Pathogenic Missense Variant Classification: From VUS to Clinical Action with AI and Structural Biology
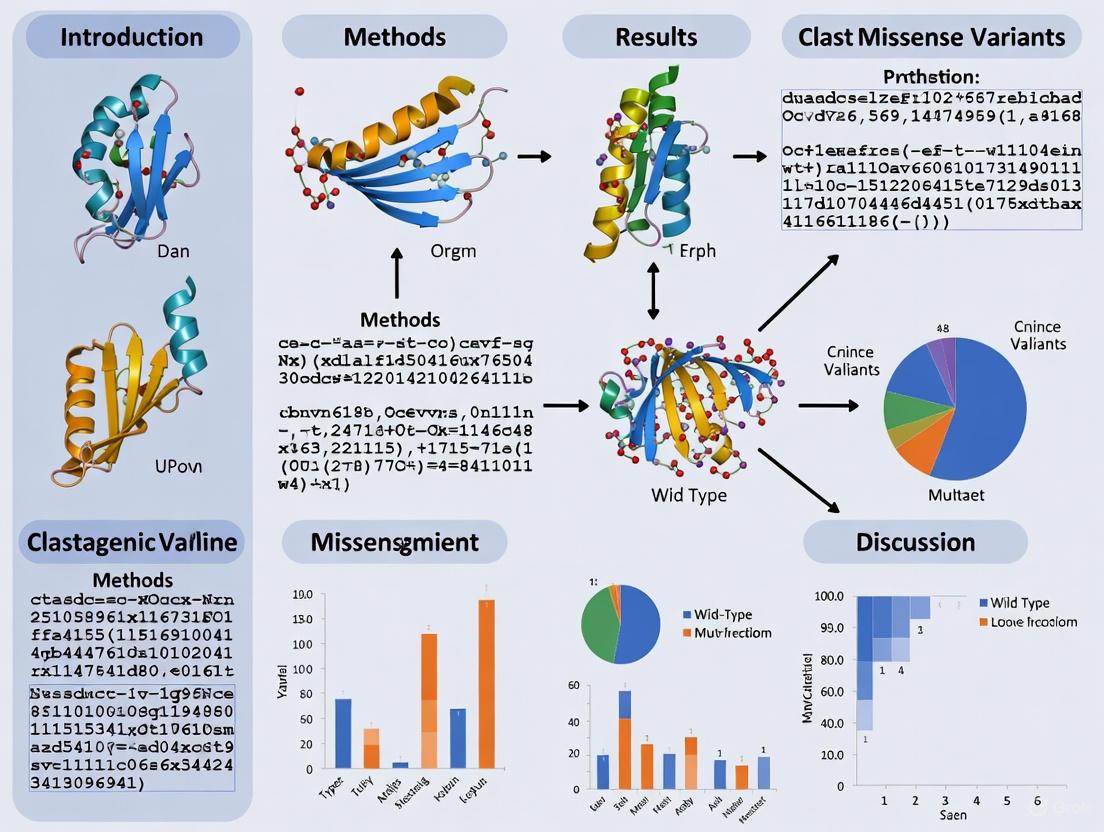
Accurate classification of missense variant pathogenicity is a critical challenge in clinical genetics and precision medicine, with over 98% of known variants still classified as Variants of Uncertain Significance (VUS).
Pathogenic Missense Variant Classification: From VUS to Clinical Action with AI and Structural Biology
Abstract
Accurate classification of missense variant pathogenicity is a critical challenge in clinical genetics and precision medicine, with over 98% of known variants still classified as Variants of Uncertain Significance (VUS). This article synthesizes the latest computational and experimental strategies to address this bottleneck, exploring foundational molecular principles of pathogenicity, advanced machine learning methodologies integrating structural biology and knowledge graphs, optimization techniques for complex cases, and rigorous validation frameworks. For researchers and drug development professionals, we provide a comprehensive roadmap covering disease-specific prediction models, AlphaFold2-enabled structural feature extraction, paralog-based evidence transfer, and emerging approaches for elucidating mode-of-action beyond binary classification to inform therapeutic development and clinical decision-making.
The Molecular Landscape of Missense Variants: From Protein Structure to Clinical Phenotype
In clinical genetics, a Variant of Uncertain Significance (VUS) represents a genetic change whose impact on health and disease risk is unknown. The classification and management of VUS constitute one of the most significant challenges in modern genomic medicine, creating what this article terms the "interpretation gap"—the disconnect between our ability to detect genetic variants and our capacity to understand their clinical relevance. This gap has profound implications for patient care, research consistency, and therapeutic development.
Recent large-scale studies have quantified the staggering scope of this problem. An analysis of over 1.6 million individuals undergoing hereditary disease genetic testing found that 41% of participants had at least one VUS [1]. The burden of VUS is not equally distributed; it varies dramatically by testing indication and population background. Research reveals that the number of reported VUS relative to pathogenic variants can vary by over 14-fold depending on the primary indication for testing and 3-fold depending on self-reported race [2] [3]. Furthermore, VUS reclassification rates highlight the dynamic nature of this field, with one study finding that at least 1.6% of variant classifications used in electronic health records for clinical care are outdated based on current ClinVar classifications [2].
