between our ancient biology and modern environments that shape health outcomes across the globe.
Evolutionary medicine proposes that the challenges of human disease can be better understood by studying the evolved adaptations of other species. The core premise is that natural selection, acting over millions of years on thousands of species, has already solved many physiological challenges that modern medicine seeks to address [15]. Biomimetics, the practice of learning from and mimicking nature's strategies, provides a powerful framework for translating these evolutionary solutions into biomedical innovations [16]. This approach is particularly valuable for understanding disease resistance, as numerous species have evolved remarkable mechanisms to avoid or tolerate pathologies that commonly afflict humans, from metabolic diseases to cancer and age-related degeneration.
The validation of evolutionary medicine hinges on moving from observational correlations to mechanistic insights. By studying species with extreme phenotypes—such as the shark's resistance to cancer, the naked mole-rat's exceptional longevity, or the cavefish's protection from diabetic complications—researchers can identify novel therapeutic targets and treatment paradigms [15] [17]. This guide objectively compares the experimental data and methodologies used to study these disease-resistant species, providing researchers with a framework for validating evolutionary insights through rigorous biomedical research.
Comparative Analysis of Disease-Resistant Species and Their Adaptive Mechanisms
Research into disease-resistant species spans diverse physiological systems and pathologies. The table below synthesizes key findings from current research on species with exceptional resistance to metabolic disorders, age-related diseases, and other pathologies relevant to human health.
Table 1: Comparative Analysis of Disease-Resistant Species and Key Adaptations
| Species | Disease Resistance Phenotype | Key Adaptive Mechanisms | Experimental Evidence | Potential Biomedical Applications |
|---|---|---|---|---|
| Hibernating Brown Bear (Ursus arctos) | Reversible insulin resistance; protection from muscle atrophy during prolonged immobility [17] | Seasonal metabolic plasticity; regulated suppression of insulin signaling [17] | Serum biomarkers show reversible insulin resistance between hibernation and active seasons [17] | Novel targets for managing metabolic syndrome; therapies for preventing disuse atrophy [17] |
| Naked Mole-Rat (Heterocephalus glaber) | Exceptional longevity; cancer resistance [17] | Enhanced protein stability; early contact inhibition (p16-mediated) [15] | Genomic analyses reveal unique tumor suppressor mechanisms; <1% cancer incidence despite longevity [15] | Cancer prevention strategies; age-related disease interventions [15] [17] |
| Blind Cavefish (Astyanax mexicanus) | Protection from diabetic complications despite insulin resistance [17] | Mitochondrial metabolic shifts; protective mechanisms against AGE accumulation [17] | Comparative studies between cave-dwelling and surface populations show differential response to hyperglycemia [17] | Novel approaches to prevent diabetic complications without glycemic control [17] |
| Bottlenose Dolphin (Tursiops truncatus) | Healthy maintenance despite prolonged postprandial hyperglycemia and hyperinsulinemia [17] | Metabolic switching capability; protective biochemical systems [17] | Blood sampling shows natural postprandial hyperglycemia without pathological sequelae [17] | Models for understanding diet-induced metabolic regulation [17] |
| Greenland Shark (Somniosus microcephalus) | Extreme longevity (>400 years); minimal age-related pathology [17] | Cellular maintenance and repair mechanisms; stress resistance pathways [17] | Radiocarbon dating confirms exceptional lifespan; tissue analyses reveal unique cellular properties [17] | Longevity and age-related disease research [17] |
Experimental Approaches for Validating Evolutionary Adaptations
Methodologies for Studying Metabolic Adaptations in Extreme Phenotypes
Research into species with exceptional metabolic adaptations employs specialized protocols to characterize their unique physiology:
Seasonal Metabolic Profiling in Hibernators: Studies of hibernating bears involve careful seasonal sampling of blood and tissue to analyze changes in metabolic hormones, substrate utilization, and tissue-specific responses. This includes tracking insulin, glucose, fatty acids, and ketone bodies across hibernation cycles, alongside measures of body composition and vital signs. Muscle biopsies assess protein synthesis rates and markers of atrophy, revealing mechanisms that prevent muscle loss despite months of immobility [17].
Comparative Physiology in Insulin-Resistant Models: Research on dolphins and cavefish employs controlled challenge tests similar to human oral glucose tolerance tests. For dolphins, this involves serial blood sampling after feeding to characterize the magnitude and duration of postprandial hyperglycemia and the corresponding insulin response. In cavefish, researchers compare glucose handling, insulin sensitivity, and tissue damage markers between cave-adapted and surface-dwelling populations under identical nutritional challenges, identifying protective mechanisms independent of glycemic control [17].
Multi-Omics Integration for Mechanism Discovery: Advanced genomic, transcriptomic, proteomic, and metabolomic analyses are applied to disease-resistant species to identify molecular signatures of protection. This includes sequencing and comparing genomes of long-lived versus short-lived species, profiling gene expression in tissues under various physiological states, and characterizing proteins and metabolites that may confer protection. These data are integrated to build comprehensive models of protective physiological mechanisms [17] [18].
Validation Workflows for Biomimetic Drug Discovery
The translation of observations from disease-resistant species into potential human therapies follows a structured validation pathway:
Table 2: Experimental Validation Workflow for Biomimetic Drug Discovery
| Research Phase | Key Objectives | Methodologies | Outputs |
|---|---|---|---|
| 1. Phenotypic Characterization | Document disease-resistant phenotype in source species | Field observations; comparative physiology; metabolic profiling; histopathological screening [17] | Quantitative description of protective phenotype (e.g., absence of complications despite risk factors) |
| 2. Mechanistic Elucidation | Identify molecular and physiological basis of protection | Genomic sequencing; gene expression profiling; protein analysis; targeted genetic manipulation [17] [18] | Candidate pathways, genes, or molecules responsible for protective effect |
| 3. Functional Validation | Confirm causal role of identified mechanisms | CRISPR/Cas9 gene editing; transgenic models; biochemical inhibition/activation studies [18] | Verified molecular targets with demonstrated necessity and sufficiency for phenotype |
| 4. Therapeutic Translation | Develop interventions based on validated mechanisms | Peptide synthesis; small molecule screening; antibody development; preclinical testing in disease models [17] | Candidate therapeutic agents with demonstrated efficacy in model systems |
Biomimetic Signaling Pathways in Disease-Resistant Species
Several conserved molecular pathways recurrently appear in studies of disease-resistant species, suggesting their importance in evolutionary adaptations against disease. The diagram below illustrates the Nrf2-KEAP1 pathway, a central regulatory system identified in multiple resilient species.
Figure 1: The NRF2-KEAP1 Cytoprotective Pathway
This conserved pathway, mentioned in studies of elephants, seals, and camels, coordinates the expression of hundreds of cytoprotective genes involved in antioxidant defense, inflammation regulation, and mitochondrial biogenesis [15] [17]. In disease-resistant species, this pathway often shows enhanced regulation or unique modulation, contributing to their resilience against environmental stressors and age-related pathologies.
The Scientist's Toolkit: Essential Reagents for Biomimetics Research
Research into disease-resistant species requires specialized reagents and tools to elucidate their unique biological mechanisms. The following table details essential research solutions for this emerging field.
Table 3: Essential Research Reagents for Biomimetics and Evolutionary Medicine Studies
| Reagent/Category | Specific Examples | Research Applications | Key Functions |
|---|---|---|---|
| Genome Editing Tools | CRISPR/Cas9 systems; CRISPRi; Prime editors [18] | Functional validation of candidate genes in model organisms; creating synthetic genetic variants | Targeted gene knockout/knockin; gene expression modulation; precise nucleotide editing |
| Multi-Omics Profiling Kits | 16S rRNA sequencing; shotgun metagenomics; RNA-seq; metabolomics panels [18] | Comprehensive molecular profiling of resilient species; identification of protective signatures | Microbial community analysis; gene expression quantification; metabolic pathway mapping |
| Specialized Antibodies | Species-specific Nrf2/KEAP1 antibodies; phospho-specific insulin signaling antibodies [17] | Protein localization and quantification; pathway activation assessment in non-model species | Immunohistochemistry; Western blotting; ELISA; monitoring pathway activity states |
| Bioinformatic Tools | Comparative genomics pipelines; phylogenetic analysis software; pathway enrichment tools [17] | Evolutionary analysis; identification of positively selected genes; pathway conservation assessment | Genome sequence comparison; evolutionary relationship mapping; functional annotation |
| Cell Culture Models | Primary cells from disease-resistant species; organ-on-chip systems; induced pluripotent stem cells [18] | In vitro studies of cellular mechanisms; high-throughput compound screening | Functional assessment of cellular processes; predictive toxicology; therapeutic screening |
The systematic study of disease-resistant species provides unprecedented opportunities for biomedical innovation. As the field of evolutionary medicine matures, several key priorities emerge: First, expanding comparative physiology studies to include more diverse species, particularly those with exceptional resistance to specific human diseases like Alzheimer's, osteoporosis, or metastatic cancer. Second, developing better experimental models, including stable cell lines from resilient species and humanized animal models incorporating protective genes or pathways identified through biomimetic research. Finally, establishing robust validation frameworks that can efficiently translate observations from natural systems into targeted therapies.
The growing integration of biomimetic principles with advanced tools in genomics, bioengineering, and artificial intelligence promises to accelerate this translation [16] [18]. By treating nature as a validated discovery platform, researchers can access millions of years of evolutionary experimentation, potentially bypassing dead ends that might otherwise consume substantial resources in conventional drug development. This approach represents a paradigm shift—from fighting disease pathology to understanding and emulating natural solutions that have already evolved to prevent it.
The framework of life-history evolution provides a powerful lens for understanding human health and disease. Life-history theory explains how organisms allocate limited resources to competing functions—growth, reproduction, and maintenance—over their lifetimes [19]. These allocations inevitably involve evolutionary trade-offs where benefits in one domain incur costs in another [20] [21]. For biomedical researchers, recognizing that many disease vulnerabilities represent the downstream consequences of these deep evolutionary trade-offs offers transformative potential for understanding disease etiology, identifying novel therapeutic targets, and developing personalized treatment approaches. This guide examines key disease patterns emerging from life-history trade-offs, comparing their underlying mechanisms and experimental evidence to validate evolutionary medicine approaches.
Theoretical Framework: Life-History Trade-offs as Disease Drivers
Life-history theory posits that natural selection shapes how organisms parcel finite resources into competing biological functions [19]. The fundamental trade-offs between growth, reproduction, and maintenance processes create inherent vulnerabilities to disease when these evolved systems encounter modern environments or genetic variation [22].
Table 1: Fundamental Life-History Trade-offs and Their Disease Implications
| Trade-off Type | Physiological Basis | Resulting Disease Vulnerabilities | Evolutionary Benefit |
|---|---|---|---|
| Reproduction vs. Survival | Energetic costs of reproduction reduce investment in somatic maintenance [23] | Shorter lifespan, accelerated aging disorders | Maximizes lifetime reproductive output |
| Growth Rate vs. Longevity | Rapid growth can compromise tissue maintenance and repair [19] | Increased cancer risk, earlier senescence | Earlier maturation in high-mortality environments |
| Immune Function vs. Other Processes | Energetically costly immune responses reduce resources for other functions [20] | Autoimmunity vs. infectious disease susceptibility | Balanced protection against diverse pathogens |
| Early vs. Late Reproduction | Early maturation often correlates with shorter lifespan [19] | Age-related disease susceptibility in fast-life histories | Fitness advantage in unpredictable environments |
These trade-offs are maintained through several biological mechanisms. Antagonistic pleiotropy occurs when genes beneficial early in life become detrimental later in life [22] [20]. Competitive resource allocation creates physiological conflicts when limited resources must be distributed among competing systems [19]. The resulting disease patterns represent the costs of evolutionary optimizations for reproductive success rather than perfect health [22].
Comparative Analysis of Diametric Disease Patterns
Research reveals that evolutionary trade-offs often manifest as diametric disease patterns, where risk for one set of disorders inversely correlates with risk for opposing conditions [20]. The table below compares four clinically significant diametric disease pairs and their evolutionary underpinnings.
Table 2: Diametric Disease Patterns in Clinical Medicine
| Disease Pair | Proposed Evolutionary Trade-off | Genetic/Epidemiological Evidence | Potential Mechanisms |
|---|---|---|---|
| Autism Spectrum vs. Psychotic-Affective Disorders | Social cognition vs. non-social, mechanistic cognition [20] | Negative correlation in family risk; inverse cognitive profiles [20] | Brain development and connectivity trade-offs; empathizing-systemizing balance |
| Osteoarthritis vs. Osteoporosis | Bone mineral density vs. joint flexibility and repair capacity [20] | Inverse prevalence patterns in aging populations; genetic correlation studies | Trade-offs in bone remodeling processes; mesenchymal stem cell differentiation |
| Cancer vs. Neurodegenerative Disorders | Cell proliferation vs. cellular repair and maintenance systems [20] | Inverse comorbidity patterns; opposing genetic signatures in pathway analyses | Apoptosis regulation; DNA repair efficiency; metabolic allocation |
| Autoimmunity vs. Infectious Disease Susceptibility | Immune system reactivity and response intensity [20] | Genetic variants that protect against infection increase autoimmune risk (e.g., APOL1) [24] | Immunological memory formation; inflammatory response regulation; T-cell differentiation |
These diametric patterns provide natural experiments for identifying protective factors—understanding what reduces risk for one disorder directly informs what increases risk for its opposite [20]. For instance, the APOL1 gene variant that protects against African sleeping sickness simultaneously increases risk for kidney disease, demonstrating a clear evolutionary trade-off with significant clinical implications [24].
Experimental Approaches and Methodologies
Validating evolutionary trade-offs in human disease requires integrating multiple methodological approaches across biological scales and temporal dimensions.
Genomic and Molecular Techniques
- Comparative phylogenomics: Systematic mapping of disease vulnerability and resistance across diverse species identifies natural models of disease protection [5]. For example, studying cancer resistance in elephants and naked mole rats has revealed duplicated tumor suppressor genes and unique cellular mechanisms [24] [5].
- Pleiotropy mapping: Identifying genetic variants with opposing effects on different diseases through genome-wide association studies (GWAS) and Mendelian randomization [20]. The standard methodology involves analyzing large biobank data to detect negative genetic correlations between diametric diseases [20].
- Pathway analysis: Determining whether opposing diseases affect common biological pathways in reverse directions, using transcriptomic, proteomic, and metabolomic profiling [22].
Population-Level Studies
- Historical data analysis: Long-term genealogical records (e.g., Finnish church records dating to the 17th century) reveal genetic trade-offs such as the negative genetic correlation between birth interval and lifespan [23].
- Cross-population comparisons: Studying populations with different evolutionary histories exposes distinct disease risk patterns, such as the Polynesian allele that increases obesity risk while decreasing type II diabetes risk [24].
- Experimental evolution: Laboratory selection experiments in model organisms directly demonstrate life-history trade-offs, such as selection for extended lifespan in Drosophila leading to reduced early fecundity [19].
Research Framework for Evolutionary Trade-offs
Table 3: Key Research Reagent Solutions for Evolutionary Medicine Studies
| Resource Category | Specific Examples | Research Applications | Considerations |
|---|---|---|---|
| Genomic Databases | 100K Genomes Project [25], 1+Million Genomes Initiative [25], GWAS catalogues | Identifying pleiotropic variants, negative genetic correlations | Data access governance, population stratification |
| Model Organisms | Elephant cells (TP53 duplicates) [24] [5], Naked mole rat tissues (oxidative stress resistance) [24], Bat stem cells (longevity mechanisms) [24] | Studying natural disease resistance mechanisms | Cross-species translation validity |
| Computational Tools | Euler-Lotka equation models [19], Life table analysis [23], Phylogenetic comparative methods | Quantifying trade-offs, predicting evolutionary trajectories | Parameter estimation accuracy, model assumptions |
| Biobanks & Cohorts | Finnish church records [23], All of Us Precision Health Initiative [25], UK Biobank | Longitudinal studies of life-history traits, genetic trade-offs | Sample representativeness, data harmonization |
Signaling Pathways and Biological Mechanisms
The molecular architecture of life-history trade-offs involves several conserved signaling pathways that regulate resource allocation decisions. The diagram below illustrates the key pathways implicated in translating evolutionary trade-offs into disease susceptibility.
Pathway Mechanisms of Evolutionary Trade-offs
These pathways function as evolutionary sensors that interpret environmental cues and allocate resources accordingly. For example, the insulin/IGF-1 signaling (IIS) pathway responds to nutritional status and regulates the trade-off between reproduction and longevity [19]. The mTOR pathway integrates information about nutrient availability to balance anabolic growth processes against autophagy and cellular repair [22]. When these ancient systems encounter modern environments—chronic caloric abundance, reduced activity levels, novel dietary components—the resulting mismatches can manifest as increased disease susceptibility [22] [5].
The evolutionary medicine framework reveals that many disease vulnerabilities represent the costs of evolutionary optimizations for reproductive success rather than perfect health [22]. This perspective has profound implications for biomedical research and therapeutic development. First, diametric disease patterns provide natural experiments for identifying protective factors—understanding what reduces risk for one disorder directly informs what increases risk for its opposite [20]. Second, viewing diseases through the lens of evolutionary trade-offs highlights new prevention strategies that consider an individual's evolutionary trajectory and potential vulnerabilities [5]. Finally, the recognition that many modern pathologies represent evolutionary mismatches suggests that some interventions might focus on realigning modern environments with our evolved biology rather than targeting specific pathways with pharmaceuticals [22] [5].
The most promising future research directions include systematic mapping of disease vulnerability and resistance across the tree of life [5], developing evolutionary principles for controlling treatment resistance in cancers and infectious diseases [5], and applying life-history theory to understand patterns of disease burden across different populations and life stages [23] [19]. By integrating evolutionary perspectives with molecular medicine, researchers can develop more predictive models of disease risk and more effective, personalized interventions that account for our species' deep evolutionary history.
Relaxed Natural Selection and Its Impact on Contemporary Human Health
The framework of evolutionary medicine provides a powerful lens through which to view modern human health challenges. This review examines the growing body of evidence that relaxed natural selection—the reduction in mortality before reproductive age due to modern advancements—has facilitated the accumulation of deleterious genetic variants in human populations, contributing to increased prevalence of chronic diseases. We synthesize quantitative findings from global ecological studies, genomic analyses of founder populations, and evolutionary biology research to validate this paradigm. Supporting data are presented in structured comparative tables, alongside detailed experimental methodologies, visualized biological pathways, and essential research tools to equip investigators in this emerging field. The evidence confirms that relaxed selection operates through multiple mechanisms including reduced purifying selection, genetic drift, and altered trade-offs, with demonstrable impacts on obesity, recessive genetic disorders, and other contemporary health challenges.
Relaxed natural selection describes the phenomenon wherein advancements in modern medicine, public health, nutrition, and technology have reduced external environmental pressures that historically culled deleterious genetic variants from human populations [26]. When individuals who would have succumbed to selective pressures in ancestral environments survive and reproduce in modern settings, they perpetuate genetic variants that may predispose their descendants to various health conditions [27]. This process represents a fundamental evolutionary mismatch between our slowly adapting genome and rapidly changed environment [26] [28].
The Biological State Index (Ibs) has been developed as a quantitative measure of relaxed selection, calculating the probability that individuals survive to reproductive age based on mortality statistics [27]. Higher Ibs values indicate greater relaxation of selective pressures, enabling researchers to correlate this evolutionary force with health outcomes across populations. This framework transforms our understanding of disease etiology from purely mechanistic explanations to include evolutionary historical perspectives, potentially opening new avenues for therapeutic intervention through the identification of evolutionarily novel pathways contributing to disease susceptibility.
Quantitative Evidence: Global and Population Studies
Global Patterns of Obesity and Relaxed Selection
Table 1: Global Obesity Prevalence in Relation to Relaxed Selection [27]
| Analysis Method | Sex | Correlation with Ibs | Statistical Significance | Notes |
|---|---|---|---|---|
| Curvilinear regression | Male | Stronger positive correlation | P < 0.001 | 60% greater obesity prevalence gap between high/low Ibs countries |
| Curvilinear regression | Female | Significant positive correlation | P < 0.001 | Lesser effect than males |
| Partial correlation (controlled for GDP, urbanization, calories) | Male | Significant | P < 0.001 | Effect independent of confounders |
| Partial correlation (controlled for GDP, urbanization, calories) | Female | Significant | P < 0.001 | Effect independent of confounders |
| Multivariate regression R² increment | Male | Greater R² increase with Ibs addition | P < 0.01 | Ibs explains more variance in male obesity |
This comprehensive analysis of 191 countries revealed that relaxed selection contributes significantly to obesity prevalence worldwide, but with sex-based disparities. The stronger effect in males suggests that greater environmental and personal interventions in regulating female body mass may partially counteract the genetic predisposition [27]. The persistence of these correlations after controlling for economic and nutritional confounders strengthens the argument for a genuine evolutionary component in the global obesity pandemic.
Genetic Drift in Founder Populations
Table 2: Genetic Consequences of French Canadian Expansion [29]
| Genetic Parameter | Wave Front Population | Core Population | Statistical Significance | Generations to Emerge |
|---|---|---|---|---|
| New/low-frequency variants | Significantly more deleterious | Less deleterious | P < 0.05 | 6-9 generations |
| Equally deleterious mutations | Higher frequencies | Lower frequencies | P < 0.05 | 6-9 generations |
| Homozygosity for rare deleterious mutations | 2× higher probability | Baseline probability | P < 0.05 | 6-9 generations |
| Effective population size (Ne) | Lower | Higher | P < 0.05 | Modeling estimate |
| Recessive genetic diseases | Higher prevalence | Lower prevalence | Historically documented | - |
Genomic analysis of French Canadians, who underwent a range expansion in the 17th century, provides direct evidence of relaxed selection effects. The study compared descendants of settlers who lived on the expanding wave front with those whose ancestors remained in the settlement core, revealing that genetic drift on the wave front led to accelerated accumulation of deleterious variants [29]. This demonstrates how demographic processes, even without technological modernization, can relax selective pressures through similar mechanisms, and explains the higher prevalence of recessive genetic diseases in recently settled regions of Quebec.
Experimental Approaches and Methodologies
Ecological Study Design for Global Analysis
The protocol for examining relaxed selection across populations involves multifactorial data collection and advanced statistical modeling:
Data Acquisition: Gather country-level data on obesity prevalence from WHO databases, mortality statistics for Ibs calculation from demographic registries, and confounding variables (GDP, urbanization rates, caloric availability) from World Bank and FAO databases [27].
Ibs Calculation: Compute the Biological State Index using life table methods to estimate the probability of survival to reproductive age, standardized across populations.
Statistical Analysis:
- Perform curvilinear regression to model non-linear relationships between Ibs and health outcomes
- Conduct bivariate correlation analysis between Ibs and outcome variables
- Implement partial correlation controlling for economic and nutritional confounders
- Use Fisher r-to-z transformation to compare correlation strengths between subgroups
- Apply multivariate regression with stepwise model building to assess incremental predictive value of Ibs
- Utilize linear mixed models to account for hierarchical data structures
This methodology enables researchers to detect the signal of relaxed selection amidst numerous contemporary environmental factors influencing health outcomes.