Quantifying the VUS Burden: Key Statistics
Prevalence and Distribution
Table 1: VUS Prevalence Across Different Studies and Populations
| Study Population | Sample Size | Key Finding on VUS Prevalence | Data Source |
|---|---|---|---|
| Multi-gene panel testing | 1.6 million individuals | 41% had at least one VUS | Invitae study [1] |
| Adult genetics practices | 5,158 patients | VUS rate varied 14-fold by testing indication, 3-fold by race | Brotman Baty Institute Database [2] |
| ClinVar database | 206,594 missense variants | 57.5% (118,864) classified as VUS | Nature Communications [4] |
| Variant reclassification | 26 specific instances | Reclassifications never communicated to patients | Folta et al. [2] |
Table 2: Factors Contributing to VUS Interpretation Discordance
| Factor | Impact on VUS Interpretation | Evidence |
|---|---|---|
| Testing laboratory differences | 43% rate of classification difference for same variant between labs | Interview data with geneticists [5] |
| Clinician expertise | Genetics experts routinely reassess lab interpretations; non-experts report high trust without reassessment | Clinician interviews [5] |
| Population ancestry | Ashkenazi Jewish/White individuals: lowest VUS rates; Pacific Islander/Asian individuals: highest VUS rates | Invitae study [1] |
| Panel size | VUS rate increases with number of genes tested | Analysis of multi-gene panels [1] |
Methodological Frameworks for VUS Interpretation
Standardized Variant Classification Guidelines
The American College of Medical Genetics and Genomics (ACMG) and the Association for Molecular Pathology (AMP) have established guidelines for variant classification that form the current gold standard. These guidelines categorize variants into five distinct classes:
- Pathogenic and Likely Pathogenic: Variants with sufficient evidence supporting disease causation
- Benign and Likely Benign: Variants with sufficient evidence supporting no clinical significance
- Variant of Uncertain Significance (VUS): Variants with insufficient evidence for either pathogenic or benign classification [6]
The ACMG/AMP framework recommends that laboratories report only pathogenic and likely pathogenic variants in most clinical contexts, though VUS may be reported in specific circumstances where the information may still have clinical utility [6].
Advanced Computational Methods for Missense Variant Interpretation
Experimental Protocol: ESM1b Protein Language Model for Pathogenicity Prediction
Recent research has demonstrated that protein language models can significantly enhance missense variant interpretation:
- Data Collection: Gather missense variant information from population databases (gnomAD) and clinical databases (ClinVar) [4]
- Feature Extraction: Utilize the ESM1b model to generate numerical scores for all possible amino acid changes
- Variant Scoring: Apply the ESM1b scoring system where scores less than -7.5 indicate likely pathogenic missense variants [4]
- Phenotype Correlation: Correlate ESM1b scores with clinical phenotypes across multiple genes
- Validation: Assess prediction accuracy against known variant classifications and clinical outcomes
This methodology has shown remarkable predictive power, with ESM1b scores significantly predicting mean phenotype of missense variant carriers in six of ten cardiometabolic genes studied (binomial enrichment p = 2.76E-06) [4]. The model can also distinguish between loss-of-function and gain-of-function variants, providing crucial functional insights beyond simple pathogenicity classification.
Integrated Workflow for VUS Assessment and Reclassification
Experimental Protocol: Comprehensive VUS Reclassification System
Data Integration
- Extract variant information from electronic health records (EHR)
- Cross-reference with public databases (ClinVar, OMIM, GeneReviews)
- Incorporate population frequency data (gnomAD, 1000 Genomes)
Evidence Aggregation
- Collect clinical patient data and phenotype information
- Perform segregation analysis within families
- Incorporate functional study results from literature
- Utilize computational predictions from multiple algorithms
Multidisciplinary Review
- Convene variant review committees with clinical and laboratory geneticists
- Assess evidence strength using ACMG/AMP criteria
- Make classification decisions based on aggregated evidence
Reclassification Communication
This systematic approach has demonstrated real-world impact, with one study identifying 26 instances where testing laboratories updated ClinVar with variant reclassifications, but this critical information was never communicated to the affected patients [2].
Table 3: Research Reagent Solutions for VUS Interpretation
| Resource Category | Specific Tools/Databases | Primary Function | Key Features |
|---|---|---|---|
| Variant Databases | ClinVar, ClinGen, Franklin Genoox | Aggregate variant classifications and evidence | Centralized repository of clinical interpretations with multiple submitter data [7] |
| Population Databases | gnomAD, 1000 Genomes, dbSNP | Provide allele frequency across populations | Filtering of common polymorphisms; identification of rare variants [8] |
| Computational Prediction Tools | ESM1b, AlphaMissense, PolyPhen-2, SIFT | Predict functional impact of missense variants | Integration of evolutionary conservation and structural features [8] [4] |
| Clinical Resources | GeneReviews, OMIM | Curated gene-disease relationships and clinical management | Expert-reviewed clinical summaries and practice guidelines [7] |
| Protein Structure Tools | AlphaFold2, PDBe, PDB | Provide protein structural context | Assessment of variant impact on protein folding and function [8] |
| Visualization Platforms | IGV, UCSC Genome Browser | Genomic context visualization | Integration of multiple data types for variant interpretation |
Troubleshooting Common VUS Interpretation Challenges
FAQ 1: How should we handle discrepant variant classifications between different testing laboratories?
Issue: Variant classifications for the same variant differ between laboratories, creating clinical confusion.
Solution:
- Review the specific evidence cited by each laboratory for their classification
- Consult independent databases such as ClinVar to assess consensus classification
- Evaluate whether clinical features in your patient support one classification over another
- Consider orthogonal testing methods or referral to specialized centers for complex cases
- Document the rationale for ultimately following a particular classification [5]
Genetic counselors report that disagreements with laboratory variant classifications, while uncommon, most frequently stem from conflicting laboratory interpretations or discrepancies in clinical correlation [7].
FAQ 2: What is the most effective approach for VUS reclassification?
Issue: VUS reclassification rates are substantial, but systematic approaches are lacking.
Solution:
- Implement proactive monitoring systems for previously identified VUS
- Establish clear institutional protocols for reassessment timelines and triggers
- Prioritize VUS in genes with strong disease association and available functional data
- Utilize computational methods like ESM1b scores that show strong correlation with phenotype severity [4]
- Develop standardized patient re-contact procedures for clinically significant reclassifications
Research indicates that clinical evidence, including detailed patient information and family studies, contributes most significantly to VUS reclassifications [1].
FAQ 3: How can we address disparities in VUS rates across different ancestral populations?
Issue: Individuals from non-European ancestries experience higher VUS rates, exacerbating health disparities.
Solution:
- Prioritize inclusion of diverse populations in genomic research databases
- Utilize population-specific allele frequency databases when available
- Advocate for funding and research focused on variant interpretation in underrepresented groups
- Implement careful pre-test counseling about VUS likelihood based on patient ancestry
- Support efforts to develop ancestry-informed computational prediction models [1]
Studies demonstrate that Ashkenazi Jewish and White individuals have the lowest observed VUS rates, while Pacific Islander and Asian individuals have the highest, highlighting the critical need for more diverse genomic data [1].
FAQ 4: What clinical guidance should be provided for VUS findings?
Issue: Uncertainty about appropriate clinical management when a VUS is identified.
Solution:
- Base clinical management on personal and family history, not VUS findings alone
- Document clear rationale against basing clinical decisions on VUS status
- Provide ongoing counseling about the possibility of future reclassification
- Establish systems to track VUS and facilitate reassessment over time
- Encourage patients to update contact information to enable future re-contact [7]
Genetic counselors report that most do notify patients of reclassification from VUS to pathogenic or benign categories, though communication methods vary, indicating a need for standardized protocols [7].
Future Directions: Closing the Interpretation Gap
The field of VUS interpretation is rapidly evolving with several promising approaches to reduce the interpretation gap. Machine learning methods are showing substantial progress, with one commercial laboratory reporting that their AI-driven approaches have already helped reduce uncertain results for over 300,000 individuals [1]. Integration of polygenic risk scores with monogenic variant analysis represents another promising avenue, as research demonstrates that polygenic background significantly modifies phenotype among pathogenic variant carriers [4]. Advanced sequencing technologies including long-read sequencing and single-cell approaches are improving variant detection in technically challenging regions, potentially resolving previously unclassifiable variants [9].
The systematic implementation of evidence-based frameworks for variant interpretation and reclassification, coupled with standardized protocols for communicating updated information to patients and providers, will be essential for addressing the current VUS challenge. As these approaches mature, the field moves closer to realizing the full potential of precision medicine by ensuring that genetic findings translate to clear clinical guidance rather than uncertainty.
Interpreting the clinical significance of genetic variants is a cornerstone of modern genomic medicine. For missense variants, this task is particularly challenging as their effect on protein function is not always obvious. The three-dimensional structure of a protein provides a critical physical framework for understanding how and why certain amino acid changes lead to disease. Proteins perform their functions through precise arrangements of domains, surfaces, and interaction interfaces, and pathogenic missense variants are not randomly distributed across these structural elements. Research has consistently demonstrated that these variants cluster in structurally and functionally important regions, including protein-protein interaction interfaces, catalytic sites, and structurally constrained cores [10] [11]. This technical support document provides researchers and drug development professionals with practical guidance for leveraging structural biology in variant interpretation, framed within the context of investigating these enrichment patterns.