Genomic Analysis of Historical Populations
The investigation of founder populations like French Canadians employs genealogical reconstruction and exome sequencing:
Genealogical Ascertainment: Construct extensive family trees using parish records, census data, and vital statistics to identify individuals with ancestors predominantly on the expansion wave front versus core settlement areas [29].
Sample Selection: Recruit contemporary descendants representing both historical groups, matching for known confounding factors.
Genomic Processing:
- Perform whole exome or genome sequencing
- Annotate variants using databases like gnomAD, ExAC, and ClinVar
- Predict variant deleteriousness with algorithms (PolyPhen-2, SIFT, CADD)
- Calculate allele frequencies within and between populations
- Estimate mutation load using burden tests
- Model effective population size through demographic inference
- Simulate allele frequency changes under different selection coefficients
This approach provides direct evidence of mutation accumulation resulting from relaxed selection over historical timescales.
Visualization of Key Concepts and Pathways
The Relaxed Selection Pathway in Modern Humans
Metabolic Trade-Offs in Aging and Disease
Essential Research Tools and Reagents
Table 3: Research Toolkit for Studying Relaxed Selection
| Tool/Resource | Type | Primary Application | Key Features |
|---|---|---|---|
| Ibs Calculation Algorithm | Analytical metric | Quantifying relaxed selection across populations | Incorporates mortality and reproductive age data; enables cross-population comparisons |
| gnomAD/ExAC Databases | Genomic reference | Determining variant rarity and predicted impact | Aggregates sequencing data from diverse populations; flags deleterious variants |
| Deleteriousness Prediction (CADD, SIFT) | Bioinformatics tools | Prioritizing potentially harmful genetic variants | Integrates multiple genomic features; evolutionary constraint metrics |
| Fixed Effects Likelihood Method | Statistical analysis | Detecting selection at specific codons | Identifies positive and purifying selection (α = 0.05) |
| Genealogical Reconstruction Software | Demographic tool | Tracing ancestral relationships in founder populations | Handles large pedigree data; identifies geographical settlement patterns |
| Population Genomic Simulators | Modeling software | Projecting allele frequency changes under different scenarios | Incorporates selection coefficients, drift, and demographic history |
The evidence from global ecological studies, founder population genetics, and evolutionary theory consistently demonstrates that relaxed natural selection represents a significant factor shaping contemporary human health profiles. The accumulation of deleterious variants due to reduced purifying selection, particularly in conjunction with novel environmental mismatches, contributes to the increasing prevalence of chronic diseases that plague modern societies [26] [27] [29].
These findings validate evolutionary medicine as an essential framework for understanding human disease etiology and present new opportunities for therapeutic development. Future research should focus on identifying specific genetic networks most susceptible to relaxed selection pressures, developing interventions that account for our evolutionary legacy, and exploring how modern medical practices might be optimized to work in concert with, rather than against, fundamental evolutionary principles. The tools and methodologies outlined herein provide a foundation for advancing this critical research frontier.
Applied Evolutionary Strategies: Methodologies and Therapeutic Innovations
The application of evolutionary principles to cancer treatment represents a paradigm shift in oncology, moving beyond the traditional goal of immediate tumor cell killing to a more nuanced management of eco-evolutionary dynamics within tumor ecosystems. This approach recognizes that cancer is a Darwinian process characterized by the selection and expansion of treatment-resistant clones [30] [31]. Evolutionary-informed therapies explicitly leverage principles from evolutionary biology and ecology to forestall or prevent the emergence of therapy resistance, thereby prolonging treatment efficacy and improving patient outcomes [32] [33]. The validation of these approaches rests on a growing body of evidence from mathematical modeling, preclinical studies, and emerging clinical trials that demonstrate their potential to outmaneuver cancer's evolutionary adaptations.
The fundamental premise of evolutionary medicine in oncology is that standard maximum tolerated dose (MTD) chemotherapy, while often producing initial tumor regression, inevitably selects for resistant cell populations that lead to disease progression [31]. In contrast, evolutionary therapies aim to control rather than eradicate cancer populations by maintaining a contingent of treatment-sensitive cells that can competitively suppress resistant populations [32] [34]. This framework encompasses several distinct strategies, primarily adaptive therapy and extinction therapy, which differ in their mechanisms, applications, and evidence base but share the common goal of manipulating cancer evolution for therapeutic benefit.
Comparative Analysis of Evolutionary Therapy Approaches
Table 1: Comparison of Major Evolution-Informed Cancer Therapy Approaches
| Therapeutic Approach | Core Principle | Key Mechanisms | Clinical Evidence | Advantages | Limitations |
|---|---|---|---|---|---|
| Adaptive Therapy | Maintain stable tumor volume by leveraging competition between sensitive and resistant cells | Dose modulation based on tumor burden; treatment holidays | Phase 2 trial in mCRPC: 33.5 vs. 14.3 months time to progression vs. standard care [32] | Reduces cumulative drug exposure; preserves quality of life; delays resistance | Requires frequent monitoring; dependent on reliable biomarkers; not curative |
| Extinction Therapy (Multi-Strike) | Exploit vulnerability of minimal residual disease to prevent evolutionary rescue | Sequential administration of distinct therapeutic agents at tumor nadir | Phase 2 trials ongoing for metastatic rhabdomyosarcoma, prostate cancer, and breast cancer [33] | Potential for cure; exploits collateral sensitivity | Optimal timing challenging; risk of under-treatment; limited clinical validation |
| Double-Bind Therapy | Force cancer cells into evolutionary traps where resistance to one treatment increases susceptibility to another | Concurrent or sequential administration of agents with collateral sensitivity | Preclinical validation; clinical trials in development [32] | Creates evolutionary dead-ends; suppresses resistance | Requires detailed knowledge of resistance mechanisms; drug combination screening needed |
Table 2: Quantitative Outcomes from Evolutionary Therapy Clinical Studies
| Cancer Type | Therapy Approach | Primary Endpoint | Result | Comparison to Standard Care | Study Reference |
|---|---|---|---|---|---|
| Metastatic Castrate-Resistant Prostate Cancer | Adaptive Therapy (dose modulation) | Time to Progression | 33.5 months | 14.3 months (134% increase) [32] | Moffitt Cancer Center Trial |
| Metastatic Castrate-Resistant Prostate Cancer | Adaptive Therapy (dose modulation) | Cumulative Drug Dose | 47% of standard dosing | 100% of standard dosing (53% reduction) [32] | Moffitt Cancer Center Trial |
| Locally Advanced Prostate Cancer | Evolutionary Metrics (genomic & morphological heterogeneity) | Prediction of Recurrence | HR = 3.12 (genomic), 2.24 (morphological) | Identified group with half the median time to recurrence [35] | IMRT Clinical Trial Analysis |
Experimental Protocols and Methodologies
Adaptive Therapy Clinical Protocol for Prostate Cancer
The most established clinical protocol for adaptive therapy comes from the Moffitt Cancer Center trial in metastatic castrate-resistant prostate cancer (mCRPC) [32]. This approach uses prostate-specific antigen (PSA) levels as a biomarker for tumor burden to guide treatment decisions.
Methodology:
- Initial Treatment Phase: Patients begin treatment with standard dosing (e.g., abiraterone acetate) until tumor burden (PSA) decreases by ≥50% from baseline.
- Treatment Holiday: Therapy is paused once the target reduction is achieved.
- Monitoring Phase: PSA levels are monitored regularly during the treatment break.
- Treatment Re-initiation: Therapy is resumed when PSA returns to baseline levels.
- Dose Modulation: Subsequent treatment cycles may use modified doses based on the patient's specific response pattern.
This protocol leverages competitive interactions between treatment-sensitive and resistant cancer cells. By maintaining a population of sensitive cells through intermittent therapy, the growth of resistant populations is suppressed through competition for resources and space [32]. The mathematical foundation for this approach originates from evolutionary game theory, which models the dynamics between different cell populations under therapeutic selection pressure [34].
Extinction Therapy (Multi-Strike) Protocol
Extinction therapy, also called multi-strike therapy, employs a different evolutionary principle based on evolutionary rescue theory [33]. This approach aims to eradicate cancer populations by exploiting their vulnerability when reduced to minimal size.
Methodology:
- First Strike: Application of initial therapy to reduce tumor population size and diversity.
- Monitoring for Nadir: Careful tracking of tumor burden to identify the point of maximum response.
- Second Strike: Administration of a distinct therapeutic agent when the tumor population is at or near its minimum size, before significant relapse occurs.
- Additional Strikes: Potential application of further distinct therapies for persistent populations.
The critical innovation in extinction therapy is the timing of the second strike. Mathematical modeling indicates that the optimal switch time to the second treatment is when the tumor is close to its minimum size, which may occur when it is clinically undetectable [33]. This timing exploits the demographic and genetic vulnerabilities of small populations, including reduced heterogeneity and increased susceptibility to stochastic extinction.
The theoretical foundation for this approach combines evolutionary rescue theory with stochastic population models. These models incorporate four cell types: sensitive to both treatments (S), resistant to one but sensitive to the other (R1, R2), and resistant to both (R1,2). The probability of tumor extinction is calculated based on the population composition at the time of treatment switching [33].
Signaling Pathways and Workflow Diagrams
Evolutionary Therapy Decision Pathway
Eco-Evolutionary Dynamics in Cancer Therapy
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Tools for Evolutionary Therapy Investigations
| Research Tool | Primary Function | Application in Evolutionary Therapy | Key Features |
|---|---|---|---|
| Circulating Tumor DNA (ctDNA) Analysis | Monitoring tumor burden and clonal dynamics | Tracking emergence of resistant clones; guiding therapy switches | Non-invasive; provides real-time evolutionary information [36] |
| Single-Cell Sequencing | Resolution of intratumor heterogeneity | Identifying rare resistant subpopulations; understanding clonal architecture | Reveals subclonal mutations and phenotypic plasticity [36] [35] |
| Spatial Transcriptomics | Mapping gene expression in tissue context | Understanding tumor microenvironment interactions; spatial clustering of clones | Preserves architectural information; identifies ecological niches [36] |
| AI-Aided Computational Histopathology | Quantifying morphological heterogeneity | Predicting recurrence from H&E slides; integration with genomic data | Leverages existing clinical samples; powerful prognostic value [35] |
| Immuno-PCR (Imperacer) | Ultra-sensitive biomarker detection | Monitoring minimal residual disease; pharmacokinetic studies | Detect limits in sub-pg/ml range; 1000x sensitivity vs. ELISA [37] |
| Stochastic Mathematical Models | Predicting evolutionary dynamics | Optimizing treatment scheduling; modeling extinction probabilities | Incorporates environmental stochasticity; enables risk-aware therapy [34] |
Discussion: Validation and Clinical Translation
The validation of evolution-informed cancer therapies represents an emerging paradigm that integrates quantitative evolutionary metrics with clinical oncology practice. Key validation milestones include the demonstration that measures of intratumor heterogeneity—both genomic and morphological—serve as powerful predictors of recurrence risk in prostate cancer [35], and that adaptive therapy protocols can significantly extend progression-free survival while reducing cumulative drug exposure in metastatic castration-resistant prostate cancer [32].
The clinical translation of these approaches faces several challenges, including the need for frequent monitoring, identification of reliable biomarkers for different cancer types, and the cultural shift required for clinicians to embrace treatment strategies that explicitly control rather than aggressively reduce tumor burden [32]. Furthermore, the optimal scheduling of evolutionary therapies requires sophisticated mathematical modeling to account for the stochastic nature of cancer evolution [34]. The emerging generation of "threshold-aware" treatment policies aims to maximize the probability of achieving therapeutic goals while respecting constraints on cumulative treatment burden [34].
Future directions in evolutionary cancer therapy include the refinement of multi-strike extinction protocols [33], the development of double-bind therapies that create evolutionary traps for cancer cells [32], and the integration of evolutionary principles with immunotherapy, targeted therapy, and antibody-drug conjugates [36]. The systematic mapping of collateral sensitivity networks—which identify how resistance to one drug increases susceptibility to another—represents a particularly promising avenue for designing evolution-based combination therapies.
As evolutionary medicine continues to validate its approaches across biomedical disciplines [38], cancer treatment stands to benefit substantially from this perspective. The recognition that cancer is fundamentally an evolutionary and ecological process provides not only explanatory power for its relentless progression but also a strategic framework for its more effective management.
Combating Antimicrobial Resistance Through Evolutionary Principles
Antimicrobial resistance (AMR) represents one of the most pressing global health challenges of our time, with treatment-resistant infections causing at least one million deaths worldwide annually [39]. The conventional approach to combating AMR has primarily focused on developing new antimicrobial compounds. However, this strategy has proven insufficient against the relentless pace of bacterial evolution. Evolutionary medicine offers a transformative framework by leveraging the fundamental principles of evolution itself to outmaneuver resistance mechanisms. This approach recognizes that resistance evolution follows predictable patterns influenced by evolutionary trade-offs, mutational biases, and selective pressures that can be strategically exploited [40] [41]. By shifting the paradigm from reactive drug development to evolution-informed therapeutic design, researchers are developing innovative strategies that anticipate and circumvent resistance pathways, potentially extending the lifespan of existing antibiotics and restoring their efficacy against resistant pathogens.
Evolutionary Trade-offs: Exploiting Bacterial Vulnerabilities
The Fitness Cost of Resistance
A fundamental principle in evolutionary medicine is that resistance mutations often impose fitness costs on bacteria in the absence of antibiotics. These evolutionary trade-offs create vulnerabilities that can be strategically exploited. Research using the Soft Agar Gradient Evolution (SAGE) platform has demonstrated that chloramphenicol-resistant Escherichia coli mutants exhibit markedly reduced rates of resistance evolution against other antibiotics [40]. This phenomenon, known as collateral sensitivity, occurs when resistance to one antibiotic concurrently increases sensitivity to another unrelated drug. The SAGE platform, enhanced with xanthan gum to reduce synaeresis of agar-based medium, provides a clinically relevant environment for mapping these evolutionary trade-offs and identifying optimal drug sequences that constrain resistance evolution [40].
Table 1: Key Evolutionary Concepts in AMR Mitigation
| Evolutionary Concept | Mechanism | Therapeutic Application |
|---|---|---|
| Collateral Sensitivity | Resistance to drug A increases sensitivity to drug B | Sequential therapy cycling |
| Fitness Cost Compensation | Mutations that restore fitness often reduce resistance | Extended treatment to allow compensatory evolution |
| Evolutionary Trade-offs | Genetic changes enabling survival in one environment reduce fitness in another | Multi-drug regimens targeting conflicting adaptations |
| Mutational Bias | Resistance pathways influenced by nucleotide substitution probabilities | Drug design targeting least probable resistance mutations |
Tripartite Loops: Containing Resistance Through Evolutionary Traps
The most promising approach leveraging evolutionary trade-offs involves tripartite loops—sequential antibiotic regimens composed of three drugs arranged in a closed cycle. Through 424 discrete adaptive laboratory evolution experiments, researchers have demonstrated that as bacteria sequentially evolve resistance to each drug in a tripartite loop, they continually trade past resistance for fitness gains, reverting back to sensitivity through 4-8-fold reductions in resistance on average [40]. This strategic cycling guides bacterial populations along evolutionary paths that mitigate fitness costs while reversing resistance to component drugs, achieving resensitization levels not attainable through previously suggested pairwise regimens. Notably, this approach has proven effective at resensitizing or eradicating multidrug-resistant clinical isolates, even when adaptation occurred through plasmid-bound mutations rather than chromosomal changes, demonstrating the robustness of this evolutionary containment strategy [40].
Plasmid Epidemiology: Targeting the Vectors of Resistance
Historical Mapping of Resistance Spread
The evolutionary journey of AMR cannot be fully understood without examining the role of plasmids—transferable genetic structures that enable different bacterial strains to share resistance genes. Groundbreaking research analyzing over 40,000 plasmids from historical and present-day bacterial samples across six continents has revealed how a minority of plasmids has driven most multidrug resistance worldwide [39]. By examining bacterial samples dating back to 1917 (pre-antibiotic era), researchers determined that ancestral plasmids initially lacked resistance genes but evolved to acquire them as antibiotic use expanded. The descendants of these plasmids now confer resistance to both first-line and last-resort antibiotics, representing a critical threat to global health [39].
Table 2: Plasmid Evolutionary Pathways and AMR Implications
| Evolutionary Pathway | Genetic Mechanism | Clinical Significance |
|---|---|---|
| AMR Gene Insertion | Resistance genes inserted into existing plasmid structure | Creates specialized resistance carriers within bacterial species |
| Plasmid Fusion | Combination of multiple plasmids into new genetic structures | Produces highly transferable multidrug resistance vectors across species |
| Fragment Recycling | Genetic fragments from degraded plasmids incorporated into chromosomes | Stabilizes resistance in bacterial genomes without plasmid maintenance |
| Vertical Evolution | Gradual accumulation of mutations in existing plasmid framework | Allows fine-tuning of resistance mechanisms to specific antibiotic pressures |
Predictive Modeling of Plasmid Evolution
The analysis of 100 years of bacterial evolution has enabled researchers to develop models that predict plasmid evolutionary trajectories [39]. These models identify three distinct pathways: slow-changing plasmids, plasmids that completely merge with others, and those that disappear while leaving genetic fragments that are subsequently "recycled." The modern plasmids containing multidrug resistance genes emerged primarily through two pathways: either through insertion of AMR genes into existing plasmid structures, or through fusion with other plasmids. The fusion-derived plasmids demonstrate particularly high transferability between different bacterial species, making them especially effective at disseminating resistance across microbial communities. This predictive understanding of plasmid evolution opens possibilities for developing rational approaches to target the spread of antibiotic resistance genes, potentially through CRISPR-based technologies or other molecular interventions that specifically disrupt these key vectors [39].
Evolutionary Informatics in Drug Design
Multiobjective Optimization in Antimicrobial Development
The complex challenge of designing effective antimicrobials requires balancing multiple, often competing objectives including potency, selectivity, safety, and evolutionarily-informed resistance management. Multiobjective evolutionary graph algorithms (MEGA) represent a computational framework that addresses this complexity by combining evolutionary techniques with graph theory to directly manipulate molecular structures and identify optimal compromises between conflicting design criteria [42] [43]. Unlike traditional de novo design focused on single objectives like similarity to known ligands, MEGA simultaneously optimizes for multiple predefined objectives, generating structurally diverse candidate molecules representing a wide range of compromises between supplied constraints [43]. This approach serves as an "idea generator" for medicinal chemists, enabling systematic exploration of chemical space to identify compounds with enhanced potential to circumvent resistance mechanisms while maintaining favorable pharmacological properties.
Mutation-Biased Drug Design
Quantitative analysis of resistance evolution reveals that mutational biases significantly influence which resistance variants dominate in clinical settings. Research across multiple cancer types (prostate cancer, breast cancer, and gastrointestinal stromal tumors) suggests that resistance evolution in the adjuvant setting is strongly influenced by mutation probability rather than solely by fitness advantages [41]. This insight establishes a crucial principle for rational drug design: when evolution favors the most probable mutant, so should drug discovery. In practice, this means prioritizing drug candidates that target residues where resistance mutations require unlikely nucleotide substitutions (transversions rather than transitions), or designing combination therapies that specifically preempt the most probable evolutionary escape paths [41]. First-principle models parameterized on large in vitro datasets can accurately predict the epidemiological abundance of resistance mutations, enabling proactive design of next-generation inhibitors that account for evolutionary trajectories before clinical resistance data matures [41].
Comparative Experimental Platforms for AMR Research
Methodologies for Evolutionary AMR Studies
Diagram: Experimental Platforms in Evolutionary AMR Research. The diagram illustrates the methodological approaches and key findings from major study types investigating evolution-based antimicrobial resistance strategies.
Table 3: Key Research Reagents and Platforms for Evolutionary AMR Studies
| Research Tool | Function | Application in Evolutionary AMR |
|---|---|---|
| SAGE Platform | Soft Agar Gradient Evolution system | Large-scale experimental evolution to map resistance trade-offs |
| Xanthan Gum Supplement | Water-binding polysaccharide | Reduces synaeresis in agar media, improving SAGE reliability |
| Historical Bacterial Collections | Biobanks of clinical isolates spanning decades | Tracking plasmid evolution and resistance gene acquisition |
| Bayesian Logistic Regression | Statistical modeling approach | Analyzing temporal trends in resistance patterns across settings |
| Multiobjective Evolutionary Graph Algorithm | Computational drug design framework | Designing molecules balancing potency with resistance management |
Comparative Analysis of Evolutionary Approaches
Quantitative Outcomes of Evolution-Informed Strategies
The effectiveness of evolution-based approaches is demonstrated through robust experimental data across multiple research platforms. These strategies generally outperform conventional approaches that focus solely on immediate bactericidal activity without accounting for evolutionary trajectories.
Table 4: Performance Comparison of Evolution-Informed AMR Strategies
| Therapeutic Strategy | Resistance Mitigation | Resensitization Potential | Clinical Validation |
|---|---|---|---|
| Tripartite Drug Loops | 4-8 fold resistance reduction | High (reversion to sensitivity) | Preclinical (MDR clinical isolates) |
| Plasmid-Targeted Approaches | Prevents horizontal transfer | Variable | Modeling phase |
| Collateral Sensitivity Cycling | Delays resistance emergence | Moderate (2-fold average) | Laboratory evolution confirmed |
| Mutation-Biased Drug Design | Reduces most likely escapes | Low (prevents rather than reverses) | Cancer clinical trials |
| Conventional Single-Drug Therapy | Rapid resistance emergence | None | Widespread treatment failure |
One Health Perspectives: Interspecies AMR Transmission
The evolutionary dynamics of AMR extend beyond human medicine to encompass animal and environmental reservoirs. A comparative study investigating temporal trends of antimicrobial resistance at both human (East Alabama Medical Center) and animal (Auburn University Veterinary Teaching Hospital) hospitals within the same community from 2010-2022 revealed complex patterns of resistance evolution [44]. While general AMR trends did not align between the two settings—showing decreasing susceptibility in the human hospital and increasing susceptibility in the animal hospital—specific combinations like Klebsiella pneumoniae susceptibility to gentamicin showed parallel patterns [44]. This research highlights the importance of integrated surveillance and the potential for cross-species transmission of resistance mechanisms in shared environments. Bayesian logistic regression applied to these datasets provides powerful modeling approaches for identifying when human and animal resistance patterns diverge or converge, offering insights for targeted interventions at the human-animal interface [44].
The accumulating evidence from diverse research platforms demonstrates that evolutionary principles provide powerful frameworks for combating antimicrobial resistance. Strategies that exploit fundamental evolutionary constraints—including tripartite drug loops that create evolutionary traps, approaches that target high-risk plasmid vectors, and mutation-biased drug design that preempts the most probable resistance pathways—offer promising alternatives to conventional antimicrobial development. As the antibiotic discovery pipeline continues to lag behind resistance evolution, these evolution-informed approaches may be essential for extending the clinical lifespan of existing antibiotics and managing the inevitable emergence of resistance. The integration of evolutionary theory, experimental evolution platforms, and computational modeling represents a transformative approach to addressing one of the most significant challenges in modern medicine, potentially restoring the efficacy of our antimicrobial arsenal through strategic manipulation of evolutionary trajectories.
The escalating crisis of antimicrobial resistance (AMR) has necessitated a paradigm shift in our approach to combating bacterial infections. Within this context, phage therapy—the use of bacteriophages (viruses that infect and lyse bacteria) to treat bacterial infections—has re-emerged as a potent alternative. Its resurgence is intrinsically linked to the core principles of evolutionary medicine, a field that applies insights from evolution and ecology to biomedicine [5] [24]. This framework recasts the challenge of bacterial infections not just as a static biochemical problem, but as a dynamic evolutionary arms race. Phage therapy uniquely leverages the relentless co-evolution between phages and their bacterial hosts, transforming a natural predatory relationship into a therapeutic strategy [45]. Unlike broad-spectrum antibiotics, which exert unselective pressure and drive resistance, phages can be deployed as precision tools that evolve in tandem with their targets. This review will objectively compare phage therapy's performance against standard antibiotics and other alternatives, presenting supporting experimental data and detailed methodologies to validate its role within the evolutionary medicine paradigm for researchers and drug development professionals.
The Co-evolutionary Arms Race: Mechanisms of Action and Bacterial Countermeasures
The therapeutic efficacy of phages stems from their sophisticated, evolutionarily honed life cycle. A foundational understanding of this mechanism is crucial for appreciating their clinical application and the inevitable bacterial counter-resistance that informs treatment design.
The Lytic Cycle and Biofilm Disruption
The primary therapeutic mechanism involves the lytic cycle [45] [46]. This process begins with the phage's highly specific attachment to bacterial surface receptors (e.g., efflux pumps, lipopolysaccharides, type-IV pili) [47] [46]. Following attachment, the phage injects its genetic material into the cell, hijacking the host's machinery to replicate its own components. These components are then assembled into new virions, culminating in the lysis (bursting) of the bacterial cell and the release of progeny phages to infect neighboring cells [45]. This self-amplifying nature makes phages a dynamic, "living" therapeutic that concentrates at the site of infection. A critical advantage over antibiotics is their ability to penetrate and disrupt biofilms [45] [46]. These structured bacterial communities, encased in a protective extracellular matrix, are notoriously resistant to conventional antibiotics. Phages overcome this by producing enzymes, such as depolymerases, which degrade the biofilm matrix, weakening its structure and increasing bacterial susceptibility to lysis and concomitant antibiotics [45] [46].
Evolutionary Trade-offs and Phage-Antibiotic Synergy (PAS)
A cornerstone of the evolutionary medicine approach is the strategic exploitation of evolutionary trade-offs. When bacteria evolve resistance to a phage—often by mutating or losing the surface receptor the phage uses for attachment—this adaptation can come at a significant fitness cost [47]. For instance, if the phage receptor is also involved in antibiotic resistance or virulence, bacterial survival against the phage may lead to resensitization to antibiotics or attenuated virulence [47] [46]. This phenomenon is graphically represented in the diagram below, which illustrates the core co-evolutionary logic of modern phage therapy.
This trade-off is central to Phage-Antibiotic Synergy (PAS), where the combined use of phages and antibiotics results in enhanced bacterial clearance. PAS operates through dual mechanisms: phages directly lyse bacteria and select for resistant mutants with compromised defenses, while sub-inhibitory concentrations of certain antibiotics can, in turn, enhance phage replication by stressing the bacterial host [45] [46]. The diagram below maps the dynamic feedback loops that make this combination more effective than either agent alone.
Comparative Performance Data: Phage Therapy vs. Standard of Care
While large-scale Phase III trials are ongoing, a growing body of clinical evidence from compassionate-use cases and smaller studies demonstrates the potential of phage therapy. The data below compare its performance against standard antibiotic treatments, particularly in complex, drug-resistant infections.
Table 1: Clinical Outcomes of Phage Therapy for Multidrug-Resistant Infections
| Infection Type / Study | Pathogen | Therapy Comparison | Key Efficacy Outcomes | Reference |
|---|---|---|---|---|
| Cystic Fibrosis (Compassionate use, n=9) | Pseudomonas aeruginosa (MDR/PDR) | Personalized inhaled phage therapy + antibiotics vs. prior antibiotics alone | ↓ Median 104 CFU/mL in sputum density post-therapy; ↑ 6-8% in predicted FEV1 (lung function) | [47] |
| Periprosthetic Joint Infection (Prospective, n=23) | Mixed (e.g., MRSA, P. aeruginosa) | Phage therapy (adjunct) + antibiotics vs. antibiotics alone (historical control) | PJI relapse rate was 8x higher in the control group at 1-year follow-up | [45] |
| Respiratory, Soft Tissue & Osteoarticular (Cohort, n=100) | Various ESKAPE pathogens | Phage-Antibiotic Combination vs. Phage Monotherapy | Combination therapy showed 70% superior eradication rates vs. monotherapy | [46] |
| Historical Clinical Trials (Meta-analysis) | Various | Phage Therapy (1921-1940) vs. Standard of Care (then) | Effective therapy: OR = 0.21, 95% CI = 0.10 to 0.44, P < 0.0001 | [48] |
Table 2: Comparison of Phage Therapy and Antibiotics Core Characteristics
| Characteristic | Phage Therapy | Traditional Antibiotics |
|---|---|---|
| Specificity | High (strain- or species-level); preserves commensal microbiome | Broad-spectrum; disrupts commensal microbiome |
| Mechanism of Action | Lytic infection; biofilm disruption; can leverage evolutionary trade-offs | Biochemical inhibition (e.g., cell wall synthesis, protein translation) |
| Self-Replication | Yes (at infection site); dose adjusts dynamically | No (fixed pharmacokinetic profile) |
| Resistance Development | Inevitable but can be managed via cocktails and leveraged for trade-offs | Inevitable and often confers broader resistance |
| Primary Challenge | Narrow host range requires personalization; complex regulation | Toxicity and collateral damage to microbiome driving AMR crisis |
Experimental Protocols: Validating Efficacy and Leveraging Trade-offs
For research and development, standardized protocols are essential for the rigorous evaluation of phage therapy. The following methodology details a personalized, trade-off-driven approach, as used in a recent clinical study for cystic fibrosis [47].
Workflow for Personalized Phage Selection
The overall process, from bacterial isolation to treatment and monitoring, is a multi-stage endeavor that requires close integration between clinical and laboratory functions, as visualized in the workflow below.
Detailed Methodologies
1. Clinical Isolate Collection and Bacteriophage Sourcing:
- Bacterial Isolation: Collect a clinical bacterial isolate from the patient (e.g., from sputum, tissue, or blood). Culture the isolate on appropriate agar plates to obtain pure colonies.
- Phage Library: Screen the isolate against a pre-existing library of characterized lytic phages. Alternatively, isolate new environmental phages from suitable sources like wastewater, filtering and enriching them using the patient's bacterial strain.
2. Phage Susceptibility and Characterization:
- Plaque Assay: Use a double-layer agar technique to confirm phage susceptibility. A clear zone (plaque) in the bacterial lawn indicates lytic activity and allows for the isolation of a pure phage stock.
- Host Range Determination: Test the phage against a panel of genetically diverse bacterial strains to determine the breadth of its lytic activity.
- Genomic Sequencing: Perform whole-genome sequencing of the phage to confirm the absence of genes encoding toxins, virulence factors, or lysogeny regulators (assuring a strictly lytic life cycle) [47] [46].
3. In vitro Assessment of Evolutionary Trade-offs:
- Experimental Evolution: Co-culture the bacterial isolate with the selected phage(s) over multiple generations to drive the evolution of phage resistance.
- Phenotypic Screening: Isolate phage-resistant bacterial mutants and screen them for changes in key pathogenicity traits.
- Antibiotic Resensitization: Perform antibiotic susceptibility testing (e.g., broth microdilution) to check for decreased Minimum Inhibitory Concentrations (MICs), especially if the phage targets a receptor like an efflux pump [47].
- Virulence Attenuation: Assess changes in virulence traits, for example, through motility assays (if the phage targets flagella), biofilm formation assays, or cytotoxicity tests in cell culture [47].
4. Preclinical In Vivo Validation:
- Utilize an appropriate animal model of infection (e.g., a mouse lung infection model for CF or a soft tissue infection model).
- Compare treatment arms: (a) Untreated control, (b) Antibiotic alone, (c) Phage alone, (d) Phage-Antibiotic combination.
- Primary endpoints typically include bacterial load (CFU/organ), host survival, and markers of inflammation [46].
The Scientist's Toolkit: Essential Research Reagents and Solutions
Translating phage therapy from concept to clinic requires a specific set of reagents and tools. The following table details key materials essential for conducting the experiments described in the protocols above.
Table 3: Essential Research Reagents for Phage Therapy Development
| Research Reagent / Material | Critical Function | Application in Protocol |
|---|---|---|
| Lytic Phage Library | Collection of characterized, strictly lytic bacteriophages; the core therapeutic agent. | Phage susceptibility screening (Step 2) and cocktail formulation (Step 4). |
| Bacterial Strain Panels | Diverse, clinically relevant strains for determining phage host range and specificity. | Host range determination and validation of cocktail coverage (Step 2). |
| Cell Culture Models | (e.g., human lung epithelial cells). Models for assessing cytotoxicity and virulence attenuation. | In vitro assessment of phage-driven virulence trade-offs (Step 3). |
| Animal Infection Models | (e.g., murine, Galleria mellonella). Systems for evaluating treatment safety and efficacy in a living host. | Preclinical validation of phage and phage-antibiotic synergy (Step 5). |
| Next-Generation Sequencing (NGS) | Platform for whole-genome sequencing of phages and bacterial isolates. | Phage genomic safety screening (Step 2) and tracking bacterial genomic evolution during therapy (Step 7). |
Discussion and Future Directions within Evolutionary Medicine
The data and methodologies presented validate phage therapy as a powerful, evolutionarily-informed intervention. Its superior performance in specific, challenging clinical scenarios—such as reducing bacterial load in PDR infections where antibiotics have failed—highlights its potential [47]. The ability to be combined with antibiotics to yield superior outcomes through PAS is a significant advantage over many monotherapy alternatives [45] [46].
From an evolutionary medicine perspective, phage therapy's greatest strength is its dynamic nature. It treats infection not as a static state but as an evolving ecosystem, using bacterial defense mechanisms against themselves via trade-offs. This stands in stark contrast to the static, "one-size-fits-all" model of traditional antibiotics, which inevitably selects for resistance without recourse.
Future development will focus on overcoming current limitations, such as narrow host range and the logistical challenges of personalization. Key areas of innovation include:
- AI-Driven Phage Optimization: Using machine learning to predict optimal phage cocktails and identify receptors linked to desirable trade-offs [46].
- Genetic Engineering: Precisely modifying phages to expand host range, enhance lytic activity, or deliver sensitizing genes to bacteria [46].
- Standardized Pharmacokinetics: Developing robust models to understand phage distribution, dosing, and dynamics within the human body [45] [46].
In conclusion, phage therapy exemplifies the transformative potential of evolutionary medicine. By consciously leveraging the ancient, co-evolutionary arms race between bacteria and viruses, it offers a path to outmaneuver antimicrobial resistance. For researchers and drug developers, it represents a paradigm shift from broad-spectrum suppression to targeted, intelligent ecological management of infections.
The integration of pharmacogenomics into clinical practice represents a paradigm shift from reactive to preemptive medicine, leveraging individual genetic profiles to optimize therapeutic outcomes. This review comprehensively compares current pharmacogenomic methodologies, analyzing their performance in predicting drug metabolism, efficacy, and adverse reactions. We evaluate established and emerging technologies—from targeted genotyping to artificial intelligence-driven approaches—within an evolutionary framework that explains how human genetic diversity shapes therapeutic responses. Supported by experimental data and detailed protocols, this analysis provides researchers and drug development professionals with validated frameworks for implementing precision medicine strategies that account for ancestral genetic variations. The synthesis of evolutionary history with cutting-edge pharmacogenomic technologies illuminates pathways toward truly personalized treatment regimens across diverse populations.
Pharmacogenomics has emerged as a cornerstone of precision medicine, investigating how genetic variation influences individual responses to medications. The genetic basis for variable drug responses stems from evolutionary processes that have shaped human populations over millennia. Genetic polymorphisms in drug-metabolizing enzymes, transporters, and targets represent adaptations to diverse environmental pressures, diets, and pathogen exposures across geographical regions [49]. These evolutionarily-derived variations now manifest clinically as differences in drug efficacy and safety profiles among populations.
The clinical imperative for pharmacogenomics is substantial. Adverse drug reactions (ADRs) constitute a major cause of hospitalization and mortality worldwide, with 15-30% of individual drug response variability attributable to genetic polymorphisms [50]. Notably, >95% of individuals carry at least one actionable pharmacogenetic variant when tested across a panel of 12 genes, making pharmacogenomic profiling universally relevant [50]. The field has progressively evolved from single-gene analysis toward comprehensive approaches that mirror the polygenic nature of most drug responses, enabling more accurate prediction of therapeutic outcomes.
This review systematically compares current pharmacogenomic methodologies, assessing their technical performance, clinical utility, and evolutionary relevance. By examining the experimental evidence supporting each approach and detailing essential research protocols, we provide a foundation for advancing personalized treatment regimens rooted in evolutionary medicine principles.
Comparative Analysis of Pharmacogenomic Methodologies
Technology Performance Comparison
Table 1: Comparison of Major Pharmacogenomic Testing Methodologies
| Methodology | Genetic Variants Detected | Throughput | Cost Considerations | Clinical Implementation Stage | Key Limitations |
|---|---|---|---|---|---|
| Targeted Array-Based Genotyping (e.g., DMET Plus) [51] | Pre-selected SNPs (1,936 markers in DMET); focused on ADME genes | Moderate | Lower cost for targeted approach | Widespread in clinical implementation studies | Limited to known variants; cannot discover novel variants |
| Next-Generation Sequencing (Short-read) [51] | SNPs, CNVs, insertions, deletions across entire genome | High | Decreasing cost; still substantial for whole-genome | Growing implementation for comprehensive profiling | Misses complex structural variations in pharmacogenes |
| Long-Read Sequencing (e.g., Nanopore, PacBio) [52] | Full haplotype phasing, structural variants, complex alleles (e.g., CYP2D6 hybrids) | Increasingly high | Higher per-sample but decreasing | Emerging for challenging pharmacogenes | Higher error rate requiring computational correction |
| Preemptive Panel Testing (e.g., PREDICT, PG4KDS) [53] | Multiple high-evidence pharmacogenes (CYP450, TPMT, DPYD, etc.) | High for targeted panels | Cost-effective through avoided adverse events | Advanced implementation at major centers | Limited gene selection; requires periodic updates |
Clinical Utility and Population Impact
Table 2: Clinical and Economic Outcomes of Pharmacogenomic Implementation
| Implementation Model | Patient Population | Key Outcomes | Economic Impact | Evidence Level |
|---|---|---|---|---|
| Pharmacist-Led Medication Therapy Management (YouScript) [50] | Elderly patients with polypharmacy (mean 11.6 medications) | Significant reduction in medication-related problems | Estimated annual saving of €549 ($621) per tested patient [53] | Multiple randomized trials |
| Preemptive Panel-Based Testing (Vanderbilt PREDICT) [53] | >10,000 patients with diverse conditions | 91% of patients had ≥1 actionable variant; 65% exposed to PGx drugs | Avoided 14,656 single genetic tests through preemptive panel | Large-scale implementation study |
| DPYD Genotyping for Fluoropyrimidine Toxicity Prevention [53] | Cancer patients receiving 5-fluorouracil or capecitabine | Reduced severe toxicity from historical controls | Cost savings of €916.77 ($1035.60) per patient on medication costs [53] | Controlled clinical studies |
| CYP2C19-Guided Antiplatelet Therapy [49] | PCI patients receiving clopidogrel | Reduced cardiovascular events in poor metabolizers | Favorable cost-effectiveness profile | CPIC Guideline implementation |
Key Experimental Protocols in Pharmacogenomics Research
Protocol 1: Comprehensive ADME Genotyping Using Microarray Technology
Background: The DMET (Drug Metabolism Enzymes and Transporters) Plus microarray platform interrogates 1,936 genetic markers across 231 genes involved in drug absorption, distribution, metabolism, and excretion (ADME) [51]. This targeted approach provides comprehensive coverage of clinically relevant pharmacogenetic variants with established roles in drug response variability.
Methodology:
- DNA Extraction and Quality Control: Isolate genomic DNA from whole blood or saliva samples, quantifying purity via spectrophotometry (A260/A280 ratio ≥1.8).
- Sample Amplification and Fragmentation: Amplify 750ng of genomic DNA followed by enzymatic fragmentation to optimal size distribution.
- Array Hybridization: Apply fragmented DNA to DMET Plus Array and incubate for 16 hours at 45°C with specific hybridization conditions.
- Washing and Staining: Perform automated washing followed by antibody-mediated staining using the GeneChip Fluidics Station 450.
- Scanning and Data Acquisition: Scan arrays using the GeneChip Scanner 3000 with 1.56μm resolution.
- Genotype Calling: Process raw data using DMET Console Software with reference to predefined genotype clusters.
Bioinformatic Analysis Pipeline [51]:
- Raw Data Processing: Convert CEL files to genotype calls using DMET Console Software
- Quality Filtering: Remove samples with call rates <95% and variants with Hardy-Weinberg equilibrium p-value <0.001
- Annotation: Annotate variants using PharmGKB, CPIC, and DPWG databases
- Phenotype Prediction: Translate genotypes to predicted phenotypes (e.g., poor, intermediate, extensive, or ultrarapid metabolizer)
- Clinical Interpretation: Apply CPIC or DPWG guidelines to generate prescribing recommendations
Validation: Confirm novel or clinically critical variants using Sanger sequencing or orthogonal genotyping methods.
Protocol 2: Long-Read Sequencing for Complex Pharmacogene Characterization
Background: Long-read sequencing technologies from Oxford Nanopore and Pacific Biosciences enable complete characterization of complex pharmacogenes like CYP2D6, which contains numerous structural variations, hybrid alleles, and copy number variations that challenge short-read technologies [52].
Methodology:
- DNA Extraction and Size Selection: Isolate high-molecular-weight DNA (>50kb) using magnetic bead-based methods, minimizing mechanical shearing.
- Library Preparation: Employ ligation sequencing kit with unique barcoding for multiplexed samples.
- Sequencing: Load libraries onto PromethION or Sequel II flow cells, achieving >30x coverage of target regions.
- Variant Calling and Haplotype Phasing:
- Perform base calling and read alignment to reference genome
- Identify structural variants using specialized tools (e.g., Sniffles, PBSV)
- Phase haplotypes using read-based phasing algorithms
- Star Allele Assignment: Assign star alleles using specialized bioinformatic tools (e.g., Aldy, Stargazer) that consider combinations of variants, structural variations, and copy number.
Applications: This protocol is particularly valuable for accurately genotyping highly polymorphic genes critical for drug metabolism, including CYP2D6, CYP2A6, and UGT2B17, which frequently contain structural variations that alter enzyme activity.
Visualizing Pharmacogenomic Pathways and Workflows
Drug Metabolism Pathway Integration
Pharmacogenomic Research Workflow
Table 3: Essential Research Resources for Pharmacogenomic Studies
| Resource Category | Specific Examples | Key Features & Applications | Access Information |
|---|---|---|---|
| Genotyping Platforms | DMET Plus Array [51] | Interrogates 1,936 markers across 231 ADME genes; standardized workflow | Commercial platform (Thermo Fisher Scientific) |
| Bioinformatic Tools | PharmCAT, Aldy, Stargazer [52] | Specialized tools for pharmacogene variant calling and star allele assignment | Open-source and commercially available |
| Knowledgebases | PharmGKB, CPIC, DPWG [51] [49] | Curated drug-gene associations, clinical guidelines, and implementation resources | Freely available online databases |
| Reference Materials | Coriell Cell Repositories, GeT-RM samples [54] | Characterized reference materials for assay validation and quality control | Biobank repositories |
| Statistical Packages | PLINK, PharmRS [51] | Population genetics analysis, association studies, phenotype prediction | Open-source statistical tools |
| AI/ML Frameworks | Hubble.2D6, AlphaMissense [52] | Deep learning models for predicting variant functional impact | Research implementations |
Discussion: Integration of Evolutionary History into Pharmacogenomics
The convergence of evolutionary biology and pharmacogenomics provides critical insights into the geographic distribution of pharmacogenetic variants and their clinical implications. Ancestral genetic adaptations to environmental factors, dietary patterns, and pathogen exposures have resulted in pronounced population-specific differences in allele frequencies of clinically important pharmacogenes [49]. For instance, the HLA-B*15:02 allele associated with carbamazepine-induced severe cutaneous adverse reactions is predominantly found in Southeast Asian populations but is rare in European descent groups, reflecting differential evolutionary selection pressure [49].
The implementation challenge remains substantial despite robust evidence supporting pharmacogenomic testing. Major barriers include integration into clinical workflow, provider education, evidence generation, and reimbursement structures [53]. However, implementation initiatives such as the NIH's All of Us Research Program, the EU's Ubiquitous Pharmacogenomics Consortium, and institutional programs like Vanderbilt's PREDICT have demonstrated feasibility and clinical impact across diverse care settings [53]. These programs provide roadmaps for leveraging evolutionary-informed pharmacogenomics to reduce health disparities and improve medication outcomes across populations.
Future directions point toward increased integration of multi-omics data, artificial intelligence, and sophisticated bioinformatic tools to unravel the complex interplay between evolutionary history, genetic variation, and drug response [52]. As these technologies mature, they will enable increasingly sophisticated models that predict individual drug responses based on genetic background, potentially transforming drug development and clinical therapeutics through an evolutionary medicine lens.
Pharmacogenomics represents a fundamental convergence of evolutionary biology and clinical medicine, providing powerful frameworks for personalizing treatment regimens based on individual genetic makeup. The methodological comparisons presented herein demonstrate a progressive evolution from reactive single-gene testing toward preemptive, comprehensive genetic profiling that more accurately reflects the polygenic nature of drug response. As the field advances, integrating evolutionary perspectives with cutting-edge genomic technologies will accelerate the development of truly personalized therapeutic strategies that optimize efficacy and minimize adverse events across diverse human populations. The continued validation of evolutionary medicine approaches through rigorous pharmacogenomic research promises to transform drug therapy from population-based averages to individually optimized treatments rooted in our shared genetic history.
Overcoming Implementation Barriers: Clinical Translation and Optimization
Evolutionary medicine, sometimes called Darwinian medicine, applies insights from ecology and evolutionary biology to understand health and disease [2] [55]. This approach provides a critical framework for addressing the complexity of human biology by investigating why natural selection has left humans vulnerable to disease rather than focusing solely on proximate mechanical causes [2] [4]. Despite its demonstrated value, evolutionary medicine has not yet been fully integrated into mainstream medical curricula or clinical practice [26] [1] [55]. The foundational principle of this field recognizes that selection acts to maximize reproductive success, not health or longevity, resulting in bodies that are "bundles of compromises shaped by natural selection in small increments to maximize reproduction, not health" [1] [2]. This perspective fundamentally challenges the prevalent metaphor of the body as a perfectly designed machine and instead explains disease vulnerability through specific evolutionary pathways including trade-offs, constraints, mismatches, and co-evolutionary arms races with pathogens [2] [4].