Core Concepts: Structural Enrichment of Pathogenic Variants
Quantitative Enrichment Patterns
Large-scale studies analyzing atomic-resolution interactomes have revealed distinct statistical patterns in the distribution of pathogenic variants. The following table summarizes key quantitative findings on the enrichment of pathogenic variants in different structural regions.
Table 1: Enrichment of Pathogenic Missense Variants Across Protein Structural Regions
| Structural Region | Enrichment Observation | Statistical Significance & Notes |
|---|---|---|
| Protein-Protein Interaction Interface | Significant enrichment of in-frame pathogenic variations [10] | Considered "hot-spots"; alterations are significantly more disruptive than evolutionary changes [10] |
| Entire Interacting Domain | Enrichment of pathogenic variations, not limited to interface residues [10] | Suggests the entire domain's structural integrity is crucial for proper interaction [10] |
| Buried Residues (Low Solvent Accessibility) | Pathogenic variants strongly associated with low Relative Solvent Accessibility (RSA) [12] | p = 2.89e-2,276; proteins are less tolerant of buried mutations [12] |
| Regular Secondary Structures (Alpha helices, Beta-sheets) | Tendency for mutations to be pathogenic [12] | Odds Ratio (OR) for alpha helices: 1.73; OR for beta-sheets: 1.97 [12] |
| Disulfide Bonds | Very high likelihood of pathogenicity if disrupted [12] | Odds Ratio (OR) = 93.8; 98.72% of disruptive variants were pathogenic [12] |
| Loops/Irregular Stretches | Tendency for mutations to be benign [12] | Odds Ratio (OR) = 0.32 [12] |
Key Structural Principles of Pathogenicity
The quantitative data above supports several core principles:
- Interface Disruption: Variations at interaction "hot-spots" can directly disrupt the biophysical strength of protein-protein interactions [10].
- Structural Destabilization: Pathogenic variations often introduce substantial changes in protein stability (measured as ΔΔG), more so than benign variants [12]. This can lead to misfolding, aggregation, or degradation.
- Domain-Wide Integrity: The enrichment of pathogenic variants across entire interacting domains, not just the direct contact residues, underscores that the overall structural fold and stability of a domain are essential for its function [10].
Frequently Asked Questions (FAQs)
FAQ 1: Our lab has identified a VUS in a gene of interest. The variant is buried in the protein core with low RSA. How should we prioritize it for further analysis?
A variant with low RSA is a higher priority for functional analysis. Buried residues are critical for maintaining the protein's stable core. Mutations in these regions often destabilize the protein's native fold, leading to loss of function. You should:
- Calculate the predicted change in stability (ΔΔG) using tools like FoldX.
- Check if the residue is highly conserved.
- A significantly destabilizing ΔΔG (e.g., < -2 kcal/mol) and high conservation strongly suggests pathogenicity [13] [12]. Proceed with functional assays to test for protein expression, stability, and localization.
FAQ 2: A variant is located in a loop region, which is often considered more tolerant of mutation. However, our structural model shows it is near the active site. How do we resolve this?
Loop regions can be functionally important despite their general tolerance. Proximity to an active site is a major red flag. You must investigate:
- Direct Involvement: Does the loop form part of the active site cavity?
- Allosteric Role: Could a mutation in this loop affect the dynamics or precise positioning of active site residues? Use Structure-Based Network Analysis (SBNA) to quantify the residue's topological importance within the 3D network; a high network score would indicate critical structural importance despite being in a loop [11].
FAQ 3: We are studying a variant that disrupts a salt bridge not at a known interaction interface. What is the potential mechanism of pathogenicity?
The disruption of a stabilizing salt bridge is a classic mechanism for pathogenic loss-of-function. Even if not at an interface, this can:
- Reduce Global Stability: Lower the protein's melting temperature and increase its propensity to unfold or aggregate.
- Alter Local Conformation: Impair the precise geometry of a functional pocket or allosteric site.
- Affect Dynamics: Hinder necessary conformational changes required for function. Evaluate the ΔΔG and correlate with clinical data. In vitro thermal shift assays are an excellent method for experimental validation [13].
FAQ 4: When using predicted structures from AlphaFold2, how reliable are they for calculating stability metrics (ΔΔG) and identifying interface residues?
AlphaFold2 has expanded structural coverage of the human proteome dramatically. Studies show that for regions with high per-residue confidence scores (pLDDT > 80), AlphaFold2 structures can be used to compute stability metrics with accuracy similar to experimentally determined structures [13] [12]. However, high-quality experimental structures (e.g., from X-ray crystallography) should still be preferred when available, as they can outperform AlphaFold2 in stability calculations [13]. For interface prediction, the newer AlphaFold3 promises better modeling of complexes, but this has yet to be fully validated for variant interpretation [13].
Troubleshooting Guides
Guide: Validating a Putative Protein-Protein Interaction Disruptor
Problem: A VUS is predicted to lie at a protein-protein interaction interface, but you need experimental validation that it disrupts the interaction.
Solution: A Yeast Two-Hybrid (Y2H) assay is a well-established method for this purpose.