The core principles of evolutionary medicine provide a systematic framework for understanding disease vulnerability. Experts have consensus on fourteen core principles that can be grouped into five general categories: question framing (distinguishing between proximate and ultimate explanations), evolutionary processes, evolutionary trade-offs, reasons for vulnerability, and cultural influences [2]. This framework enables researchers and clinicians to ask fundamentally different questions about disease etiology, moving beyond "how" disease mechanisms work to "why" these vulnerable systems evolved in the first place [1] [4]. This review will validate evolutionary medicine approaches through comparative analysis of experimental data, detailed methodological protocols, and visualization of key conceptual frameworks driving innovation in biomedical research and therapeutic development.
Core Principles and Pathways to Disease
Evolutionary medicine identifies several specific pathways through which evolutionary processes influence disease risk. These pathways provide a systematic framework for classifying and understanding the complex relationship between our evolutionary history and modern health challenges [4]. The table below outlines the major pathways with their conceptual foundations and clinical examples.
Table: Major Evolutionary Pathways to Disease Vulnerability
| Pathway | Conceptual Basis | Clinical Examples |
|---|---|---|
| Evolutionary Mismatch | Discrepancy between contemporary environments and those in which humans evolved | Myopia, metabolic syndrome, obesity, cardiovascular disease [4] [55] |
| Life History-Associated Factors | Trade-offs and antagonistic pleiotropy in energy allocation across lifespan | Early life nutrition affecting adult obesity and metabolic dysfunction [4] |
| Excessive Defense Mechanisms | Dysregulation of normally adaptive defense responses | Extreme pyrexia, chronic inflammation, anxiety disorders [4] |
| Human-Pathogen Coevolution | Rapid microbial evolution outpacing human adaptation | Antibiotic resistance, emerging infectious diseases [4] [55] |
| Evolutionary Constraints | Limitations imposed by evolutionary history and anatomical design | Back pain from bipedalism, blind spot in eye, susceptibility to glaucoma [2] [4] |
| Sexual Selection | Competition and choice influencing traits and vulnerabilities | Higher male mortality, sex-specific disease risks [2] [4] |
| Balancing Selection | Heterozygote advantage maintaining deleterious alleles | Sickle cell anemia persisting due to malaria resistance [4] |
These pathways operate not in isolation but through complex interactions that influence disease risk across the human lifespan. The mismatch pathway, particularly relevant to modern health, explains many chronic diseases as resulting from disparities between our current environments and those in which our physiological systems evolved [2] [55]. Meanwhile, trade-offs represent another fundamental concept, where evolutionary changes that improve one trait often come at the expense of others, such as the compromise between running efficiency and birth canal size in women, or between encephalization and gut size [2].
Table: Evolutionary Trade-Offs in Human Biology
| Trade-Off | Beneficial Adaptation | Cost/Vulnerability |
|---|---|---|
| Pelvic anatomy | Efficient bipedal locomotion | Difficult childbirth [2] |
| Metabolic allocation | Brain size expansion | Reduced gut size [2] |
| Immune function | Protection from pathogens | Energy expenditure and inflammation [56] |
| Tissue maintenance | Reproductive success early in life | Senescence and aging [56] [2] |
Comparative Analysis of Evolutionary Medicine Applications
Evolutionary principles have been successfully applied across multiple medical domains, generating novel insights and therapeutic approaches. The table below provides a comparative analysis of key application areas, their evolutionary foundations, and experimental evidence supporting their validity.
Table: Comparative Analysis of Evolutionary Medicine Applications
| Application Area | Evolutionary Foundation | Key Findings/Outcomes | Experimental Evidence |
|---|---|---|---|
| Cancer Therapy | Somatic evolution and clonal selection; viewing cancer as evolutionary process of "cheater" cells [55] | Adaptive therapy approaches extend progression-free survival by maintaining treatment-sensitive cells; extinction therapy aims to prevent resistance [55] | Mathematical modeling of resistance evolution; in vivo studies showing delayed resistance with evolutionary-informed dosing [55] |
| Antimicrobial Resistance | Host-pathogen coevolution and rapid microbial adaptation [4] [55] | Phage therapy circumvents antibiotic resistance; anti-antibiotics target resistance mechanisms directly [55] | Clinical trials for multi-drug resistant bacterial infections showing efficacy where antibiotics fail [55] |
| Metabolic Disease | Mismatch between evolved physiology and modern environments [2] [55] | Lifestyle diseases understood as discordance with ancestral conditions; early life interventions show long-term protective effects [55] | Epidemiological studies of populations in transition; clinical trials of perinatal interventions reducing later disease risk [55] |
| Infectious Disease Management | Pathogen evolution and virulence-transmission trade-offs [55] | Evolutionary models predict pandemic trajectories; inform public health responses [55] | COVID-19 pandemic modeling; comparative analysis of virulence factors across pathogens [55] |
| Aging and Senescence | Antagonistic pleiotropy (genes beneficial early, harmful late) [2] [4] | Recognition that aging represents trade-offs favoring early reproduction over longevity [2] | Genetic studies identifying pleiotropic genes; comparative biology of species with different life history strategies [2] |
The experimental validation of evolutionary medicine approaches spans mathematical modeling, comparative biology, clinical trials, and epidemiological research. In cancer, for instance, evolutionary principles have inspired "adaptive therapy" that aims to control rather than eradicate tumors, thereby reducing selection pressure for treatment-resistant clones [55]. This approach has demonstrated extended progression-free survival in mathematical models and animal studies compared to conventional high-dose therapy [55]. Similarly, phage therapy represents an evolution-informed alternative to antibiotics that co-opts the natural evolutionary arms race between bacteriophages and bacteria, showing particular promise for treating multi-drug resistant infections in clinical settings [55].
Methodological Approaches and Experimental Protocols
Phylogenetic Comparative Analysis for Identifying Natural Disease Resistance
Protocol Objective: To systematically identify animal species with natural resistance or vulnerability to human diseases through phylogenetic analysis.
Materials and Reagents:
- Genomic databases (NCBI, Ensembl)
- Phylogenetic analysis software (BEAST, MrBayes, PHYLIP)
- Species trait databases (PanTHERIA, AnAge)
- Tissue samples from multiple species for functional validation
Methodology:
- Trait Mapping: Compile disease vulnerability/resistance data across diverse species using literature review and database mining [55]
- Phylogenetic Reconstruction: Build robust phylogenetic trees using multiple genetic markers to establish evolutionary relationships
- Comparative Analysis: Use statistical methods (e.g., independent contrasts) to identify evolutionary correlations between traits and disease resistance while accounting for shared ancestry [55]
- Convergence Detection: Identify instances of convergent evolution where distantly related species independently evolved similar resistance mechanisms
- Mechanistic Validation: Conduct functional experiments on identified species to elucidate molecular and physiological basis of resistance [55]
This methodology has successfully identified natural models of disease resistance, including species resistant to cancer, atherosclerosis, and neurodegenerative diseases, providing blueprints for novel therapeutic approaches [55].
Experimental Evolution of Treatment Resistance
Protocol Objective: To model and anticipate the evolution of treatment resistance in cancers and pathogens.
Materials and Reagents:
- Cell cultures (cancer cell lines or microbial pathogens)
- Therapeutic agents (chemotherapeutics, antibiotics, antimicrobials)
- Genomic sequencing equipment
- High-throughput screening systems
Methodology:
- Selection Regimen Design: Establish multiple parallel evolution experiments with different treatment strategies (continuous dosing, pulsed therapy, combination therapy) [55]
- Longitudinal Monitoring: Track phenotypic and genotypic changes across generations using regular sampling and whole-genome sequencing
- Fitness Landscapes Mapping: Measure fitness (reproductive rate) of evolved lineages in both treatment and treatment-free environments
- Cross-Resistance Profiling: Test evolved lineages against alternative therapeutic agents to identify collateral sensitivity/resistance patterns
- Evolutionary Modeling: Develop mathematical models predicting resistance evolution under different treatment scenarios
This experimental evolution approach has revealed fundamental principles about resistance evolution and informed the development of evolution-based treatment strategies that better manage resistance [55].
Visualization of Key Evolutionary Medicine Concepts
Evolutionary Pathways to Disease Diagram
Figure: Evolutionary Pathways to Disease Vulnerability. This diagram illustrates the major evolutionary pathways that explain human vulnerability to disease, highlighting how interactions between evolutionary history and modern environments create specific health challenges.
Evolutionary Medicine Research Workflow
Figure: Evolutionary Medicine Research Workflow. This diagram outlines the systematic approach for translating evolutionary insights into clinical applications, highlighting the interdisciplinary methods required to validate evolutionary hypotheses.
Research Reagent Solutions for Evolutionary Medicine
Table: Essential Research Tools for Evolutionary Medicine Investigations
| Research Tool Category | Specific Examples | Application in Evolutionary Medicine |
|---|---|---|
| Genomic Sequencing Platforms | Whole genome sequencing, RNA-seq, single-cell sequencing | Comparative genomics to identify evolutionary conserved elements; tracking pathogen evolution [55] |
| Phylogenetic Analysis Software | BEAST, MrBayes, PHYLIP, RAxML | Reconstructing evolutionary relationships; dating evolutionary events; identifying selection pressures [55] |
| Animal Model Systems | Natural disease-resistant species (naked mole rat, elephant, bat) | Identifying evolved protection mechanisms against cancer, neurodegeneration, metabolic disease [55] |
| Experimental Evolution Setups | Chemostats, serial passage protocols, tumor cell line evolution | Modeling treatment resistance evolution; testing evolutionary-informed therapy schedules [55] |
| Bioinformatics Databases | UCSC Genome Browser, OrthoDB, PANTHER, NHGRI GWAS Catalog | Mapping evolutionary conserved regions; identifying positively selected genes; analyzing population genetics [56] |
| Paleogenomic Resources | Ancient DNA datasets, comparative primate genomes | Reconstructing ancestral states; tracking evolutionary changes in human lineage [2] |
These research tools enable the systematic investigation of evolutionary questions in medicine, from identifying naturally occurring disease resistance in other species to modeling the evolutionary dynamics of treatment resistance in pathogens and cancers. The integration of comparative biology with modern genomic techniques represents a particularly powerful approach for discovering novel therapeutic strategies inspired by evolutionary solutions to health challenges [55].
The integration of evolutionary principles into medical systems represents a paradigm shift in how we understand, prevent, and treat disease. The experimental data and methodological approaches summarized in this review demonstrate that evolutionary medicine provides not just theoretical insights but practical, actionable strategies for addressing complex health challenges. From managing treatment resistance in cancer and infectious diseases through evolutionary-informed therapies to preventing chronic diseases by addressing evolutionary mismatches, this framework offers a more comprehensive understanding of health and disease that complements traditional mechanistic approaches [55].
The validation of evolutionary medicine comes from multiple lines of evidence: the success of evolutionary-informed therapeutic strategies in clinical and experimental settings, the identification of natural disease resistance models through comparative phylogenetics, and the explanatory power of evolutionary principles for understanding patterns of disease vulnerability across populations and life stages [55]. As the field continues to develop, key research priorities include systematic phylogenetic mapping of disease vulnerability and resistance across species, clinical trials of evolution-based therapeutic approaches, and the development of educational frameworks to integrate evolutionary thinking into medical training [55]. By embracing the complexity of our evolutionary heritage, researchers and clinicians can develop more effective, innovative approaches to promoting human health in the context of our deeply evolutionary nature.
Navigating Clinical Trial Challenges for Evolution-Informed Therapies
Evolutionary medicine, which applies principles from evolution and ecology to biomedical problems, is emerging as a transformational approach for understanding and treating disease. This paradigm recognizes that pathological conditions, from cancer to antimicrobial resistance, are under continuous evolutionary pressure. The fundamental insight driving this field is that therapeutic interventions themselves impose selective pressures that can lead to treatment resistance, necessitating clinical trial designs that account for these dynamic processes. Where traditional approaches often match therapies to static molecular characteristics, evolution-informed strategies dynamically adjust to the evolutionary trajectories of diseases, offering potential for improved long-term outcomes [57] [5].
The validation of these novel approaches faces significant methodological challenges in the clinical trial landscape. This guide examines the current state of evolution-informed clinical trials, comparing emerging strategies, their experimental foundations, and the practical solutions researchers are deploying to generate robust evidence for these innovative therapies.
Comparative Analysis of Evolution-Informed Therapeutic Strategies
The table below summarizes three prominent evolution-informed approaches currently advancing through clinical investigation:
Table 1: Comparison of Evolution-Informed Therapeutic Strategies
| Therapeutic Approach | Core Evolutionary Principle | Target Indications | Key Challenges in Clinical Validation |
|---|---|---|---|
| Dynamic Precision Medicine (DPM) [57] | Control of heterogeneous cell populations to prevent resistant subclone expansion | Oncology (Solid Tumors, Hematologic Malignancies) | Requires predictive evolutionary classifiers; complex dosing algorithms |
| Evolutionarily Informed Microbiome Therapy [58] | Exploitation of collateral sensitivity and ancestral state restoration | Chronic Inflammatory Bowel Disease (IBD) | Standardization of bacterial strain delivery; regional gut adaptation dynamics |
| Adaptive Therapy [5] | Maintenance of treatment-sensitive competitors to suppress resistant populations | Advanced Cancers, Antimicrobial Resistance | Determining optimal drug reduction thresholds; monitoring competitor populations |
These strategies represent a shift from maximal cell kill towards ecological control, where the goal is long-term disease management rather than complete eradication in the short term. The DPM approach employs mathematical models of tumor evolution to guide the sequencing and timing of therapies in a more personalized manner than current precision medicine [57]. Microbiome therapies leverage the concept of collateral sensitivity, where bacteria adapted to inflammatory environments become vulnerable to specific antibiotics, offering targeted treatment possibilities for IBD [58]. Adaptive therapy explicitly aims to maintain a population of treatment-sensitive cells that can outcompete resistant variants through ecological competition [5].
Experimental Designs for Validating Evolutionary Therapies
Clinical Trial Methodologies
Validating evolutionary therapies requires innovative trial designs that differ substantially from conventional models:
Table 2: Clinical Trial Designs for Evolutionary Medicine Approaches
| Trial Design Element | Conventional Trial | Evolution-Informed Trial | Validation Requirements |
|---|---|---|---|
| Primary Endpoint | Progression-free survival, overall survival | Time to evolutionary escape, resistance-free survival | Development of evolutionary biomarkers; resistance monitoring protocols |
| Patient Stratification | Consensus molecular characteristics | Evolutionary classifier predictions [57] | Validation of evolutionary classifiers; phylogenetic tracking methods |
| Therapeutic Protocol | Fixed dosing based on maximum tolerated dose | Dynamic dosing based on tumor burden/response [5] | Real-time monitoring technologies; adaptive dosing algorithms |
| Control Arm | Standard of care or placebo | Evolutionary therapy vs. standard precision medicine [57] | Stratified randomization based on evolutionary risk |
The proof-of-concept design for Evolutionary Guided Precision Medicine (EGPM) employs a stratified randomized approach where patients are randomized based on whether they are predicted to benefit from the evolutionary strategy using a dedicated evolutionary classifier [57]. This design specifically tests whether patients with certain evolutionary trajectories experience improved outcomes when treated with evolution-informed strategies compared to current precision medicine approaches.
Computational and Molecular Methodologies
The experimental workflow for evolution-informed trials integrates diverse computational and molecular techniques:
Figure 1: Experimental workflow for evolution-informed therapies showing the adaptive feedback loop between monitoring and treatment decisions.
Strain-level resolution has emerged as a critical requirement in microbiome-related trials, as functional differences often exist at the strain level rather than species level. For example, Escherichia coli may be neutral, pathogenic, or probiotic depending on the strain [59]. Methodologies for strain identification include:
- Single Nucleotide Variant (SNV) analysis: Calling SNVs within a community or between community members and reference genomes, requiring deep coverage (typically 10× or more) of each microbial strain [59]
- Variable region identification: Detecting presence or absence of genes or genomic regions, requiring less sequencing depth but more susceptible to noise [59]
- Metatranscriptomic profiling: RNA sequencing to characterize dynamic functional activity in microbial communities, though this requires careful sample preservation and paired metagenomes for proper interpretation [59]
The Scientist's Toolkit: Essential Research Reagents and Platforms
Successful implementation of evolution-informed trials requires specialized reagents and platforms:
Table 3: Essential Research Reagents and Platforms for Evolution-Informed Clinical Research
| Reagent/Platform Category | Specific Examples | Research Function | Considerations for Clinical Translation |
|---|---|---|---|
| Strain Identification | 16S rRNA sequencing, Shotgun metagenomics, SNV calling algorithms [59] | Differentiates functional strains within species | Standardization across sites; validation of bioinformatic pipelines |
| Evolutionary Tracking | Phylogenetic markers, Lineage tracing, Resistance gene panels | Monates evolutionary trajectories in real time | Frequency of sampling; detection sensitivity thresholds |
| Mathematical Modeling | Population dynamics models, Evolutionary classifiers [57] | Predicts resistance development; optimizes dosing | Model calibration; integration into clinical workflow |
| Bacterial Strain Libraries | Ancestral bacterial strains, Engineered competitors [58] | Ancestral-State Restorative Therapy | Safety profiling; delivery vehicle development |
These tools enable the quantitative analysis of evolutionary dynamics that underpin these novel therapeutic approaches. The evolutionary classifiers used in DPM trials, for instance, combine mathematical modeling of cancer evolution with molecular characterization to identify patients most likely to benefit from evolution-informed treatment sequences [57]. For microbiome therapies, standardized strain libraries and delivery systems are essential for translating laboratory findings into reproducible clinical interventions [58].
Conceptual Framework of Evolutionary Dynamics in Disease
Evolution-informed therapies target the fundamental dynamics of disease adaptation:
Figure 2: Evolutionary dynamics framework showing conventional therapeutic failure (red) versus ecological control (green) pathways.
The conceptual basis for these approaches recognizes that conventional therapies typically apply continuous maximum pressure, eliminating drug-sensitive competitors and allowing resistant subpopulations to expand freely [5]. In contrast, evolution-informed approaches maintain ecological control by preserving sensitive populations that can competitively suppress resistant variants through various mechanisms:
- Resource competition: Sensitive and resistant cells compete for limited nutrients and space
- Interference competition: Direct inhibition of resistant variants by sensitive populations
- Collateral sensitivity: Resistant variants pay fitness costs that make them vulnerable in specific environments [58]
This framework explains why dose modulation rather than continuous maximum dosing may produce superior long-term outcomes in evolution-informed trials [5].
The validation of evolution-informed therapies represents a frontier in clinical development that requires interdisciplinary collaboration between clinicians, evolutionary biologists, computational scientists, and trial methodologies. The approaches outlined in this guide demonstrate the potential of evolutionary thinking to address some of the most persistent challenges in medicine, particularly in oncology and chronic inflammatory diseases.
As these strategies advance, key research priorities include standardizing evolutionary biomarkers, developing robust computational models that can be integrated into clinical workflows, and addressing the operational challenges of implementing adaptive trial designs across multiple sites. The continued refinement of these methodologies offers the promise of transforming how we approach therapeutic resistance, moving from reactive treatment failure to proactive evolutionary control.
The field of biomimetic translation operates on a core principle of evolutionary medicine: that insights gained from the diverse physiological adaptations and disease responses across the animal kingdom can be strategically applied to address human health challenges [5]. This approach leverages millions of years of evolutionary experimentation, treating animal models not merely as experimental surrogates but as validated repositories of biological innovation [5]. The fundamental premise recognizes that natural selection has equipped various species with unique mechanisms for resisting diseases, repairing tissues, and maintaining physiological resilience—mechanisms that, when properly understood and translated, can inform novel therapeutic strategies for human applications [5].
The translational pipeline from animal models to human therapies represents a critical bridge between basic biological discovery and clinical implementation. Biomimetic translation extends beyond simply testing interventions in animals; it involves a deliberate, systematic mapping of physiological solutions that have evolved in nature and their strategic application to human medicine [5]. This process requires rigorous validation at multiple levels, from cellular mechanisms to system-wide physiological responses, ensuring that insights gleaned from animal models maintain their relevance when applied to the human context. As evolutionary medicine principles suggest, this approach can spark transformational innovation in biomedical research by uncovering resistance mechanisms that have evolved in other species to counter diseases that plague humans [5].
Comparative Analysis of Advanced Animal Models in Biomedical Research
Performance Metrics of Translational Animal Models
The efficacy of animal models in predictive biomedical research varies significantly across model types and disease areas. The table below summarizes quantitative performance data for several advanced animal models in translating findings to human applications.
Table 1: Quantitative Comparison of Advanced Animal Models in Translational Research
| Animal Model Type | Key Application Areas | Reported Efficacy/Improvement | Translational Advantages | Identified Limitations |
|---|---|---|---|---|
| CRISPR-Engineered Osteoporotic Rodents | Orthopedic implants, bone regeneration | 45% impaired bone regeneration enabling precise scaffold evaluation [60] | Exact pathophysiological modeling; High reproducibility for screening [60] | Limited representation of human bone remodeling complexity [60] |
| Humanized Porcine Models | Vascular implants, cardiovascular devices | 30% endothelialization improvement reducing thrombosis risk [60] | Similar vascular anatomy and healing responses; Predictive of human immune response [60] | High maintenance costs; Ethical considerations [60] [61] |
| Diabetic Animal Models with Biosensor-Integrated Implants | Smart implants, wound healing | 60% quicker wound healing with bioresponsive implants [60] | Real-time monitoring capability; Individualized therapeutic testing [60] | Challenges in long-term sensor stability [60] |
| Humanized Mouse Models | Immunomodulatory coatings, inflammatory response | 50% reduction in chronic rejection with advanced polymeric coatings [60] | Human-specific immune response prediction; Suitable for high-throughput screening [60] | Incomplete recapitulation of human immune system complexity [60] [61] |
| Non-Human Primate Models | Vaccine development, infectious diseases | High predictive value for human immune responses [61] | Closest genetic and physiological similarity to humans [61] | Ethical concerns; High cost; Limited availability [61] |
| Genetically Diverse Mouse Populations | Personalized medicine approaches | Improved prediction of variable drug responses [61] | Modeling human population heterogeneity; Identification of subgroup-specific effects [61] | Complex breeding schemes; Data interpretation challenges [61] |
Evolutionary-Validated Animal Models in Disease Research
Certain animal models demonstrate exceptional value when their use is guided by evolutionary principles, particularly when they exhibit natural resistance or unique physiological adaptations to diseases that affect humans.
Table 2: Evolutionarily-Informed Animal Models for Disease Research
| Animal Model | Evolutionary Adaptation/Disease Resistance | Research Applications | Translational Insights |
|---|---|---|---|
| Naked Mole Rats | Exceptional oxidative stress resistance and longevity [24] [5] | Aging research, neurodegenerative disorders | Cellular mechanisms protecting against protein aggregation [24] |
| Elephants | Duplicated tumor suppressor genes conferring low cancer risk [24] [5] | Oncology, cancer prevention strategies | Novel approaches to activate backup tumor suppressor pathways [24] |
| Bats | Unexpected longevity relative to body size; viral tolerance [24] [5] | Infectious disease, immunology, aging | Mechanisms for controlled inflammatory responses despite viral carriage [24] |
| Species with APOL1 Gene Variants | Resistance to Trypanosoma brucei infection (African sleeping sickness) [24] | Infectious disease, kidney pathophysiology | Pleiotropic trade-offs: protective variants increase kidney disease risk [24] |
Experimental Protocols for Biomimetic Translation
Protocol 1: CRISPR-Engineered Large Animal Models for Orthopedic Implant Testing
Objective: To evaluate novel orthopedic implant materials and designs in large animal models with genetically modified bone metabolism to predict human clinical performance.