Workflow Overview: The diagram below illustrates the logical workflow for this experimental validation.
Detailed Protocol:
- Generate Variants: Using the wild-type cDNA clone (e.g., from the human ORFeome collection), generate the specific VUS allele via site-directed mutagenesis. Use a kit such as the Stratagene QuikChange Kit and mutagenic primers designed according to the manufacturer's protocol. Perform mutagenesis PCR with a high-fidelity polymerase like Phusion [10].
- Clone into Y2H Vectors: Clone both the wild-type and VUS sequences into appropriate Y2H vectors (e.g., pGBKT7 as bait and pGADT7 as prey).
- Co-transform Yeast: Co-transform the bait and prey plasmids into a suitable yeast strain (e.g., AH109 or Y2HGold).
- Select for Diploids: Plate the transformed yeast on synthetic dropout (SD) media lacking Leucine and Tryptophan (SD/-Leu/-Trp) to select for cells containing both plasmids. Incubate at 30°C for 3-5 days.
- Assay for Interaction: Restreak positive colonies onto more stringent selective media, typically SD media lacking Adenine and Histidine (SD/-Ade/-His) and supplemented with X-α-Gal. A successful protein-protein interaction will activate reporter genes, allowing growth and turning colonies blue.
- Interpret Results: Compare the growth and color of yeast containing the VUS pair against the wild-type positive control and empty vector negative controls. Lack of growth/blue color suggests the VUS disrupts the interaction.
Guide: Choosing the Right Protein Structure for Analysis
Problem: Inconsistent results from in silico tools due to the use of different protein structures or models.
Solution: Follow a structured hierarchy for selecting the most reliable protein structure.
Workflow Overview: The diagram below outlines the decision-making process for structure selection.
Troubleshooting Steps:
- Check the PDB: Always first search the Protein Data Bank (PDB) for an experimentally determined structure.
- Prioritize by Method: Prefer high-resolution X-ray crystallography or high-quality Cryo-EM structures. NMR structures, while informative for dynamics, are less suitable for computing stability metrics due to their conformational ensembles [13].
- Evaluate Quality: If multiple structures exist, choose the one with the highest resolution and completeness for your region of interest.
- Use Predictions if Necessary: If no experimental structure exists, use a predicted structure from AlphaFold2 (via the AlphaFold Protein Structure Database). Focus your analysis on regions with high per-residue confidence (pLDDT > 80) [12].
- Consider Homology Modeling: As an alternative, check repositories like SWISS-MODEL for homology models, but native or ab initio predicted structures are generally preferred [13].
The Scientist's Toolkit: Essential Research Reagents & Computational Tools
This table lists key materials and tools required for experiments investigating the structural basis of variant pathogenicity.
Table 2: Research Reagent Solutions for Structural Pathogenicity Analysis
| Category / Item Name | Specific Example / Vendor | Function & Application in Research |
|---|---|---|
| Cloning & Mutagenesis | ||
| Human ORFeome Collection | e.g., Human ORFeome v8.1 [10] | Source of wild-type, sequence-verified cDNA clones for a wide array of human genes. |
| Site-Directed Mutagenesis Kit | e.g., Stratagene QuikChange Kit [10] | Introduces specific nucleotide changes into plasmid DNA to create VUS and control constructs. |
| High-Fidelity DNA Polymerase | e.g., Phusion Polymerase (NEB) [10] | Used for accurate amplification during mutagenesis PCR to avoid introducing secondary mutations. |
| Interaction Validation | ||
| Yeast Two-Hybrid System | e.g., MATCHMAKER Gal4 System (Clontech) | In vivo method to test for protein-protein interaction disruption by a variant [10]. |
| Y2H Yeast Strain | e.g., AH109, Y2HGold | Genetically engineered yeast strains with multiple auxotrophic markers for selection. |
| Structural Analysis Software | ||
| Molecular Visualization | UCSF Chimera, PyMOL | Visualizes 3D structures, maps variants, and analyzes residue burial and contacts. |
| Stability Prediction | FoldX [13] [12] | Industry-standard tool for predicting the change in protein stability (ΔΔG) upon mutation. |
| Structure-Based Network Analysis | Custom SBNA scripts [11] | Quantifies topological importance of a residue within the 3D protein structure network. |
| Solvent Accessibility | Naccess [10] | Calculates Relative Solvent Accessibility (RSA) from PDB files. |
| Structural Databases | ||
| Experimental Structures | Protein Data Bank (PDB) [10] [13] | Primary repository for experimentally determined 3D structures of proteins. |
| Predicted Structures | AlphaFold Protein Structure Database [12] | Database of AlphaFold2 predictions for a large portion of the human proteome. |
| Domain Interactions | 3did, iPfam [10] | Curated databases of protein domain-domain interactions. |
Evolutionary Conservation and Paralogous Genes as Evidence for Pathogenicity
Frequently Asked Questions (FAQs) and Troubleshooting
Q1: What is a paralogous variant and how can it serve as evidence for pathogenicity?