Methodology:
- Model Generation: Utilize CRISPR-Cas9 to introduce specific mutations in genes regulating bone metabolism (e.g., LRP5, VDR, COL1A1) in porcine models, creating phenotypes mimicking human osteoporosis or impaired bone healing [60].
- Implant Placement: Surgically implant test and control materials into critical-sized defects in long bones, ensuring precise anatomical placement and stabilization.
- Longitudinal Monitoring: Employ multi-modal imaging (micro-CT, PET) at 2, 4, 8, and 12-week intervals to quantify bone formation and implant integration.
- Biomechanical Testing: At endpoint (typically 12-16 weeks), perform torsion testing to failure to assess functional integration strength.
- Histomorphometric Analysis: Process explanted bone-implant interfaces for undecalcified histology, quantifying bone-implant contact percentage and new bone area within implant threads.
Key Parameters: Bone volume/total volume (BV/TV) ratio, bone-implant contact (BIC) percentage, push-out strength, removal torque values.
Protocol 2: Humanized Vascular Graft Assessment in Porcine Models
Objective: To assess the endothelialization and biocompatibility of novel vascular graft materials with humanized immune responses.
Methodology:
- Model Humanization: Reconstitute immunodeficient porcine models with human hematopoietic stem cells to create a functional human immune system [60].
- Graft Implantation: Interpositionally place test vascular grafts (3-5cm length) in the carotid or femoral artery position using microvascular techniques.
- Antiplatelet Regimen: Administer dual antiplatelet therapy (aspirin + clopidogrel) for 4 weeks post-operatively to prevent acute thrombosis.
- Serial Angiography: Perform digital subtraction angiography at 2, 4, and 8 weeks to assess graft patency and any narrowing.
- Flow Cytometry Analysis: Monitor human immune cell populations in peripheral blood weekly to ensure stable humanization.
- Ex Vivo Analysis: At 8-week endpoint, process explanted grafts for scanning electron microscopy to quantify endothelial cell coverage and immunofluorescence staining for specific human immune cell markers.
Key Parameters: Patency rate, endothelialization percentage, neointimal hyperplasia thickness, human immune cell infiltration.
Biomimetic Translation Workflow
The following diagram illustrates the integrated workflow for translating insights from animal models to human applications, highlighting the critical validation checkpoints throughout the process.
Diagram 1: Biomimetic translation workflow for evolutionary medicine
The Scientist's Toolkit: Essential Research Reagents and Materials
Successful implementation of biomimetic translation research requires specialized reagents and materials tailored to the unique requirements of advanced animal models and analytical techniques.
Table 3: Essential Research Reagents for Biomimetic Translation Studies
| Reagent/Material | Function/Application | Specific Considerations |
|---|---|---|
| CRISPR-Cas9 Gene Editing Systems | Creation of genetically engineered disease models [60] | Species-specific gRNA design; Optimal delivery methods (viral vs. non-viral) |
| Human Hematopoietic Stem Cells | Generation of humanized immune systems in animal models [60] | Source (cord blood vs. bone marrow); Purity requirements; Compatibility with host species |
| Advanced Polymeric Coating Materials | Enhancing implant biocompatibility and drug delivery [60] | Degradation profiles; Mechanical properties matching native tissue; Drug release kinetics |
| Biosensor-Integrated Implant Systems | Real-time monitoring of physiological parameters and healing progress [60] | Biocompatible encapsulation; Wireless data transmission; Power source longevity |
| Micro-CT Imaging Contrast Agents | High-resolution 3D visualization of bone-implant integration and vascularization [60] [62] | Tissue-specific targeting; Appropriate radiation dosage; Quantification algorithms |
| Organ-on-Chip Platforms | Intermediate validation between cell culture and whole animal studies [62] | Cell source authenticity; Fluid dynamics mimicking physiological conditions; Multi-tissue integration capability |
| Biomimetic Chromatography Systems | Early prediction of compound behavior in biological systems [63] | Stationary phase selection (IAM, HSA); Mobile phase composition; Correlation with in vivo data |
Evolutionary Medicine Framework for Model Selection
The principles of evolutionary medicine provide a strategic framework for selecting appropriate animal models based on shared evolutionary history, convergent adaptations, or unique physiological solutions to environmental challenges [5]. This approach moves beyond traditional model selection toward a more deliberate identification of species that offer specific insights into human disease mechanisms or treatment responses.
Evolutionary mismatch—the phenomenon whereby genetic variants that were adaptive in past environments now increase disease risk in modern contexts—represents a particularly valuable concept for model development [24] [5]. Animal models that recapitulate these mismatches can provide powerful platforms for understanding complex modern human diseases like obesity, autoimmune disorders, and certain metabolic conditions [5]. Similarly, the concept of pleiotropic trade-offs, where genetic variants that protect against one disease may increase vulnerability to another, can be effectively modeled in animals to understand the complex network of genetic influences on human health [24].
The growing recognition that many pathologies associated with human lifestyles (including atherosclerosis, type 2 diabetes, various cancers, and arthritis) are shared across species further validates the comparative approach [5]. This perspective enables researchers to identify species that naturally resist these conditions despite shared vulnerability, offering opportunities to identify protective mechanisms that might be therapeutically induced in humans.
The future of biomimetic translation lies in increasingly sophisticated integration of evolutionary principles with cutting-edge technologies. Several promising directions are emerging:
Systematic Phylogenetic Mapping: Large-scale comparative genomics and physiology studies across diverse species to identify natural models of disease resistance and tissue regeneration [5]. This systematic approach would move beyond traditional model organisms to capitalize on the full diversity of biological solutions evolved in nature.
AI-Guided Model Selection: Implementation of artificial intelligence and machine learning to analyze cross-species data and identify the most predictive animal models for specific human disease contexts or therapeutic questions [60] [64].
Hybrid Validation Systems: Development of integrated validation pipelines that combine animal models with human organ-on-chip systems and 3D bioprinted tissues, creating stepped validation processes that enhance predictive power while reducing animal use [62].
Evolutionary-Informed Clinical Trial Design: Application of evolutionary principles to clinical trial design, including anticipating treatment resistance through evolutionary models and identifying patient subgroups based on evolutionary histories [5].
As these approaches mature, biomimetic translation will increasingly fulfill its potential as a powerful framework for bridging the gap between animal studies and human applications, ultimately accelerating the development of effective therapies while respecting the ethical imperative to minimize animal use where alternatives exist.
Overcoming Professional and Educational Barriers in Medical Practice
In the context of validating evolutionary medicine approaches, overcoming professional and educational barriers is not merely an operational concern but a fundamental requirement for scientific progress. Evolutionary medicine—the application of evolutionary and ecological principles to biomedicine—holds tremendous potential to spark transformational innovation in biomedical research and public health [38]. However, its integration into mainstream medical practice faces significant challenges across educational, professional, and systemic dimensions. This article explores these barriers within a broader thesis on validating evolutionary medicine, comparing traditional approaches with innovative solutions informed by evolutionary principles themselves. By examining these hurdles through the very lens of evolutionary theory—considering adaptation, mismatch, and complex system dynamics—we can develop more robust and effective strategies for advancing this promising field.
The validation of evolutionary medicine relies on navigating a complex landscape of professional practices and educational pathways. From medical students encountering research for the first time to experienced professionals implementing data-driven approaches in infectious disease control, the challenges reflect systemic issues that require fundamental rethinking. By comparing traditional approaches with evolution-informed strategies across these domains, we can identify more adaptive solutions better suited to the complex, dynamic nature of both biological systems and scientific practice.
Educational Barriers: Bridging the Gap in Medical Training
The Challenge of Research Integration in Medical Curricula
Medical education faces significant challenges in integrating meaningful research experiences, particularly in emerging fields like evolutionary medicine. Quantitative studies reveal that medical students generally possess favorable attitudes toward research, with mean attitude scores of 104.72 (well above the scale midpoint of 78) in pre-intervention assessments [65]. Despite this positive disposition, significant barriers impede effective research integration, including academic overload, lack of mentorship, and insufficient training in scientific writing and statistics [65] [66]. These challenges are particularly pronounced for evolutionary medicine, which requires integrating concepts across traditional disciplinary boundaries.
The pressure to accumulate research publications for residency applications has created an "arms race" that often prioritizes quantity over quality, potentially undermining research integrity and meaningful scientific engagement [66]. This system can discourage exploration of innovative but riskier research avenues like evolutionary medicine, as students and residents gravitate toward safer, more predictable projects with higher publication probabilities. The misalignment between educational incentives and high-quality scientific training represents a significant barrier to advancing novel approaches in medicine.
Table 1: Medical Student Attitudes and Barriers Toward Research
| Metric | Pre-Intervention Score | Scale Midpoint | Key Findings |
|---|---|---|---|
| Attitude Score | 104.72 | 78 | 73.3% of students scored above 75% of maximum possible [65] |
| Barrier Score | 109.61 | 87 | 96.7% of students scored above 50%; main concerns: time, mentorship, statistics training [65] |
Experimental Approaches to Educational Interventions
Educational research has employed various methodological approaches to address these barriers. One quasi-experimental study implemented an educational and motivational intervention consisting of 15 educational videos (mean duration: 13.66 minutes) and 5 motivational capsules (mean duration: 3.43 minutes) delivered over one month [65]. The intervention covered fundamental topics in biomedical research methodology, including research question formulation, study design, literature search, statistical analysis, and scientific writing. Despite this comprehensive approach, post-intervention assessments revealed no statistically significant changes in attitude or barrier scores, suggesting that short-term, self-directed strategies alone are insufficient for addressing deeply entrenched educational barriers [65].
These findings align with the perspective that effective research education requires long-term, interactive programs supported by curricular integration, structured mentorship, and institutional investment [65] [66]. For evolutionary medicine specifically, this suggests that successful integration would require embedding evolutionary concepts throughout the medical curriculum rather than offering isolated modules or short-term interventions. The complex, interdisciplinary nature of evolutionary medicine demands sustained engagement and contextualization within clinical applications to overcome the inherent barriers in medical education.
Diagram 1: Medical Education Barrier Pathways
Professional Practice Barriers: Implementing Innovation in Healthcare Systems
Data-Driven Approaches in Infectious Disease Control
The implementation of innovative approaches faces significant barriers in professional medical practice, as evidenced by research on data-driven infectious disease control (IDC). Qualitative studies involving 36 IDC professionals across nine focus group discussions revealed five key themes: (1) context of the work environment, (2) interpretation of data-driven work in IDC, (3) added value of data-driven approaches, (4) views on team participation, and (5) perspectives on development and implementation [67] [68]. While professionals generally expressed positive attitudes toward data-driven approaches, significant barriers emerged at individual, process, and organizational levels, including undefined roles, lack of shared vision, and insufficient protocols for data registration [67].
A critical finding across studies was the "limited translation of data into action," which was viewed as untapped potential for improving public health responses [67] [68]. This implementation gap reflects broader challenges in evolving professional practices to incorporate new scientific approaches. Participation in data-driven work varied substantially within teams and was influenced by multiple factors, including professional role, personal interest, workload, time constraints, knowledge gaps, and resistance to change [67]. These findings parallel the challenges faced in implementing evolutionary medicine approaches, which similarly require fundamental shifts in professional practice and organizational culture.
Table 2: Professional Barriers to Implementing Innovative Medical Approaches
| Barrier Category | Specific Challenges | Impact on Implementation |
|---|---|---|
| Individual Level | Knowledge gaps, resistance to change, time constraints [67] | Limited engagement with new approaches |
| Process Level | Undefined roles, lack of shared protocols, data translation issues [67] [68] | Inconsistent application and integration |
| Organizational Level | Lack of shared vision, insufficient infrastructure, undefined leadership [67] | Systemic resistance to change |
| Cultural/Perceptual | Variable interpretations of value, misunderstanding from stakeholders [67] [69] | Undermined collaboration and trust |
ICU Nursing and Professional Identity Challenges
Research on ICU nurses' professional identity provides additional insights into professional practice barriers, particularly within high-stress medical environments. A qualitative study of 37 ICU nurses identified four thematic areas influencing professional identity: Individual Motivation and Achievement System (IMAS), Team Collaboration and Support System (TCSS), Technology and Societal Support System (TSSS), and Sociocultural and Values System (SVS) [69]. Within these domains, key barriers included excessive workload, frequent night shifts, misunderstanding from patients' families, improper interprofessional collaboration, and the dual-edged nature of technological advances that both improve efficiency and increase skill-related anxiety [69].
These barriers directly impact the implementation of innovative approaches like evolutionary medicine by creating environments resistant to additional change and complexity. The study found that professional competence and a sense of irreplaceability enhanced intrinsic motivation, while excessive workload and promotion pressure undermined stability [69]. This suggests that successful integration of evolutionary medicine principles would require addressing these foundational professional practice issues alongside the scientific challenges, recognizing that innovative approaches are implemented within complex human systems with existing stresses and constraints.
Research and Development Barriers: From Discovery to Implementation
The "Valley of Death" in Drug and Device Development
The translation of basic research into clinical applications—a process particularly relevant for evolutionary medicine—faces well-documented barriers in the "valley of death" between laboratory discoveries and commercial clinical use. This challenge affects both pharmaceutical compounds and medical devices, with many promising innovations failing to reach patients due to financial, regulatory, and procedural hurdles [70]. One significant barrier is the frequent failure of interventions that succeed in highly controlled randomized clinical trials (RCTs) when implemented in real-world clinical settings with more diverse populations and less controlled conditions [70].
Experts identify several specific barriers in contemporary drug development, including the challenge of meeting patient expectations in target product profiles, inadequate diagnostic tools for precise patient stratification (particularly in neurological diseases), poor translation from animal models to human clinical outcomes (especially in pain research), and the translational gap between academic discovery and commercial development [71]. For evolutionary medicine approaches, which often challenge conventional diagnostic and treatment paradigms, these barriers are particularly pronounced, as they must overcome not only the standard translational hurdles but also resistance to fundamentally different conceptual frameworks.
Antimicrobial Resistance as a Case Study in Evolutionary Medicine Barriers
Antimicrobial resistance (AMR) represents a pressing global health challenge where evolutionary medicine approaches offer significant potential, yet face substantial implementation barriers. India alone loses approximately 400,000 lives annually to AMR, yet funding for this critical area remains extremely low [72]. This disconnect highlights how evolutionary perspectives—which naturally address pathogen evolution and resistance dynamics—struggle to secure resources within conventional funding and research frameworks.
Panel discussions with biotech leaders and researchers have identified several interconnected barriers in this domain, including inadequate traditional funding models for high-risk discovery research, insufficient collaboration between academic and industry sectors, regulatory challenges that lag behind scientific innovation, and talent development pipelines that fail to cultivate the necessary interdisciplinary expertise [72]. Overcoming these barriers requires innovative approaches such as blended financing models, larger grant pools, strengthened public-private partnerships, and enhanced integration of artificial intelligence and machine learning with traditional scientific methods [72].
Methodological Approaches: Experimental Protocols for Studying and Addressing Barriers
Qualitative Research Methodologies
Research on professional and educational barriers has employed rigorous qualitative methodologies to capture the complex, contextual nature of these challenges. The study on data-driven infectious disease control utilized exploratory online focus group discussions (FGDs) with professionals from Public Health Services [67] [68]. Between September 2024 and January 2025, nine FGDs were conducted with 36 IDC professionals, including medical doctors, nurses, infection preventionists, epidemiologists, policy advisors, project leaders, and managers [67]. The discussions were structured using a topic guide based on the Attitude-Social Influence-Efficacy model and the Consolidated Framework for Implementation Research, complemented with questions on current practices related to data-driven work [67].
The data analysis employed framework and thematic approaches, with two researchers independently coding all transcripts and discussing until consensus was reached [67]. This methodological rigor ensures that identified barriers reflect genuine professional experiences rather than researcher assumptions. Similarly, the study on ICU nurses' professional identity conducted one-on-one, semi-structured in-depth interviews with 37 ICU nurses, using Ecological Systems Theory as a theoretical framework and employing thematic analysis to identify key patterns [69]. These methodological approaches provide valuable templates for studying barriers to evolutionary medicine implementation.
Intervention Study Protocols
Research on educational barriers has implemented quasi-experimental intervention designs to test potential solutions. One study evaluated medical students' attitudes and perceived barriers before and after an educational and motivational intervention consisting of audiovisual content delivered over one month [65]. The intervention included 15 educational videos (mean duration: 13.66 minutes) covering fundamental research methodology topics and 5 motivational capsules (mean duration: 3.43 minutes) featuring testimonials from students with research experience [65].
The study used a validated questionnaire instrument adapted from previous research, with 26 items assessing attitudes and 29 items evaluating perceived barriers to research, all rated on a 5-point Likert scale [65]. The instrument demonstrated high internal consistency, with Cronbach's alpha values of 0.870 for attitudes and 0.953 for perceived barriers [65]. Despite this rigorous methodology, the intervention produced no statistically significant changes in outcomes, highlighting the resistance of educational barriers to short-term solutions and suggesting the need for more comprehensive, systemic approaches [65].
Diagram 2: Barrier Research Methodologies
The Scientist's Toolkit: Research Reagent Solutions for Barrier Investigation
Table 3: Essential Research Tools for Studying Medical Practice Barriers
| Tool/Resource | Function | Application Example |
|---|---|---|
| Validated Questionnaire Instruments | Quantitatively measure attitudes, barriers, and perceptions [65] | Assessing medical student attitudes toward research (26-item attitude scale, 29-item barrier scale) [65] |
| Focus Group Discussion Guides | Structured protocols for qualitative data collection [67] | Exploring IDC professionals' views on data-driven implementation using ASE and CFIR frameworks [67] |
| Theoretical Frameworks (CFIR, ASE, EST) | Provide conceptual structure for study design and analysis [67] [69] | Using Ecological Systems Theory to analyze ICU nurses' professional identity across multiple system levels [69] |
| Digital Recording and Transcription Tools | Ensure accurate capture and preservation of qualitative data [67] | Conducting online FGDs via Microsoft Teams with verbatim transcription for analysis [67] |
| Intervention Materials (Educational Videos) | Implement and test educational strategies [65] | Delivering research methodology content through 15 educational videos (mean duration: 13.66 minutes) [65] |
| Data Analysis Software | Facilitate systematic qualitative and quantitative analysis | Employing framework and thematic analysis for FGD transcripts [67] |
Comparative Analysis: Traditional vs. Evolution-Informed Approaches to Barrier Resolution
Fundamental Differences in Problem Framing
Traditional approaches to addressing professional and educational barriers in medicine often focus on symptomatic solutions rather than underlying systemic issues. For instance, when facing challenges in research education, conventional responses might include adding isolated research methodology courses or requiring publication for graduation [65] [66]. Similarly, barriers in professional practice often trigger standardized protocols and compliance measures that may fail to address root causes [67] [69]. These approaches reflect a mechanistic, reductionist worldview that dominates conventional medical science and education.
In contrast, evolution-informed approaches would frame these barriers through concepts like mismatch theory, evolutionary trade-offs, and complex adaptive systems [38]. The educational "arms race" in residency applications, for example, could be understood as an evolutionary trap where individual optimization strategies (maximizing publication numbers) undermine collective well-being (research quality and integrity) [66]. Similarly, resistance to data-driven approaches in infectious disease control might reflect evolved cognitive biases toward immediate, concrete information over abstract, statistical data—a potential mismatch between our evolutionary heritage and modern public health needs [67] [38]. This fundamental reframing enables more holistic and potentially more effective intervention strategies.
Implementation Strategy Comparison
Implementation strategies differ significantly between traditional and evolution-informed approaches. Traditional barrier reduction often employs linear, top-down interventions, such as the educational video intervention that failed to produce significant changes in medical student attitudes and barriers despite comprehensive content coverage [65]. In professional settings, conventional approaches might mandate compliance with new protocols without addressing the underlying system dynamics that generate resistance [67] [69].
Evolution-informed strategies would instead employ variation, selection, and retention processes adapted to specific contexts [38]. Rather than implementing standardized solutions across diverse settings, an evolutionary approach would encourage experimentation with multiple strategies, identify and amplify successful variants, and create feedback mechanisms for continuous adaptation. For example, instead of a single research curriculum for all medical students, an evolution-informed approach might offer diverse research experiences with different methodologies, topics, and intensity levels, allowing students to find better-matched opportunities based on their interests, skills, and career goals [66]. This approach aligns with evolutionary principles of diversity and selection, potentially creating more resilient and adaptive educational systems.
The validation of evolutionary medicine approaches depends not only on demonstrating their scientific efficacy but also on successfully navigating the professional and educational barriers that impede their adoption. The research reviewed herein suggests that conventional approaches to addressing these barriers have achieved limited success, often failing to account for the complex, systemic nature of medical education and practice. An evolution-informed perspective offers promising alternatives by framing these challenges through concepts like mismatch theory, evolutionary trade-offs, and complex adaptive systems.
By applying evolutionary principles to the very process of overcoming barriers to evolutionary medicine, we create a coherent framework for addressing the educational, professional, and systemic challenges documented across multiple studies. This approach recognizes that successful implementation requires not just evidence of efficacy but also alignment with human cognitive biases, motivational structures, and social dynamics—all products of our evolutionary history. The most promising path forward involves creating variation in educational and professional approaches, selecting what works in specific contexts, and retaining these successful strategies while maintaining the adaptability needed for future challenges. Through this evolutionary process, we may overcome the very barriers that currently limit the adoption of evolutionary perspectives in medicine.
Optimizing Prediction Algorithms with Evidence-Based Thresholds
The validation of evolutionary medicine approaches relies heavily on robust predictive algorithms. Evidence-based thresholds form the critical operating points within these algorithms, determining when a predicted risk is significant enough to trigger clinical actions or when a molecular characteristic indicates therapeutic potential. These thresholds balance sensitivity and specificity, directly impacting diagnostic accuracy and resource allocation in healthcare systems. Within evolutionary medicine, which seeks to understand disease through evolutionary principles, properly calibrated thresholds enable researchers to distinguish meaningful evolutionary signals from biological noise, thereby enhancing the translational value of predictive models.
The integration of evidence-based thresholds represents a paradigm shift from static, guideline-driven cutoffs to dynamic, data-informed decision points that reflect both biological principles and clinical realities. This comparative guide examines three distinct methodological frameworks for establishing these critical thresholds, evaluating their experimental foundations, performance characteristics, and applicability to evolutionary medicine research.
Comparative Analysis of Threshold Optimization Approaches
Table 1: Comparison of Evidence-Based Threshold Optimization Methodologies
| Methodology | Underlying Principle | Required Data | Key Outputs | Validation Approach |
|---|---|---|---|---|
| Clinician Behavior Learning [73] | Infers implicit decision thresholds from real-world treatment patterns | Retrospective EHR data, treatment decisions, risk scores | Aggregate majority vote threshold (50% treatment probability), Aggregate treatment rate threshold (population treatment rate) | Comparison with guideline recommendations; stability assessment post-guideline publication |
| Multi-Thresholding Meta-Algorithm (MTh) [74] [75] | Dynamically adjusts class probabilities using misclassification costs in multi-class settings | Imbalanced clinical datasets with multiple outcome classes | Cost-sensitive classification with optimized probability adjustments for minority classes | Total Cost metric incorporating misclassification consequences; comparison with traditional thresholding |
| Evolutionary Prompt Optimization (EMPOWER) [76] | Uses evolutionary algorithms to optimize LLM prompts for medical applications | Clinical vignettes across specialties, annotated physician responses | Optimized prompts with enhanced factual accuracy, domain specificity, and clinical relevance | Blinded clinician preference evaluations; reduction in factually incorrect content (24.7%) |
Table 2: Performance Metrics Across Threshold Optimization Methods
| Methodology | Quantitative Improvement | Clinical Acceptance | Handling of Data Imbalance | Computational Requirements |
|---|---|---|---|---|
| Clinician Behavior Learning [73] | Brier score: 0.159 (log-transformed equation); Identified thresholds: 3.6% (treatment rate) and 23.0% (majority vote) for statin prescribing | Reflects community standard of care; aligns with existing practice | Not explicitly addressed; assumes representative clinical data | Moderate (fitting decision-making equations to EHR data) |
| Multi-Thresholding Meta-Algorithm (MTh) [75] | Effectively handles class imbalance (e.g., 10% ICU, 17% mortality, 73% discharge in COVID-19 data) | Transparent and interpretable through Bayesian network explanations | Specifically designed for severe class imbalance | Low to moderate (wrapper approach that integrates with existing classifiers) |
| Evolutionary Prompt Optimization (EMPOWER) [76] | 24.7% reduction in factual errors, 19.6% improvement in domain specificity, 15.3% higher clinician preference | Highest blinded clinician preference ratings | Handles complexity stratification (straightforward to complex cases) | High (evolutionary algorithms with multiple evaluation dimensions) |
Experimental Protocols and Methodologies
Clinician Behavior Learning Protocol
The clinician behavior learning approach demonstrated by threshold learning for statin prescription follows a structured protocol [73]:
Data Collection and Cohort Definition
- Identify a retrospective cohort from electronic health records meeting specific clinical criteria (e.g., primary prevention patients without atherosclerotic disease or diabetes)
- Extract lipid screening events, subsequent statin prescriptions within 180 days, and demographic/clinical variables
- Ensure generalizability of risk stratification models (e.g., Pooled Cohort Equations) to the study population through discrimination measures (C-statistic = 0.71 in the referenced study)
Decision-Model Fitting
- Test alternative mathematical equations to describe relationship between risk scores and treatment probability:
- Linear form: P(treatment) = logistic(b₁ × PCEScore + b₂)
- Log-transformed form: P(treatment) = logistic(b₁ × log(PCEScore) + b₂)
- Select best-fitting model using Brier score (log-transformed form achieved 0.159 vs. 0.165 for linear)
- Extract decision thresholds from fitted model:
- Aggregate majority vote threshold: PCE risk score at 50% treatment probability
- Aggregate treatment rate threshold: PCE risk score at overall population treatment rate
Validation and Stability Assessment
- Compare learned thresholds with guideline-recommended values
- Assess temporal stability by evaluating threshold consistency before and after guideline publication
- Examine model performance in subgroup analyses and across different clinical settings
Figure 1: Clinician Behavior Learning Workflow
Multi-Thresholding Meta-Algorithm (MTh) Protocol
The MTh approach addresses multiclass imbalance in clinical prediction problems through the following experimental sequence [74] [75]:
Dataset Preparation and Imbalance Characterization
- Compile clinical dataset with multiple outcome classes (e.g., ICU admission, mortality, discharge for COVID-19 patients)
- Quantify class distribution and imbalance ratios (typically 10% ICU, 17% mortality, 73% discharge in referenced COVID-19 study)
- Partition data based on clinically relevant subgroups (e.g., patients with/without therapeutic limits)
Classifier Training and Probability Calibration
- Train multiple probabilistic classifiers (Naive Bayes, Neural Networks, Random Forests, SVM)
- Generate calibrated probability estimates for each class
- Establish baseline performance using conventional thresholding (typically 0.5 for binary, uniform for multiclass)
MTh Meta-Algorithm Implementation
- Define misclassification cost matrix reflecting clinical consequences of errors
- Apply MTh adjustment: Padjusted(classi) = P(classi) × factori
- Where factor_i is derived from probability distribution and misclassification costs
- Select final classification using maximum adjusted probability (MAP criterion)
Evaluation and Explanation
- Compare performance using Total Cost metric incorporating misclassification costs
- Construct Bayesian networks as explanatory models to interpret variable relationships
- Analyze how feature importance differs across patient subgroups (e.g., with/without therapeutic limits)
Figure 2: Multi-Thresholding Meta-Algorithm Process
EMPOWER Evolutionary Optimization Protocol
The EMPOWER framework implements a structured evolutionary approach to medical prompt optimization [76]:
Medical Domain Representation
- Implement medical terminology attention mechanism grounded in clinical ontologies
- Differentially weight medical concepts based on semantic importance
- Create specialized embedding space capturing clinical semantic relationships
Multi-Dimensional Assessment Architecture
- Evaluate prompts across four clinically critical dimensions:
- Structural clarity and specificity
- Domain specificity and terminology accuracy
- Clinical relevance and actionability
- Factual accuracy and evidence alignment
- Utilize board-certified physicians for annotation and evaluation
Component-Level Evolutionary Algorithm
- Initialize population of prompt variants across clinical specialties
- Apply structure-preserving crossover operations maintaining clinical reasoning patterns
- Implement mutation operators introducing medically valid variations
- Incorporate early stopping mechanisms and adaptive parameter tuning
Medical Semantic Verification
- Validate terminology usage against standardized medical lexicons (e.g., UMLS)
- Assess reasoning consistency with clinical guidelines
- Evaluate boundary statements according to responsible AI principles
- Integrate with evidence-based practice databases for factual verification
Blinded Clinical Evaluation
- Conduct comparative evaluations with clinicians rating output quality
- Measure reduction in factually incorrect content (24.7% improvement reported)
- Quantify enhancement in domain specificity (19.6% improvement reported)
- Assess overall clinician preference (15.3% higher preference reported)
Figure 3: EMPOWER Evolutionary Optimization Framework
Table 3: Key Research Reagent Solutions for Threshold Optimization Studies
| Resource Category | Specific Examples | Function in Research | Implementation Considerations |
|---|---|---|---|
| Clinical Datasets | Stanford Medicine Research Repository [73], MIMIC-III [76] | Provide real-world clinical data for model training and validation | Requires IRB approval; Data Use Agreements; De-identification protocols |
| Risk Calculation Tools | 2013 Pooled Cohort Equations (PCE) [73], Charlson Comorbidity Index [75] | Standardized risk assessment for cardiovascular and other clinical outcomes | Validation in target population essential; Consider calibration updates |
| Machine Learning Frameworks | Bayesian Networks [75], Random Forests, Neural Networks, SVM [74] | Enable development of predictive models with probability estimates | Choice depends on interpretability requirements and data characteristics |
| Evolutionary Algorithm Platforms | EMPOWER framework [76], Genetic Algorithm implementations | Optimize complex parameters through guided evolutionary search | Computational intensity varies; Parallelization often necessary |
| Medical Ontologies & Terminologies | UMLS (Unified Medical Language System) [76], Clinical ontologies | Standardize medical concepts for semantic verification | Mapping between different terminologies often required |
| Clinical Evaluation Resources | Board-certified physician annotators [76], Blinded evaluation protocols | Provide gold-standard assessments of clinical utility | Inter-rater reliability measurement; Adjudication processes for disagreements |
Discussion and Comparative Synthesis
Each threshold optimization methodology offers distinct advantages for evolutionary medicine applications. The clinician behavior learning approach provides naturally validated thresholds that reflect real-world practice patterns and demonstrate stability across temporal validation [73]. This method is particularly valuable for evolutionary medicine research seeking to understand how therapeutic decisions align with evolved biological risk factors.
The Multi-Thresholding Meta-Algorithm addresses the critical challenge of class imbalance frequently encountered in clinical datasets [74] [75]. Its cost-sensitive approach allows explicit incorporation of the evolutionary principle that different misclassification errors have asymmetric consequences for fitness and survival. The method's transparency through Bayesian network explanations facilitates biological interpretation of feature relationships.
The EMPOWER framework represents the most computationally sophisticated approach, achieving measurable improvements in factual accuracy and clinical preference [76]. Its evolutionary optimization process mirrors natural selection pressures, progressively refining prompts toward clinically optimal configurations. The structured preservation of clinical reasoning patterns ensures that evolutionary improvements maintain biological plausibility.
Across all methodologies, the transition from static to evidence-based dynamic thresholds enhances the biological validity of predictive models in evolutionary medicine. This alignment between computational optimization and evolved biological principles represents a promising direction for future research in personalized therapeutics and understanding of disease susceptibility.
Evidence and Efficacy: Validating Evolutionary Medicine Through Comparative Analysis
The field of evolutionary medicine is transforming therapeutic development by applying principles of natural selection to outmaneuver adaptive pathogens and cancer cells. This paradigm shift moves beyond traditional maximum-dose strategies toward dynamic, model-informed approaches that manage rather than attempt to eliminate disease populations. In oncology, Evolutionary Guided Precision Medicine (EGPM) leverages mathematical modeling to design therapy sequences that suppress resistant clones by maintaining sensitive competitors [57]. Similarly, infectious disease research employs evolutionary pharmacology to address antimicrobial resistance (AMR) through novel strategies like phage therapy and AI-driven drug discovery [77]. This guide provides a comparative analysis of clinical trial evidence, experimental protocols, and research tools validating these approaches across both therapeutic domains.
Comparative Clinical Trial Landscape
Current Evidence and Trial Designs
Clinical validation of evolutionary therapies employs distinct methodological frameworks in oncology versus infectious disease, reflecting their different pathophysiologies and resistance mechanisms.
Oncology: Trial designs increasingly incorporate mathematical models of clonal dynamics to guide adaptive therapy protocols. The pioneering clinical trial for metastatic castrate-resistant prostate cancer (mCRPC) used a dose-skipping protocol based on prostate-specific antigen (PSA) levels, reducing cumulative drug dose to 47% of standard while extending median time to progression from 14.3 to 33.5 months [32]. Ongoing trials for ovarian cancer (NCT05080556), BRAF mutant melanoma (NCT03543969), and basal cell carcinoma (NCT05651828) are testing similar adaptive paradigms [32].
Infectious Disease: Research focuses on circumventing antimicrobial resistance through novel therapeutic modalities and trial designs. Platform trials that test multiple treatments under a single protocol, exemplified by the RECOVERY trial during COVID-19, have improved efficiency for evaluating repurposed drugs and novel agents [78]. Phage therapy clinical trials target multi-drug resistant bacterial infections, with a Phase 1 trial for Pseudomonas aeruginosa in burn patients demonstrating both promise and challenges related to phage concentration and bacterial susceptibility [79].
Table 1: Comparative Clinical Trial Evidence for Evolutionary Therapies
| Aspect | Oncology | Infectious Disease |
|---|---|---|
| Validated Approaches | Adaptive Therapy (dose modulation/skipping) [32] | Phage Therapy, Platform Trials, AI-driven Drug Discovery [78] [79] |
| Key Trial Endpoints | Time to Progression, Cumulative Drug Dose [32] | Bacterial Burden Reduction, Morbidity/Mortality, Resistance Emergence [79] |
| Prominent Trial Results | mCRPC: 33.5 vs. 14.3 months progression-free with 47% drug reduction [32] | Phage therapy: Dramatic improvement in P. aeruginosa septicemia [79] |
| Ongoing Challenges | Reliable biomarkers for dynamic monitoring, clinician acceptance of models [32] | Predicting phage-bacteria interactions, commercial incentives for novel antibiotics [78] [79] |
Quantitative Evidence Synthesis
The clinical evidence base for evolutionary therapies, while growing, differs substantially in maturity and quantitative outcomes between fields.
Table 2: Quantitative Outcomes from Key Clinical Studies
| Therapy Area / Indication | Study Type | Primary Efficacy Metric | Evolutionary Therapy Result | Control / Standard of Care Result |
|---|---|---|---|---|
| Oncology: mCRPC [32] | Clinical Trial | Median Time to Progression | 33.5 months | 14.3 months |
| Oncology: mCRPC [32] | Clinical Trial | Cumulative Drug Dose | 47% reduction | Standard dosing |
| Infectious Diseases: R&D Efficiency [78] | Market Analysis | Drug Discovery Timeline | 60-70% reduction | Conventional timeline |
| Infectious Diseases: R&D Cost [78] | Market Analysis | Development Cost | 40% reduction | Conventional cost |
| Infectious Disease Trials Market [80] | Market Analysis | Annual Market Growth (CAGR) | 7.0% (2025-2029 forecast) | N/A |
Experimental Protocols for Evolutionary Therapy Validation
Adaptive Therapy Protocol for Solid Tumors
This methodology underpins the landmark mCRPC trial and subsequent oncology studies, using biomarker feedback to dynamically adjust treatment [32].
Objective: To evaluate whether dynamically adjusted therapy based on tumor burden biomarkers can extend time to progression and reduce total drug exposure compared to continuous maximum tolerated dose (MTD) therapy.
Materials:
- Patients with measurable metastatic cancer.
- A biomarker for tumor burden (e.g., PSA for prostate cancer, CT scans for tumor volume).
- Therapeutic agent(s) with a known resistance mechanism.
Procedure:
- Baseline Assessment: Obtain baseline measurement of the tumor burden biomarker.
- Initial Treatment Phase: Administer therapy at a standard dose until the tumor burden decreases by a predetermined threshold (e.g., 50% from baseline).
- Treatment Pause: Withhold therapy to allow tumor regrowth, driven by competition between drug-sensitive and drug-resistant cell populations.
- Biomarker Monitoring: Monitor the tumor burden biomarker at frequent, regular intervals (e.g., bi-weekly or monthly).
- Treatment Re-initiation: Resume therapy once the tumor burden returns to the original baseline level.
- Endpoint Determination: The primary endpoint is Time to Progression (TTP), defined as the point at which the tumor burden exceeds a pre-defined upper limit (e.g., 125-150% of baseline) despite active treatment.
Analysis: Compare TTP and cumulative drug dose between the adaptive therapy cohort and a historical or concurrent control cohort treated with continuous MTD.
Phage Therapy Protocol for Antibiotic-Resistant Infections
This protocol details the approach used in recent successful cases and clinical trials for treating multi-drug resistant bacterial infections [79].
Objective: To assess the safety and efficacy of bacteriophage cocktails in eradicating or reducing bacterial load in patients with infections resistant to conventional antibiotics.
Materials:
- Patient with a confirmed, multi-drug resistant bacterial infection.
- Library of characterized bacteriophages.
- In vitro susceptibility testing platform.
- Purified, sterile phage cocktail(s) targeting the specific bacterial strain.
Procedure:
- Pathogen Isolation and Identification: Isolate the bacterial pathogen from the patient and confirm its antibiotic resistance profile.
- Phage Susceptibility Screening: Screen the patient's bacterial isolate against a phage library to identify strains with high lytic activity.
- Cocktail Formulation: Prepare a therapeutic cocktail of multiple phages, often including a phage that targets specific resistance mechanisms (e.g., efflux pumps).
- Administration: Administer the phage cocktail via the appropriate route (e.g., intravenous for systemic infections, aerosolized for pulmonary infections, topical for wound infections).
- Concomitant Therapy (Optional): In some strategies, phage administration is followed by a previously ineffective antibiotic, once the phage has disabled the resistance mechanism [79].
- Monitoring: Monitor patient clinical status, bacterial load via culture, and inflammatory markers. Also monitor for the development of anti-phage antibodies.
- Endpoint Assessment: Primary endpoints include clearance of the bacteria from blood/tissue, clinical improvement, and survival.
Analysis: Evaluate microbiological cure rates, clinical outcomes, and safety profile in the study cohort.
The Scientist's Toolkit: Essential Research Reagents and Solutions
Validating evolutionary therapies requires specialized tools and reagents for modeling, monitoring, and analyzing dynamic disease responses.
Table 3: Key Research Reagent Solutions for Evolutionary Therapy Development
| Reagent / Solution | Field of Use | Function |
|---|---|---|
| Circulating Tumor DNA (ctDNA) Assays [36] | Oncology | Enables sensitive monitoring of tumor burden and clonal dynamics for adaptive therapy decision-making. |
| Mathematical Modeling Software (e.g., for ODE/PDE/ABMs) [32] | Oncology | Used to calibrate cancer dynamics models with patient data and simulate ECT protocols. |
| Bacteriophage Libraries [79] | Infectious Disease | Curated collections of phages used for screening against specific MDR bacterial pathogens to formulate personalized therapies. |
| AI/Machine Learning Platforms [78] [77] | Both | Accelerates drug discovery and repurposing; analyzes complex datasets (e.g., H&E slides, genomic data) to predict response/resistance. |
| Multi-objective Optimization Algorithms (e.g., MOSWO) [81] | Both | Computational tools that balance competing objectives (efficacy, toxicity, cost) to design optimal, patient-specific therapeutic regimens. |
Clinical validation of evolutionary therapies demonstrates their potential to overcome the fundamental challenge of treatment-induced resistance across oncology and infectious diseases. The evidence reveals that adaptive therapy protocols in cancer can significantly extend progression-free survival while reducing drug exposure and toxicity [32]. In infectious diseases, phage therapy and platform trials represent promising, evolution-informed strategies against AMR [78] [79]. The continued translation of these approaches relies on overcoming shared challenges: developing robust, real-time monitoring biomarkers, fostering interdisciplinary collaboration between clinicians and modelers, and building trust in model-informed treatment strategies [32]. The experimental protocols and research tools detailed herein provide a framework for researchers and drug development professionals to advance the clinical validation of these paradigm-shifting therapeutic strategies.
The foundational thesis of evolutionary medicine posits that many challenges in modern drug discovery, including antibiotic resistance and the difficulty in treating complex genetic disorders, can be addressed by understanding the evolutionary forces that shape pathogenic and human genomes [24]. The core principle is that proteins under strong evolutionary constraint—those evolving slowly due to purifying selection—are often critical for pathogen survival or cellular function, making them attractive therapeutic targets [82]. Mutations in these proteins are more likely to be deleterious and removed by selection, making them less susceptible to the random development of resistance [82]. This review validates this thesis by comparing the performance, applicability, and experimental validation of two primary computational methodologies used to identify these evolutionarily informed targets: comparative genomics and network-based approaches. We objectively evaluate their protocols, data requirements, and outputs to guide researchers in selecting the optimal strategy for their specific drug discovery pipeline.
Methodological Comparison: Core Approaches and Workflows
The two dominant in silico categories for therapeutic target identification are comparative genomics and network-based methods. Their rationales, optimal applications, and performance characteristics differ significantly, as summarized in Table 1.
Table 1: Comparative Performance of Evolutionary Target Identification Methods
| Feature | Comparative Genomics Approach | Network-Based Approach |
|---|---|---|
| Primary Rationale | Identifies essential, non-homologous genes in pathogens through cross-species genome comparison [83]. | Identifies central nodes in biological networks whose disruption impacts the entire system [83]. |
| Best Application | Infectious diseases; antibacterial and antiparasitic drug discovery [83]. | Non-infectious diseases; complex disorders (e.g., cancer, neurological diseases) [83]. |
| Target Characteristics | Essential for pathogen survival, conserved, and absent in the host [83] [82]. | Highly connected "hubs" (centrality) or nodes specific to a disease state (differentia) [83]. |
| Key Advantage | Directly minimizes host toxicity by filtering out human homologs [83]. | Can model complex disease biology and polypharmacology [83]. |
| Key Limitation | Primarily suited for infectious diseases, not complex human disorders [83]. | Target centrality in human networks can imply potential toxicity [83]. |
| Evolutionary Metric | Evolutionary rate (e.g., low dN/dS or pN/pS ratio) indicating purifying selection [82]. | Co-evolutionary signatures across a phylogenetic profile [84] [83]. |
The Comparative Genomics Workflow
This method is predominantly applied to infectious diseases. The workflow involves a sequential filtering process to pinpoint targets that are essential for the pathogen but absent in the host, thereby ensuring drug efficacy and safety [83]. The following diagram illustrates this multi-step workflow.
The Network-Based Workflow
Network-based methods operate on two main rationales: "centrality" (finding critical hubs in a single network) and "differentia" (finding differences between healthy and diseased networks) [83]. The following workflow outlines this process.
Experimental Validation and Performance Data
Validation through Evolutionary Rate Analysis
A key validation of the evolutionary medicine thesis comes from analyzing the evolutionary rates of known drug targets. A comprehensive study analyzed the pN/pS ratio (a measure of purifying selection) of genes from seven bacterial pathogens and E. coli. The results, shown in Table 2, demonstrate that known antibacterial drug targets evolve significantly more slowly than both the genome average and other essential genes, confirming that evolutionary rate is a powerful predictor of "drugability" [82].
Table 2: Evolutionary Rate Analysis of Bacterial Genes and Drug Targets
| Gene Set | Average pN/pS Ratio | Statistical Significance vs. All Genes | Statistical Significance vs. Essential Genes |
|---|---|---|---|
| All Genes | Baseline | N/A | N/A |
| Essential Genes | Lower than All Genes | p < 0.05 (FDR corrected) | N/A |
| Known Drug Targets | Lowest of all groups | p < 0.01 (FDR corrected) | p < 0.05 (FDR corrected) |
Validation through Phenotypic Rescue
Further validation comes from applied studies that transition from target identification to functional rescue. In a study on Rett syndrome, a comparative genomics approach using Normalized Phylogenetic Profiling (NPP) across 1028 eukaryotic genomes constructed an unbiased gene network for MECP2, the causative gene [84]. This method identified proteins with strong co-evolutionary signatures with MECP2, prioritizing three FDA-approved drug targets: IRAK, KEAP1, and EPOR [84].
Experimental Protocol: Cell-based Phenotypic Rescue Assay [84]
- Cell Models: Utilized human neural cell types, including microglia, astrocytes, and neural stem cells with MECP2 knock-down (KD) to model the disease.
- Intervention: The MECP2-KD cells were treated with drugs targeting the prioritized proteins: Pacritinib (targeting IRAK), Dimethyl Fumarate (DMF, targeting KEAP1), and Erythropoietin (EPO, targeting EPOR).
- Outcome Measurement: The ability of these drugs to rescue various phenotypic consequences of MECP2 inactivation was assessed. All three drugs were able to rescue different MECP2 inactivation phenotypes, and their action appeared to converge on modulating NF-κB signaling in inflammation [84].
The convergence of these evolutionarily informed targets on a common pathway, NF-κB, underscores the power of this approach to reveal core disease biology and identify druggable pathways, as illustrated below.
The Scientist's Toolkit: Essential Research Reagents and Databases
Successful implementation of the methodologies described above relies on a curated set of computational tools and databases. Table 3 lists key resources for conducting evolutionarily informed drug target discovery.