A paralogous variant is a missense variant located in a paralogous gene at the analogous residue position, as defined by a multiple sequence alignment across a gene family, and it shares the same reference amino acid as the target gene [14].
The presence of a pre-classified pathogenic variant at this conserved position in a paralogous gene provides quantifiable evidence for the pathogenicity of a novel variant in your gene of interest. Systematic analyses show that this evidence, termed the para-SAME criterion, is associated with a positive likelihood ratio (LR+) of 13.0 for variant pathogenicity. Even a pathogenic variant with a different amino acid change at the same position (the para-DIFF criterion) has an LR+ of 6.0 [14].
Q2: Why is my variant still a VUS even though a pathogenic variant exists in a paralog?
This typically occurs for one of the following reasons:
- Insufficient Sequence Similarity: The paralogous gene used for comparison may not share a high enough degree of sequence similarity (>90% in key domains) to confidently transfer pathogenic evidence. Always verify the quality of the multiple sequence alignment.
- Lack of Gene-Family Specific Calibration: The strength of evidence from paralogous variants can differ significantly across gene families [14]. General guidelines may not be calibrated for your specific gene family.
- Conflicting Evidence: Other lines of evidence, such as population frequency or computational predictions, may conflict with the paralog-based evidence, preventing an upgrade from VUS to Likely Pathogenic.
Q3: How many pathogenic paralogous variants are needed for strong evidence?
While a single pathogenic variant in a paralog provides moderate evidence, the strength of evidence increases with the number of independent pathogenic variants found at the same conserved residue across multiple paralogs within the gene family [14]. The fold enrichment of pathogenic variants progressively rises with a higher number of supporting paralogous variants.
Q4: How do I handle phenotypes when using paralogous evidence?
Phenotype patterns can be conserved across paralogs. For example, in voltage-gated sodium channels, loss-of-function related disorders in genes like SCN1A, SCN2A, SCN5A, and SCN8A show overlapping spatial variant clusters in 3D protein structures [14]. When selecting paralogous variants as evidence, consider if the associated disorders in the paralog share a similar molecular disease mechanism with the disorder linked to your target gene. Integrating phenotype data can improve variant classification.
Q5: What are the best tools for identifying and analyzing paralogous genes and variants?
The table below summarizes essential tools for this workflow.
Table 1: Key Bioinformatics Tools for Paralog and Variant Analysis
| Tool Name | Primary Function | Key Application in This Context | Source/Link |
|---|---|---|---|
| BLAST | Sequence similarity search | Identifying paralogous genes via sequence comparison [15] [16]. | NCBI |
| Clustal Omega / MAFFT | Multiple Sequence Alignment (MSA) | Creating alignments to find conserved residue positions across paralogs [15]. | EMBL-EBI |
| HAMAP-Scan | Protein family classification | Scanning sequences against curated protein families [17]. | Expasy |
| OrthoDB | Cataloging orthologs & paralogs | Providing evolutionary and functional annotations for paralogs [17]. | OrthoDB |
| AlphaMissense | Pathogenicity prediction | Computational evidence for missense variant pathogenicity [18]. | Google Research |
| gnomAD | Population variant frequency | Assessing variant frequency to find benign controls [14] [19]. | gnomAD |
| UCSC Genome Browser | Genome visualization | Visualizing variant conservation across paralogous regions [19]. | UCSC |
| SAMtools | Handling sequence data | Processing and manipulating alignment files (BAM/VCF) [16]. | SAMtools |
Quantitative Data on Paralogous Variant Evidence
The following table summarizes the key quantitative findings from a large-scale exome study on using paralogous variants as evidence for pathogenicity [14].
Table 2: Quantitative Impact of Integrating Paralogous Variant Evidence
| Metric | Gene-Specific Evidence Only | With Paralogous Evidence | Fold Change |
|---|---|---|---|
| Classifiable Amino Acid Residues | 22,071 residues | 83,741 residues | 3.8-fold increase |
| Positive Likelihood Ratio (LR+) | |||
| • para-SAME (same AA change) | N/A | 13.0 (95% CI: 12.5-13.7) | N/A |
| • para-DIFF (different AA change) | N/A | 6.0 (95% CI: 5.7-6.2) | N/A |
Experimental Protocols
Protocol 1: Identifying Pathogenic Variants in Paralogous Genes
This protocol outlines the steps to systematically gather evidence from paralogs for a missense VUS.
1. Define the Gene Family: * Input: Your gene of interest (e.g., PRPS1). * Method: Use databases like HGNC, OrthoDB, or PANTHER to identify all members of the gene family [20] [17]. * Output: A list of paralogous genes (e.g., for PRPS1, this includes PRPS2, PRPS3, PRPSAP1, PRPSAP2).