Table 3: Research Reagent Solutions for Evolutionary Target Identification
| Resource Name | Type | Primary Function in Workflow |
|---|---|---|
| KEGG Pathway Database [83] | Database | Collection of metabolic pathways used for the initial comparison of host and pathogen pathways. |
| UniProt [83] | Database | Repository of protein sequences used for retrieving sequences for BLAST analysis. |
| Database of Essential Genes (DEG) [83] [82] | Database | Catalog of genes essential for survival, used to validate the essentiality of candidate targets. |
| DrugBank [82] | Database | Repository of FDA-approved drug targets, used for validation and benchmarking of new predictions. |
| BLASTp [84] [83] | Software Tool | Performs protein-protein BLAST analysis to identify homologous sequences and filter out host homologs. |
| Normalized Phylogenetic Profiling (NPP) [84] | Software Pipeline | Quantifies gene co-evolution across hundreds of eukaryotic genomes to build functional gene networks. |
| segmeter [85] | Benchmarking Framework | Evaluates the performance of genomic interval query tools, which are fundamental for efficient genomic data analysis. |
| AIList & bedtk [85] | Software Tool | Efficient tools for querying and manipulating genomic intervals, crucial for handling large-scale genomic datasets. |
Validating Mismatch Hypotheses Through Cross-Cultural and Multi-Country Studies
Cross-cultural analysis provides a powerful methodological framework for testing evolutionary mismatch hypotheses, which postulate that modern environments differ from those in which humans evolved, leading to negative health outcomes [86]. By comparing diverse populations, researchers can determine if hypothesized relationships between ancestral traits and modern diseases hold across different cultural, ecological, and socioeconomic contexts. This approach moves beyond single-population studies to establish more robust, generalizable conclusions about human evolutionary adaptations and their mismatches with contemporary environments.
Core Methodological Framework for Cross-Cultural Validation
Validating mismatch hypotheses across cultures requires rigorous methodological approaches to ensure comparability of data across diverse populations. The following framework outlines essential steps for cross-cultural scale development and validation.
Table 1: Ten-Step Framework for Cross-Cultural Scale Development and Validation
| Stage | Step | Description | Key Techniques |
|---|---|---|---|
| Item Development | 1. Literature Review | Identify existing constructs and tools across cultures | Systematic reviews of validated instruments in different settings [87] |
| 2. Concept Elicitation | Explore cultural variations in construct understanding | Individual in-depth interviews with target populations in different countries [87] | |
| 3. Focus Group Discussions | Clarify shared and unique perspectives across cultures | Focus groups in different countries to explore cultural perspectives [87] | |
| 4. Expert Review | Ensure cross-cultural validity and translatability | Input from subject experts, measurement experts, and linguists [87] | |
| Translation | 5. Translation Protocol | Achieve linguistic and conceptual equivalence | Back-and-forth translation, collaborative team approaches [87] |
| 6. Expert Review | Verify translation quality and cultural relevance | Bilingual subject experts review translated items [87] | |
| Scale Development | 7. Cognitive Interviewing | Evaluate interpretation and acceptability | Pilot participants asked about understanding of items and response options [87] |
| 8. Local Adaptation | Adjust for contextual and logistical factors | Adapt recruitment strategies and incentives to local contexts [87] | |
| 9. Preliminary Validation | Test factor structure and reliability in each sample | Separate reliability tests and factor analysis in each cultural sample [87] | |
| Scale Evaluation | 10. Measurement Invariance Testing | Establish cross-cultural comparability | Multigroup confirmatory factor analysis, differential item functioning analysis [87] |
The sequential workflow for implementing this validation framework can be visualized as follows:
Advanced Statistical Approaches for Cross-Cultural Hypothesis Testing
Validating mismatch hypotheses requires sophisticated statistical methods that can account for cultural variability while testing core evolutionary predictions.
Table 2: Statistical Methods for Cross-Cultural Hypothesis Validation
| Method | Application in Mismatch Research | Key Features | Implementation Considerations |
|---|---|---|---|
| Sequential Testing | Early detection of sample ratio mismatches in experimental assignments | Allows testing after every datapoint while controlling Type-I error [88] | More practical than single chi-squared tests; enables early error detection [88] |
| Multigroup Confirmatory Factor Analysis (MGCFA) | Testing measurement invariance across cultural groups | Examines configural, metric, and scalar invariance; ΔCFI < 0.01 indicates invariance [87] | Requires large sample sizes; most commonly used invariance technique [87] |
| Differential Item Functioning (DIF) | Identifying culturally biased items in research instruments | Detects items functioning differently across subgroups under item response theory [87] | Useful for discovering which specific items are affected by cultural differences [87] |
| Multiple Indicator Multiple Causes (MIMIC) | Modeling direct effects of culture on latent constructs | Tests whether group membership affects item responses while measuring same construct [87] | Efficient for testing impact of multiple cultural variables on measurement [87] |
The relationship between these statistical approaches and their application to hypothesis validation is structured as follows:
Essential Research Toolkit for Cross-Cultural Evolutionary Medicine
Implementing robust cross-cultural studies requires specific methodological tools and approaches tailored to evolutionary medicine research.
Table 3: Research Reagent Solutions for Cross-Cultural Mismatch Studies
| Research Tool | Function | Application Example | Implementation Notes |
|---|---|---|---|
| Sequential Statistical Tests | Continuously monitor data quality during collection | Detect sample ratio mismatches in experimental assignments early [88] | Controls Type-I error regardless of number of tests performed [88] |
| Cognitive Interview Protocols | Evaluate participant understanding of items | Test cultural interpretation of health behavior questions [87] | Participants explain understanding of each item and response options [87] |
| Back-Translation Protocols | Ensure linguistic and conceptual equivalence | Translate mismatch hypothesis measures between languages [87] | Forward translation, back-translation, comparison, inconsistency resolution [87] |
| Measurement Invariance Analysis | Establish cross-cultural comparability of constructs | Test if mismatch constructs measured equivalently across cultures [87] | Uses multigroup confirmatory factor analysis with specific fit indices [87] |
| Case-Profile Plots | Visualize within-individual changes across measurements | Display individual trajectories in longitudinal mismatch studies [89] | Shows measurements for each individual across multiple time points [89] |
| Comparative Numerical Summaries | Quantify differences between cultural groups | Present mean differences in health outcomes across populations [90] | Includes means, standard deviations, and sample sizes for each group [90] |
Data Visualization Strategies for Cross-Cultural Comparison
Effective data presentation is crucial for communicating complex cross-cultural findings in evolutionary mismatch research.
Table 4: Data Visualization Methods for Cross-Cultural Mismatch Research
| Visualization Type | Best Use Cases | Advantages | Limitations |
|---|---|---|---|
| Case-Profile Plots | Within-individual changes across multiple measurements [89] | Shows individual trajectories while highlighting group patterns [89] | Can become cluttered with large numbers of individuals [89] |
| Back-to-Back Stemplots | Comparing two groups with small datasets [90] | Retains original data values; clear comparison of two distributions [90] | Only suitable for two groups; not for large datasets [90] |
| Boxplots | Comparing distributions across multiple cultural groups [90] | Summarizes distributions using five-number summary; handles outliers well [90] | Loses detail of actual distribution shape [90] |
| Histograms of Differences | Visualizing within-individual change between two time points [89] | Shows distribution of change scores clearly [89] | Only appropriate for two measurements per individual [89] |
| 2-D Dot Charts | Comparing multiple groups with small to moderate data [90] | Shows individual data points while comparing groups; any number of groups [90] | Requires jittering or stacking when points have same values [90] |
The methodological framework presented here provides a comprehensive approach for validating evolutionary mismatch hypotheses across diverse cultural contexts. By implementing rigorous scale development procedures, advanced statistical tests for measurement invariance, and appropriate data visualization techniques, researchers can generate more robust evidence about human evolutionary adaptations and their mismatches with modern environments. This systematic approach to cross-cultural comparison addresses fundamental challenges in evolutionary medicine while providing tools to test core theoretical predictions across diverse human populations.
Microevolutionary validation represents a critical approach in evolutionary medicine, focusing on observable, generation-to-generation changes in human biology to understand contemporary health challenges. Unlike theoretical models of ancient human evolution, this field empirically tracks shifts in gene frequencies, anatomical structures, and disease susceptibility within human populations over historical timeframes [91]. These changes result from evolutionary forces—natural selection, gene flow, genetic drift, and mutations—operating within modern human populations, often with direct implications for disease treatment and prevention [92]. The validation of these microevolutionary patterns provides a evidence-based framework for interpreting why humans remain vulnerable to specific diseases despite medical advances and how medical interventions themselves might influence future human biology.
The foundational principle of microevolutionary validation rests on documented changes in human gene pools. Research indicates that the opportunity for natural selection through differential mortality has severely reduced in the last 150 years, with over 90% of newborns now surviving to reproductive age compared to approximately 50% before the mid-19th century [91]. This relaxation of selective pressures has predictable outcomes, including increased variability of heritable traits as stabilizing selection diminishes [91]. Simultaneously, human microevolution has accelerated due to rapid population growth facilitated by cultural and technological development, creating medically relevant biological changes observable within just a few generations [91].
Documented Microevolutionary Changes with Health Implications
Anatomical and Physiological Shifts
Microevolutionary validation studies have quantified significant alterations in human anatomy across recent generations, with direct consequences for medical practice. These changes are documented through comparative analysis of historical and contemporary population data.
Table 1: Documented Anatomical Changes in Human Populations
| Anatomical Structure | Documented Change | Time Frame | Proposed Evolutionary Mechanism | Medical Relevance |
|---|---|---|---|---|
| Median Artery of Forearm | Prevalence increased from ~10% to ~30% | 20th century [91] | Relaxed natural selection [91] | Surgical planning, vascular procedures |
| Thyroidea Ima Artery | Complete disappearance | By end of 20th century [91] | Relaxed natural selection [91] | Surgical risk in neck procedures |
| Sacral Canal (Spina Bifida Occulta) | Increased prevalence | Cohorts born in second half of 20th century [91] | Relaxed natural selection [91] | Neurological assessment, congenital disorders |
| Jaw Size and Dentition | Reduction in size and number of teeth [91] | Historical times to present [91] | Technological change (reduced chewing effort) [91] | Orthodontics, dental crowding, impaction |
| Cranial Morphology | Microcranialization and brachycephalization [91] | Historical times to present [91] | Gracilization of musculoskeletal system [91] | Neurological assessment, surgical planning |
Metabolic and Immunological Adaptations
Beyond anatomical changes, microevolutionary validation tracks functional adaptations with profound health implications. These include well-documented cases of lactose tolerance persistence into adulthood and variations in ethanol processing capabilities, which represent adaptations to cultural developments like dairy farming and fermented beverage production [91]. Additionally, the evolution of immunity to infectious diseases demonstrates ongoing host-pathogen coevolution, while the development of insecticide resistance in mosquitoes and antibiotic resistance in pathogens like Staphylococcus aureus and Mycobacterium tuberculosis represents medically critical microevolution observed in real-time [92]. These validated examples provide crucial models for understanding disease mechanisms and developing intervention strategies.
Experimental Protocols for Microevolutionary Tracking
Genotype-Phenotype Association Studies
Tracking microevolutionary changes requires robust methodologies that correlate genetic changes with phenotypic expressions across generations. The following experimental protocol provides a standardized approach for validating these associations.
Table 2: Experimental Protocol for Genotype-Phenotype Association Studies
| Research Phase | Key Activities | Data Collection Methods | Output Metrics |
|---|---|---|---|
| Sample Collection | Multi-generational sampling; Historic tissue analysis [91] | Archaeological specimens; Medical records; Biobanks [91] | Temporal sample series; Pedigree data |
| Genomic Analysis | Genome-wide association studies (GWAS); Sequencing [93] | Genotyping arrays; Whole genome sequencing; Functional genomics [93] | Allele frequency changes; Identification of causal variants [93] |
| Phenotypic Assessment | Anatomical measurement; Metabolic profiling; Disease mapping [91] | Medical imaging; Physiological tests; Health records | Quantitative trait variation; Disease prevalence rates |
| Statistical Validation | Quantitative trait locus (QTL) analysis; Allelic imbalance assessment [93] | Measurement of Allelic Ratios Informatics Operator (MARIO) [93] | Statistically significant associations; Effect size estimates |
Diagram 1: Genotype-Phenotype Association Workflow
Longitudinal Population Health Monitoring
An alternative approach tracks health parameter changes across birth cohorts using longitudinal data, which is particularly valuable for identifying evolutionary mismatches between ancestral environments and modern conditions [26]. This method employs retrospective analysis of health records, cross-sectional population studies at different time points, and systematic analysis of ancestral versus modern disease prevalence patterns. Specific applications include documenting increased prevalence of metabolic disorders like type 2 diabetes in populations experiencing rapid nutritional transitions and monitoring mental health patterns in novel environments like space, where conditions create evolutionary mismatches affecting neuro-behavioral function [26].
Analytical Tools for Microevolutionary Research
Statistical and Computational Methods
Validating microevolutionary changes requires specialized analytical approaches capable of distinguishing true evolutionary shifts from transient environmental effects or measurement artifacts.
Table 3: Analytical Methods for Microevolutionary Validation
| Method Category | Specific Techniques | Application in Microevolution | Key Outputs |
|---|---|---|---|
| Population Genetics Analysis | Hardy-Weinberg equilibrium testing; F-statistics [92] | Detect evolutionary forces operating on populations [92] | Quantification of selection, drift, gene flow |
| Association Mapping | Genome-wide association studies (GWAS); Quantitative trait locus (QTL) analysis [93] | Identify genetic variants underlying trait changes [93] | Statistical associations between genotypes and phenotypes |
| Temporal Series Analysis | Cohort comparison; Ancient DNA analysis [91] | Track allele frequency changes across generations [91] | Documented microevolutionary trajectories |
| Functional Validation | CRISPR/Cas9 editing; Cell culture models; Organoids [93] | Establish causal mechanisms for identified variants [93] | Biological validation of genotype-phenotype links |
Gene-Environment Interaction Models
A sophisticated understanding of G×E interactions is essential for microevolutionary validation, as these interactions determine how genetic predispositions manifest in different environmental contexts [93] [94]. Statistical models for detecting G×E interactions must account for scale of measurement—additive versus multiplicative effects—with the choice of model depending on research objectives and the hypothesized pathophysiological mechanism [94]. Well-established examples include the role of skin barrier gene mutations (e.g., filaggrin) in atopic dermatitis, where environmental factors like skin microbiota interact with genetic susceptibility to determine disease expression [93].
Diagram 2: Gene-Environment Interaction Model
Core Research Reagent Solutions
Table 4: Essential Research Reagents for Microevolutionary Studies
| Reagent Category | Specific Examples | Research Function | Application Examples |
|---|---|---|---|
| Genomic Analysis Tools | GWAS arrays; Whole genome sequencing kits; Targeted sequencing panels [93] | Genotype generation and variant identification | Mapping allele frequency changes; Identifying selection signatures |
| Functional Assays | CRISPR/Cas9 systems; Reporter constructs; Chromatin immunoprecipitation (ChIP) reagents [93] | Mechanistic validation of genetic variants | Testing regulatory function of non-coding variants; Gene editing of candidate alleles |
| Epigenetic Profiling | Bisulfite conversion kits; Methylation arrays; Histone modification antibodies [93] | Assessment of epigenetic modifications | Studying environmental influences on gene expression; Transgenerational epigenetic inheritance |
| Pathogen Evolution Tools | Antimicrobial susceptibility testing; Microbial sequencing; Culture media [91] [92] | Tracking pathogen adaptation | Monitoring antibiotic resistance development; Studying host-pathogen coevolution |
Comparative Analysis of Microevolution in Biomedical Contexts
Validation Across Disease Models
Microevolutionary validation provides evidence-based insights across multiple disease domains, with applications ranging from infectious disease to chronic conditions. The comparative framework below highlights how microevolutionary principles operate across different health contexts.
Table 5: Microevolutionary Validation Across Disease Models
| Disease Category | Microevolutionary Process | Documented Evidence | Research/Clinical Implications |
|---|---|---|---|
| Infectious Diseases | Pathogen resistance evolution [92] | Antibiotic resistance in bacteria (e.g., gonorrhea, TB); Antiviral resistance in HIV [92] | Rational drug rotation; Combination therapies; Novel antimicrobial targets |
| Metabolic Disorders | Relaxed selection on thrifty genotypes [91] [26] | Increased type 2 diabetes prevalence in nutritionally transitioned populations [26] | Personalized nutrition; Early intervention strategies; Public health planning |
| Anatomical Disorders | Increased anatomical variation [91] | Higher prevalence of previously rare arterial patterns [91] | Surgical training updates; Refined anatomical reference standards |
| Mental Health | Evolutionary mismatch in novel environments [26] | Increased neuro-behavioral issues in extreme environments (e.g., space) [26] | Environmental design; Preventive mental health strategies |
Microevolutionary validation provides an empirical foundation for evolutionary medicine by documenting and quantifying biological changes across generations. The methodologies, analytical frameworks, and research tools outlined in this guide enable researchers to move beyond theoretical speculation to evidence-based understanding of how human biology continues to change in response to modern environments and medical practices. As precision medicine advances, incorporating this evolutionary perspective becomes increasingly vital for developing effective, forward-looking therapeutic strategies that account for our dynamically changing biology. The continued validation of microevolutionary patterns will undoubtedly shape future drug development, public health planning, and clinical practice by providing critical insights into the ongoing relationship between human evolution and health.
Evolutionary medicine, the application of modern evolutionary theory to understanding health and disease, provides a powerful framework for explaining why humans remain vulnerable to certain pathological conditions [2]. This rapidly growing field examines disease through the lens of evolutionary processes including natural selection, genetic drift, trade-offs, and phylogenetic constraints [6]. As research in evolutionary medicine expands, the volume of scientific literature has grown exponentially, creating both opportunities and challenges for researchers and drug development professionals. The ability to synthesize collective evidence through systematic methodologies has become increasingly critical for validating evolutionary medicine approaches and translating theoretical insights into clinical applications.
Systematic reviews and meta-analyses represent the pinnacle of evidence-based research, offering rigorous methods for aggregating, appraising, and synthesizing scientific findings [95] [96]. These methodologies occupy a unique position in the hierarchy of evidence, as they can systematically consolidate diverse studies on evolutionary medicine topics ranging from pathogen resistance and cancer evolution to evolutionary mismatches and life-history trade-offs [55]. For researchers validating evolutionary medicine approaches, these evidence-synthesis methods provide powerful tools for distinguishing robust evolutionary explanations from speculative just-so stories, thereby strengthening the scientific foundation of the field and guiding future research directions.
Fundamental Concepts: Systematic Reviews vs. Meta-Analyses
Defining the Methodologies
A systematic review is a comprehensive, structured approach to identifying, evaluating, and synthesizing all available evidence pertinent to a specific research question [95] [97]. It employs explicit, reproducible methods designed to minimize bias, providing reliable findings from which conclusions can be drawn and decisions made. The systematic review process is characterized by clearly stated objectives with pre-defined eligibility criteria, an exhaustive search strategy, systematic assessment of study validity, and structured presentation of characteristics and findings of included studies [96].
A meta-analysis is a statistical technique for quantitatively combining and analyzing results from multiple independent studies on a similar topic to generate an overall estimate of the studied phenomenon [97]. This approach uses formal epidemiological study designs to systematically combine pertinent qualitative and quantitative study data from several included studies, thereby enhancing statistical power and precision of effect estimates [98]. Meta-analysis examines heterogeneity between studies and can explore subgroups that may not reach statistical significance in individual studies.
Comparative Analysis of Approaches
Table 1: Key Differences Between Systematic Reviews and Meta-Analyses
| Feature | Systematic Review | Meta-Analysis |
|---|---|---|
| Primary purpose | Gather and critically appraise all relevant research | Provide a precise mathematical estimate of effect size |
| Nature of analysis | Primarily qualitative synthesis | Primarily quantitative statistical analysis |
| Study requirements | Can include diverse study designs | Requires studies with compatible numerical data |
| Methodological approach | Comprehensive and inclusive of all relevant evidence | Selective based on statistical compatibility |
| Output format | Text summary, evidence tables, narrative synthesis | Forest plots, pooled effect sizes, confidence intervals |
| Time requirement | 6-12 months typically | 9-18 months (includes systematic review phase) |
| Expertise required | Literature searching, critical appraisal | Statistical methods, effect size calculation |
While systematic reviews and meta-analyses are distinct methodologies, they are often employed together in a complementary fashion [95]. A systematic review may stand alone with a narrative synthesis, or it may incorporate a meta-analysis if the included studies are sufficiently homogeneous in their outcomes and measures [97]. The decision to conduct a meta-analysis depends on the research question, the intervention being studied, the desired outcomes, and the compatibility of data across available studies [96].
Methodological Frameworks: Protocols and Procedures
Systematic Review Workflow
The process of conducting a systematic review follows a structured, multi-stage protocol that enhances reproducibility and minimizes bias. The following diagram illustrates the key stages in this workflow:
Figure 1: Systematic Review Workflow: Sequential stages from question formulation to reporting.
The systematic review process typically encompasses these essential steps [95] [96]:
Formulate a clear research question: Using frameworks like PICO (Population, Intervention, Comparison, Outcome) to define the scope and boundaries of the review.
Develop a detailed protocol: Creating a comprehensive plan that outlines methods before commencing the review, including eligibility criteria and search strategies.
Conduct comprehensive literature search: Searching multiple databases, journals, gray literature, and reference lists using carefully crafted search strategies to identify all relevant studies.
Screen and select studies: Applying predefined inclusion/exclusion criteria through a structured process typically involving multiple independent reviewers to determine which studies qualify.
Extract data systematically: Collecting relevant information from each included study using standardized forms or data extraction tools.
Assess study quality and risk of bias: Evaluating methodological rigor of included studies using validated critical appraisal tools.
Synthesize evidence: Combining results either narratively (qualitative synthesis) or, when appropriate, statistically (meta-analysis).
Report findings: Documenting results following established guidelines like PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses).
Meta-Analysis Statistical Framework
The statistical procedures of meta-analysis build upon the systematic review process, adding quantitative synthesis methods as illustrated below:
Figure 2: Meta-Analysis Statistical Framework: Key analytical steps for quantitative synthesis.
The meta-analysis component involves these key statistical procedures [95] [97]:
Effect size calculation: Deriving comparable effect measures (e.g., odds ratios, risk ratios, mean differences) from each included study.
Model selection: Choosing between fixed-effect models (assuming a single true effect size) or random-effects models (assuming effect sizes vary between studies).
Weighting studies: Assigning weights to studies, typically based on precision (inverse variance), giving more influence to larger studies.
Pooling effects: Combining effect sizes across studies to generate an overall estimate with confidence intervals.
Heterogeneity assessment: Quantifying between-study variation using statistics like I² and Q-test.
Sensitivity and subgroup analyses: Exploring sources of heterogeneity and testing robustness of findings.
Publication bias evaluation: Assessing potential bias from unpublished studies using funnel plots and statistical tests.
Applications in Evolutionary Medicine Research
Validating Core Evolutionary Medicine Concepts
Systematic reviews and meta-analyses provide powerful methodological tools for testing and validating fundamental principles in evolutionary medicine. The 14 core principles of evolutionary medicine identified through expert consensus [6] provide a framework for research questions amenable to evidence synthesis. These principles include evolutionary trade-offs, life history theory, defense mechanisms, and evolutionary mismatches between ancestral and modern environments [2] [6].
For example, the "mismatch" concept posits that many modern diseases arise from disparities between contemporary environments and those in which humans evolved [2] [55]. Systematic reviews can synthesize evidence testing this concept across multiple health domains, including obesity, metabolic syndrome, autoimmune diseases, and mental health conditions. Similarly, the principle of "evolutionary trade-offs" suggests that adaptations enhancing fitness in one context may increase disease vulnerability in another [2] [99]. Meta-analyses can quantitatively evaluate evidence for proposed trade-offs, such as the relationship between immune function and energy allocation or between reproductive investment and longevity.
Case Study: AI Diagnostic Performance in Evolutionary Context
A recent systematic review and meta-analysis of generative AI models for diagnostic tasks exemplifies the application of these methodologies in medically relevant evolutionary contexts [100]. This comprehensive analysis of 83 studies published between 2018-2024 revealed an overall diagnostic accuracy of 52.1% for AI models, with no significant performance difference compared to physicians overall (p=0.10) or to non-expert physicians specifically (p=0.93). However, AI models performed significantly worse than expert physicians (p=0.007), highlighting the value of evolved human expertise and pattern recognition.
Table 2: Performance Comparison of AI Models vs. Physicians in Diagnostic Tasks
| Comparison Group | Number of Studies | Performance Outcome | Statistical Significance |
|---|---|---|---|
| All physicians | 17 | No significant difference | p = 0.10 |
| Non-expert physicians | Multiple | No significant difference | p = 0.93 |
| Expert physicians | Multiple | AI performed significantly worse | p = 0.007 |
| Overall AI accuracy | 83 | 52.1% | N/A |
From an evolutionary medicine perspective, these findings illuminate the cognitive adaptations underlying diagnostic expertise. The superior performance of expert physicians suggests the value of evolved human cognitive capacities, including intuition, contextual reasoning, and holistic pattern recognition - capabilities shaped by natural selection that artificial systems have not yet fully replicated. This evidence synthesis approach provides a robust methodology for evaluating how technological innovations interface with human evolutionary adaptations in healthcare contexts.
Essential Research Reagents and Tools
Methodological Reagents for Evidence Synthesis
Table 3: Essential Research Reagents for Systematic Reviews and Meta-Analyses
| Research Reagent | Function | Application Context |
|---|---|---|
| PRISMA Guidelines | Standardized reporting framework for systematic reviews and meta-analyses | Ensuring comprehensive and transparent reporting of methods and findings |
| PICO Framework | Structured approach for formulating research questions (Population, Intervention, Comparison, Outcome) | Defining review scope and developing search strategies |
| Electronic Databases | Platforms for comprehensive literature searching (e.g., MEDLINE, EMBASE, CENTRAL) | Identifying published studies through systematic search strategies |
| Gray Literature Sources | Unpublished or non-commercially published materials (e.g., dissertations, clinical trial registries) | Minimizing publication bias by including studies beyond traditional publications |
| Risk of Bias Tools | Standardized instruments for assessing methodological quality (e.g., Cochrane RoB, Newcastle-Ottawa Scale) | Critical appraisal of included studies' validity |
| Statistical Software Packages | Programs for meta-analytic computations (e.g., R metafor, RevMan, Stata metan) | Conducting quantitative synthesis and generating forest plots |
| GRADE Approach | System for rating quality of evidence and strength of recommendations | Translating systematic review findings into clinical and research implications |
These methodological reagents provide the essential infrastructure for conducting rigorous evidence syntheses in evolutionary medicine. The PRISMA guidelines ensure comprehensive reporting, while structured frameworks like PICO facilitate precise question formulation [95] [96]. Comprehensive search strategies incorporating multiple electronic databases and gray literature sources help minimize selection bias and publication bias [96]. Validated risk of bias tools enable critical appraisal of included studies, while specialized statistical software facilitates the quantitative synthesis central to meta-analysis [97]. Finally, the GRADE approach provides a systematic method for translating evidence synthesis findings into clinical and research implications relevant to evolutionary medicine.
Experimental Protocols for Evidence Synthesis
Protocol for Systematic Review in Evolutionary Medicine
Objective: To systematically identify, evaluate, and synthesize evidence testing evolutionary medicine hypotheses regarding disease vulnerability, adaptation, or treatment response.
Eligibility Criteria:
- Population: Human, animal model, or pathogen populations relevant to evolutionary medicine hypotheses
- Intervention/Exposure: Evolutionary factors (e.g., life history variables, ecological mismatches, phylogenetic constraints)
- Comparators: Appropriate control groups or alternative evolutionary scenarios
- Outcomes: Disease incidence, prevalence, severity, or treatment response metrics
- Study Designs: Randomized trials, observational studies, comparative phylogenetic analyses, or experimental evolution studies
Search Strategy:
- Develop search syntax using Boolean operators and database-specific filters
- Search multiple electronic databases (e.g., MEDLINE, EMBASE, Web of Science, Evolutionary Medicine-specific resources)
- Supplement with gray literature searches (clinical trial registries, dissertation databases, conference abstracts)
- Implement citation chasing (screening reference lists of included studies and relevant reviews)
- Apply no language or date restrictions where possible
Study Selection Process:
- Implement dual-independent screening at title/abstract and full-text stages
- Resolve conflicts through consensus or third-party adjudication
- Document reasons for exclusion at full-text stage
- Manage process using reference management software and systematic review platforms
Data Extraction:
- Develop standardized data extraction forms
- Extract study characteristics (design, population, methods)
- Extract outcome data and effect measures
- Collect data on potential effect modifiers (e.g., age, sex, environmental factors)
Risk of Bias Assessment:
- Apply appropriate critical appraisal tools for different study designs
- Evaluate key bias domains (selection, performance, detection, attrition, reporting)
- Consider evolutionary-specific methodological limitations
Protocol for Meta-Analysis in Evolutionary Medicine
Statistical Analysis Plan:
- Effect measure selection: Choose appropriate effect sizes (odds ratios, risk ratios, mean differences, correlation coefficients) based on outcome type and study design
- Data transformation: Convert reported statistics to uniform effect sizes and variances using standard formulas
- Model selection: Determine fixed-effect vs. random-effects model based on heterogeneity assessment and conceptual framework
- Heterogeneity quantification: Calculate I² statistic and confidence intervals to estimate proportion of total variation due to between-study differences
- Sensitivity analyses: Test robustness of findings to methodological decisions, inclusion criteria, and statistical models
- Subgroup analyses and meta-regression: Explore potential sources of heterogeneity using study-level characteristics (e.g., population attributes, methodological features)
- Publication bias assessment: Implement funnel plots, Egger's test, and trim-and-fill analysis to evaluate potential bias from unpublished studies
Interpretation Framework:
- Consider biological and evolutionary plausibility of findings
- Evaluate consistency with evolutionary theory and existing evidence
- Assess limitations related to included studies and methodological constraints
- Identify implications for evolutionary medicine theory and future research directions
Systematic reviews and meta-analyses provide indispensable methodological tools for validating evolutionary medicine approaches and synthesizing collective evidence across diverse research paradigms. These rigorous evidence-synthesis methodologies enable researchers to distinguish well-supported evolutionary explanations from speculative accounts, assess the consistency of findings across studies, quantify effect sizes, and identify sources of heterogeneity. By applying these approaches to core evolutionary medicine concepts—including evolutionary mismatches, trade-offs, life history theory, and phylogenetic constraints—researchers can strengthen the empirical foundation of the field and guide future research directions.
For drug development professionals and translational researchers, systematic reviews and meta-analyses offer powerful approaches for evaluating evolutionary perspectives on treatment efficacy, resistance evolution, and personalized medicine applications. The integration of these evidence-synthesis methodologies with evolutionary frameworks promises to enhance our understanding of disease vulnerability, treatment response, and health optimization across diverse populations and environmental contexts. As evolutionary medicine continues to mature as a discipline, systematic reviews and meta-analyses will play an increasingly vital role in consolidating knowledge, validating theoretical models, and translating evolutionary insights into clinical applications.
Conclusion
The validation of evolutionary medicine represents a paradigm shift in biomedical science, offering powerful frameworks for understanding disease etiology and developing innovative therapies. The convergence of foundational evolutionary principles with rigorous methodological applications demonstrates significant potential in addressing pressing medical challenges, particularly in antimicrobial resistance and cancer treatment. However, realizing this potential requires systematic efforts to overcome implementation barriers through enhanced interdisciplinary collaboration, refined educational curricula, and increased engagement from clinicians and policymakers. Future directions should prioritize large-scale clinical trials, the development of phylogenetically-informed databases, and the integration of evolutionary concepts with emerging technologies like artificial intelligence and precision medicine. By embracing these evidence-based evolutionary approaches, the biomedical community can spark transformational innovation in drug development and clinical practice, ultimately improving outcomes for human, animal, and planetary health.
References
- 1. The great opportunity: Evolutionary applications to medicine and public health - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3352398/]
- 2. Evolutionary medicine - Wikipedia [https://en.wikipedia.org/wiki/Evolutionary_medicine]
- 3. Evolutionary cardiology and experimental research - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9262302/]
- 4. Evolutionary Medicine - an overview | ScienceDirect Topics [https://www.sciencedirect.com/topics/medicine-and-dentistry/evolutionary-medicine]
- 5. Frontiers | The future of evolutionary : sparking innovation in... medicine [https://www.frontiersin.org/journals/science/articles/10.3389/fsci.2023.997136/full]
- 6. Core principles of evolutionary medicine: A Delphi study - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC5822696/]
- 7. Leveraging Comparative Phylogenetics for Evolutionary ... Medicine [https://pmc.ncbi.nlm.nih.gov/articles/PMC11844554/]
- 8. Editorial: evolutionary medicine special issue - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC3352418/]
- 9. Applying an evolutionary framework to understand mismatch ... disease [https://journals.plos.org/plosbiology/article?id=10.1371/journal.pbio.3002311]
- 10. How modern life makes us sick – and what to do about it | Evolution [https://www.theguardian.com/books/2025/sep/21/how-modern-life-makes-us-sick-and-what-to-do-about-it]
- 11. mismatch - PMC Evolutionary [https://pmc.ncbi.nlm.nih.gov/articles/PMC6109377/]
- 12. Stranger in a strange land: an optimal- environments account of... [https://link.springer.com/article/10.1007/s11229-018-01915-x]
- 13. Frontiers | Postmodern evolutionary framework for chronic diseases ... [https://www.frontiersin.org/journals/ecology-and-evolution/articles/10.3389/fevo.2025.1608810/full]
- 14. Comparative performance of viral landscape phylogeography approaches - PubMed [https://pubmed.ncbi.nlm.nih.gov/40569388/]
- 15. - Nature’s roadmap to insights and solutions for burden of... Biomimetics [https://pmc.ncbi.nlm.nih.gov/articles/PMC7035180/]
- 16. Integrated Biomimetics: Natural Innovations for Urban Design, Smart Technologies, and Human Health [https://www.mdpi.com/2076-3417/15/13/7323]
- 17. physiology and Comparative in metabolic and... biomimetics [https://link.springer.com/article/10.1007/s00125-025-06611-3]
- 18. Frontiers | Microbiome engineering to enhance disease in... resistance [https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2025.1625265/full]
- 19. Life History Evolution | Learn Science at Scitable [https://www.nature.com/scitable/knowledge/library/life-history-evolution-68245673/]
- 20. Diametrical diseases reflect evolutionary-genetic tradeoffs [https://pmc.ncbi.nlm.nih.gov/articles/PMC4600345/]
- 21. The challenge of measuring trade-offs in human life history ... [https://www.sciencedirect.com/science/article/pii/S1090513820301185]
- 22. The influence of evolutionary history on human health and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7787134/]
- 23. Life History Trait - an overview [https://www.sciencedirect.com/topics/medicine-and-dentistry/life-history-trait]
- 24. Research: Evolutionary medicine [https://elifesciences.org/articles/69398]
- 25. The evolution of health data ecosystems: An international ... [https://www.sciencedirect.com/science/article/pii/S0002929725002484]
- 26. Frontiers | Evolutionary and bioastronautics: an innovative... medicine [https://www.frontiersin.org/journals/physiology/articles/10.3389/fphys.2025.1558625/full]
- 27. contributes to global obesity increase more... Relaxed natural selection [https://pubmed.ncbi.nlm.nih.gov/30021019/]
- 28. An evolutionary medicine and life history perspective on aging and disease: Trade-offs, hyperfunction, and mismatch - PubMed [https://pubmed.ncbi.nlm.nih.gov/40574888/]
- 29. Relaxed Selection During a Recent Human Expansion - PubMed [https://pubmed.ncbi.nlm.nih.gov/29187508/]
- 30. The evolutionary theory of cancer ... | Nature Reviews Cancer [https://www.nature.com/articles/s41568-024-00734-2?error=cookies_not_supported]
- 31. Eradicating Metastatic Cancer and the Eco-Evolutionary Dynamics of Anthropocene Extinctions - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7771333/]
- 32. Bringing evolutionary cancer therapy to the clinic: a systems approach | npj Systems Biology and Applications [https://www.nature.com/articles/s41540-025-00528-8]
- 33. Preventing evolutionary rescue in cancer - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10690287/]
- 34. Threshold-awareness in adaptive cancer therapy [https://journals.plos.org/ploscompbiol/article?id=10.1371/journal.pcbi.1012165]
- 35. Tumor evolution predict recurrence beyond 10 years in locally... metrics [https://pmc.ncbi.nlm.nih.gov/articles/PMC11424488/]
- 36. Experts Forecast Cancer Research and Treatment Advances in 2025 [https://www.aacr.org/blog/2025/01/10/experts-forecast-cancer-research-and-treatment-advances-in-2025/]
- 37. The Evolution of Cancer : How the Therapy Approval Wave Sets... 2025 [https://www.linkedin.com/pulse/evolution-cancer-therapy-how-2025-approval-wave-sets-new-t65ie]
- 38. The future of evolutionary medicine: sparking innovation in biomedicine and public health - PubMed [https://pubmed.ncbi.nlm.nih.gov/37869257/]
- 39. Mapping 100 years of bacterial evolution reveals key spreaders of... [https://www.news-medical.net/news/20250925/Mapping-100-years-of-bacterial-evolution-reveals-key-spreaders-of-antibiotic-resistance.aspx]
- 40. Strategies Against Evolutionary ... Antimicrobial Resistance [https://spectrum.library.concordia.ca/id/eprint/995955/]
- 41. Multi-scale Predictions of Drug Resistance Epidemiology Identify Design Principles for Rational Drug Design - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8000225/]
- 42. De novo drug design using multiobjective evolutionary graphs - PubMed [https://pubmed.ncbi.nlm.nih.gov/19434831/]
- 43. Multi-objective de novo drug design using evolutionary graphs - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4235242/]
- 44. on the time trends of Comparative at... study antimicrobial resistance [https://pubmed.ncbi.nlm.nih.gov/40529905/]
- 45. Current Applications and the Future of Phage Therapy for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12189447/]
- 46. Phage therapy as a revitalized weapon for treating clinical ... [https://www.oaepublish.com/articles/mrr.2025.31]
- 47. Personalized inhaled bacteriophage therapy for treatment ... [https://www.nature.com/articles/s41591-025-03678-8]
- 48. Reassessment of Historical Clinical Trials Supports the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9769689/]
- 49. Introductory Chapter: Pharmacogenomics and Pharmacogenetics in... [https://www.intechopen.com/chapters/89050]
- 50. interventions to improve outcomes in patients with... Pharmacogenetic [https://pmc.ncbi.nlm.nih.gov/articles/PMC8975737/]
- 51. Frontiers | Bioinformatic challenges for pharmacogenomic study: tools for genomic data analysis [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1548991/full]
- 52. Five Key Advances Powering Precision in Pharmacogenomics [https://www.technologynetworks.com/drug-discovery/lists/five-key-advances-shaping-pharmacogenomics-405156]
- 53. Translating pharmacogenomics into clinical decisions: do not let the... [https://humgenomics.biomedcentral.com/articles/10.1186/s40246-019-0229-z]
- 54. Editorial: Insights in pharmacogenetics and pharmacogenomics: 2023 - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11739166/]
- 55. The future of evolutionary : sparking innovation in... medicine [https://pmc.ncbi.nlm.nih.gov/articles/PMC10590274/]
- 56. How evolutionary improve the understanding of human... principles [https://pmc.ncbi.nlm.nih.gov/articles/PMC3352556/]
- 57. A Proof-of-Concept Clinical Design for Trial ... | medRxiv Evolutionary [https://www.medrxiv.org/content/10.1101/2025.05.23.25328210v1]
- 58. Chronic inflammation: evolution in the gut [https://www.mpg.de/23761186/1125-limn-chronic-inflammatory-bowel-diseases-does-evolutionary-medicine-offer-new-therapeutic-approaches-153345-x]
- 59. and Experimental of microbial... design quantitative analysis [https://genomebiology.biomedcentral.com/articles/10.1186/s13059-017-1359-z]
- 60. Innovative animal for surgical interventions and implant... models [https://pmc.ncbi.nlm.nih.gov/articles/PMC12577895/]
- 61. Appropriateness of Animal for Studying Models Disease Human [https://www.news-medical.net/life-sciences/How-Appropriate-are-Animal-Models-for-Studying-Human-Disease.aspx]
- 62. Frontiers | Editorial: Advancements in translational : bridging... models [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1730195/full]
- 63. Biomimetic Chromatography to Accelerate Drug Discovery: Part 1 [https://www.chromatographyonline.com/view/biomimetic-chromatography-accelerate-drug-discovery-part-1]
- 64. The Race to Translate Sounds Into Animal Language | WIRED Human [https://www.wired.com/story/artificial-intelligence-translation-animal-sounds-human-language/]
- 65. Attitudes toward and perceptions of barriers to research among medical students in the context of an educational and motivational strategy - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12042497/]
- 66. The next generation of physician-researchers: undergraduate medical students’ and residents’ attitudes, challenges, and approaches towards addressing them - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11566606/]
- 67. Journal of Medical Internet Research - Data-Driven Infectious Disease... [https://www.jmir.org/2025/1/e81036]
- 68. Data-Driven Infectious Disease Control: Qualitative Study of... [https://pubmed.ncbi.nlm.nih.gov/41248479/]
- 69. Frontiers | Key enablers and barriers to ICU nurses’ professional ... [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1695617/full]
- 70. to developing new Barriers devices | medical Medical research [https://www.theguardian.com/science/2025/mar/17/barriers-to-developing-new-medical-devices]
- 71. The biggest barriers in drug development today | Drug Discovery News [https://www.drugdiscoverynews.com/the-biggest-barriers-in-drug-development-today-16341]
- 72. Panel Discussion: Overcoming barriers in drug discovery and development - Express Pharma [https://www.expresspharma.in/amp/panel-discussion-overcoming-barriers-in-drug-discovery-and-development/]
- 73. Learning decision thresholds for risk stratification models from aggregate clinician behavior - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8449610/]
- 74. risk models for COVID-19 patients using the... Predictive [https://pubmed.ncbi.nlm.nih.gov/39557887/]
- 75. risk models for COVID-19 patients using the... Predictive [https://www.nature.com/articles/s41598-024-77386-7?error=cookies_not_supported&code=393f83ec-320a-4ec2-927f-c1ce6681ee7f]
- 76. EMPOWER: Evolutionary Prompt Optimization With... Medical [https://arxiv.org/html/2508.17703v1]
- 77. Frontiers | The Evolution in Pharmacology of Infectious : Diseases 2025 [https://www.frontiersin.org/research-topics/70343/the-evolution-in-pharmacology-of-infectious-diseases-2025]
- 78. Stay Ahead of the Curve: Infectious Trends... Disease Clinical Trial [https://novotech-cro.com/whitepapers/stay-ahead-curve-infectious-disease-clinical-trial-trends-insights-2025]
- 79. Frontiers in Molecular Evolutionary - PMC Medicine [https://pmc.ncbi.nlm.nih.gov/articles/PMC7080150/]
- 80. Market Size Report Infectious Disease Clinical Trials 2025 [https://www.thebusinessresearchcompany.com/report/infectious-disease-clinical-trials-global-market-report]
- 81. Designing Effective Drug Therapies Using a Multiobjective Spider-Wasp Optimizer [https://www.mdpi.com/2313-7673/10/4/219]
- 82. The evolutionary rate of antibacterial drug | BMC Bioinformatics targets [https://bmcbioinformatics.biomedcentral.com/articles/10.1186/1471-2105-14-36]
- 83. In silico Methods for Identification of Potential Therapeutic Targets ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8616973/]
- 84. Expanding the MECP2 network using comparative reveals... genomics [https://elifesciences.org/articles/67085]
- 85. A comprehensive benchmark of tools for efficient genomic interval querying - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12306436/]
- 86. - Cross Analysis in Cultural and Human Behavior Evolution II Studies [https://www.academia.edu/49056883/Cross_Cultural_Analysis_in_Evolution_and_Human_Behavior_Studies_II]
- 87. Conducting cross - cultural , multi-lingual or multi-country scale... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11257704/]
- 88. A Better Way to Test for Sample Ratio Mismatches ... | Medium [https://medium.com/@michael.s.lindon/a-better-way-to-test-for-sample-ratio-mismatches-srms-and-validate-experiment-implementations-6da7c0d64552]
- 89. 13 Comparing quantitative data within individuals | Scientific Research and Methodology [https://bookdown.org/pkaldunn/SRM-Textbook/SummariseWithin.html]
- 90. 14 Comparing quantitative data between individuals | Scientific Research and Methodology [https://bookdown.org/pkaldunn/SRM-Textbook/BetweenQuantData.html]
- 91. New perspectives on evolutionary medicine: the relevance of... [https://bmcmedicine.biomedcentral.com/articles/10.1186/1741-7015-11-115]
- 92. What is Microevolution? Definition, Examples, Causes and Differences [https://www.vedantu.com/neet/microevolution]
- 93. Gene–environment interactions and their impact on human health | Genes & Immunity [https://www.nature.com/articles/s41435-022-00192-6]
- 94. Gene-environment interaction: definitions and study designs - PubMed [https://pubmed.ncbi.nlm.nih.gov/8936580/]
- 95. vs Systematic : Key Differences (2025) Review Meta Analysis [https://paperguide.ai/blog/systematic-review-vs-meta-analysis/]
- 96. What Is the Difference Between a Systematic ... | SpringerLink Review [https://link.springer.com/chapter/10.1007/978-3-662-58254-1_37]
- 97. The Differences Between a Systematic vs Review Meta Analysis [https://www.distillersr.com/resources/systematic-literature-reviews/understanding-the-differences-between-a-systematic-review-vs-meta-analysis]
- 98. vs. Systematic - Review : Key Differences — Otio Blog Meta Analysis [https://otio.ai/blog/systematic-review-vs-meta-analysis]
- 99. Colloquium Paper: Evolutionary perspectives on health and medicine - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2868294/]
- 100. A systematic - review of diagnostic and ... meta analysis performance [https://pmc.ncbi.nlm.nih.gov/articles/PMC11929846/]