2. Perform Multiple Sequence Alignment (MSA): * Input: Protein sequences for all paralogs. * Method: Use a tool like Clustal Omega or MAFFT to generate a high-quality MSA [15]. * Troubleshooting: If alignment quality is poor in key domains, consider aligning specific protein domains identified via Pfam or PROSITE [19] [17]. * Output: A residue-to-residue alignment mapping your VUS position to the equivalent positions in all paralogs.
3. Mine Variant Databases: * Input: The equivalent amino acid positions in all paralogs. * Method: Query clinical databases (ClinVar, HGMD) and population databases (gnomAD, ExAC) for all variants at these aligned positions [14] [19]. * Output: A list of pre-classified variants (Pathogenic, Likely Pathogenic, Benign, etc.) at the conserved residue across the gene family.
4. Apply Classification Criteria: * Input: The list of variants from Step 3. * Method: * If a Pathogenic or Likely Pathogenic variant with the identical amino acid change is found, apply the para-SAME criterion. * If a Pathogenic or Likely Pathogenic variant with a different amino acid change is found, apply the para-DIFF criterion. * Output: Supporting evidence for pathogenicity (at the supporting, moderate, or strong level, depending on gene-family specific calibration) for your VUS.
Protocol 2: Calibrating Paralogous Evidence for a Specific Gene Family
To use paralogous evidence quantitatively, gene-family specific calibration is recommended [14].
1. Curate a Gold-Standard Variant Set: * Compile known pathogenic variants (from ClinVar/HGMD) and benign population variants (from gnomAD) for all genes in the family.
2. Map Variants to MSA: * Map all variants to the multiple sequence alignment to identify residues with variants in multiple paralogs.
3. Calculate Likelihood Ratios (LR):
* For a given residue, calculate the LR as follows:
LR = (Probability residue is in a pathogenic variant | Pathogenic) / (Probability residue is in a pathogenic variant | Benign)
* This calculates how much more likely it is to find a pathogenic variant at a residue that is "hit" by a pathogenic paralogous variant compared to a benign variant.
4. Establish Evidence Strength Thresholds: * Based on the calculated LRs, define thresholds for supporting, moderate, and strong levels of evidence for your gene family, similar to the ACMG/AMP guidelines for PS1 and PM5 criteria [21].
Identifying Pathogenic Variants in Paralogous Genes Workflow
Research Reagent Solutions
Table 3: Essential Reagents and Databases for Paralog-Based Pathogenicity Analysis
| Item Name | Type | Function/Application | Source |
|---|---|---|---|
| ClinVar | Database | Public archive of reports of human genetic variants and interpretations [14] [18]. | NIH/NCBI |
| HGMD (Human Gene Mutation Database) | Database (Commercial) | Comprehensive collection of published pathogenic mutations in human genes [14]. | Qiagen |
| gnomAD (Genome Aggregation Database) | Database | Population genome variant frequency database; used as a source of benign control variants [14] [19]. | Broad Institute |
| UniProtKB/Swiss-Prot | Database | Expertly curated protein sequence and functional information [17]. | SIB Swiss Institute |
| HGNC Gene Family Data | Database | Authoritative gene families as defined by the Human Gene Nomenclature Committee [14]. | HGNC |
| Multiple Sequence Alignment (MSA) | Computational Tool | Fundamental for identifying conserved residue positions across paralogs [14]. | Clustal Omega, MAFFT |
Evolutionary Relationship of Paralogous Genes
FAQs: Core Concepts and Molecular Features
FAQ 1: What are the key molecular and cellular features that differentiate pathogenic missense variants from benign ones?
Pathogenic and benign missense variants can be distinguished by their distinct molecular footprints across protein structure, functional pathways, and proteomic properties. The following table summarizes the key differentiating features identified through large-scale analyses.
Table 1: Key Molecular Features Differentiating Pathogenic and Benign Variants
| Feature Category | Pathogenic Variant Association | Benign (Population) Variant Association |
|---|---|---|
| Protein Structural Region | Enriched in protein cores and interaction interfaces [22] | Enriched on protein surfaces and in disordered regions [22] |
| Functional Pathways | Affect cell proliferation and nucleotide processing pathways [22] | Not strongly associated with specific pathways in this analysis [22] |
| Protein Abundance | Found in more abundant proteins [22] | No strong correlation with abundance [22] |
| Protein Stability | Often predicted to be destabilizing to protein structure [23] [24] | Often predicted to have neutral stability effects [23] |
| Downstream Proteomic Effect | Destabilizing pathogenic variants linked to lower protein levels in cancer samples [23] | Not associated with significant changes in protein levels [23] |
FAQ 2: How does the local 3D structural context of a variant influence its pathogenicity?
The location of a missense variant within a protein's three-dimensional structure is a major determinant of its functional impact. Pathogenic variants are significantly enriched in buried residues that form the protein core and at residues that form interfaces with other molecules. In contrast, population variants are more common on the solvent-accessible protein surface. This is because residues in the core are often critical for maintaining structural stability, while interface residues are essential for specific binding and signaling functions. Variants on the surface or in intrinsically disordered regions are more likely to be tolerated, as they less frequently disrupt the protein's fundamental architecture [22]. Furthermore, a study exploring mechanistic impacts found that disease-linked variants are enriched in predicted small-molecule binding pockets and at protein-protein interfaces [23].
FAQs: Experimental Approaches and Validation
FAQ 3: What high-throughput experimental methods can functionally profile thousands of missense variants at once?
Deep Mutational Scanning (DMS) is a powerful framework for exhaustively mapping the functional consequences of missense variants. The core workflow involves creating a vast library of variant genes, expressing them in a system where protein function influences a selectable outcome (like cell growth), and using high-throughput sequencing to quantify the effect of each variant.
Table 2: Key Deep Mutational Scanning (DMS) Methodologies
| Method Stage | Description | Key Techniques/Considerations |
|---|---|---|
| 1. Mutagenesis | Generation of a library containing all possible amino acid substitutions. | Random codon mutagenesis (e.g., POPCode) to ensure even coverage [25]. |
| 2. Library Generation | Cloning the variant library into an expression system. | Can be barcoded (DMS-BarSeq) for tracking individual variants or tiled (DMS-TileSeq) for direct variant sequencing [25]. |
| 3. Functional Selection | Applying a selection pressure linked to protein function. | Often uses functional complementation assays in yeast or other models to test if variants rescue a loss-of-function phenotype [25]. |
| 4. Readout & Analysis | Quantifying variant fitness from selection results. | High-throughput sequencing of barcodes or tiled amplicons before and after selection to calculate enrichment/depletion [25]. |
The diagram below illustrates the two primary DMS workflows.
FAQ 4: How can I validate the functional impact of a specific missense variant in a live animal model?
Caenorhabditis elegans (C. elegans) is a simple, cost-effective in vivo model for functional validation. The protocol involves:
- Ortholog Analysis: Identify the C. elegans ortholog of the human gene of interest. Approximately 250 human disease genes have clear orthologs in C. elegans, and about half of documented human variants in these genes are missense variants of uncertain significance [26].
- Strain Generation: Use CRISPR-Cas9 genome editing to introduce the specific human missense variant into the orthologous C. elegans gene.
- Phenotypic Analysis: Conduct assays to compare the phenotype of the variant-bearing worm to wild-type and known loss-of-function mutants. Phenotypes can include morphological defects, changes in lifespan or reproduction, and sensitivity to stress.
- Rescue Experiments: Test if the observed pathogenic phenotype can be rescued by supplementation with a relevant molecule, such as coenzyme Q10 for variants in the COQ2 ortholog, coq-2 [26].
This approach provides direct, quantitative phenotypic data on the functional consequences of a variant in a living organism.
FAQs: Computational Prediction and Troubleshooting
FAQ 5: A widely-used computational predictor (AlphaMissense) classified my variant as pathogenic, but my experimental data suggests it is benign. Why might this happen?
Discordance between computational predictions and experimental or clinical findings is a known challenge. A 2025 study highlighted specific limitations of deep learning models like AlphaMissense:
- Performance Gaps: When evaluated on a rare disease cohort, AlphaMissense showed a precision of only 32.9%, meaning many variants it flagged as likely pathogenic were not classified as such by expert curation in ClinVar [27].
- Intrinsic Disorder: AlphaMissense and other models struggle to accurately evaluate pathogenicity in intrinsically disordered regions (IDRs), which lack a fixed 3D structure, leading to unreliable predictions in these protein segments [27].
- Splice Effects: Some variants classified as missense may actually affect mRNA splicing. In one analysis, 5-7% of pathogenic missense variants not caught by predictors had potential splice-disrupting effects, which the missense-focused models would not account for [27].
Always correlate computational predictions with other lines of evidence, such as population frequency, evolutionary conservation, and functional assay data, before drawing conclusions.
FAQ 6: With over 97 variant effect predictors (VEPs) available, how do I choose one and avoid biased evaluations?
Choosing and evaluating VEPs requires careful consideration to avoid data circularity, which can make predictors seem more accurate than they are. The following table compares a selection of widely used predictors.
Table 3: Comparison of Selected Variant Effect Predictors (VEPs)
| Predictor Name | Underlying Approach | Score Range & Interpretation | Key Considerations |
|---|---|---|---|
| AlphaMissense | Deep learning (based on AlphaFold2), fine-tuned on population frequency [28] [27] | 0 to 1; <0.34 Benign, >0.56 Pathogenic [28] | Struggles with disordered regions; author thresholds may favor recall over precision [27]. |
| REVEL | Ensemble method combining 13 other tools [29] [28] | 0 to 1; Higher scores = more likely pathogenic [28] | An established meta-predictor that integrates multiple independent signals. |
| SIFT | Evolutionary conservation of amino acids [30] [28] | 0 to 1; <0.05 Deleterious [28] | One of the earliest and most widely used methods. |
| PolyPhen-2 | Physical/ comparative considerations of protein structure/function [30] [28] | 0 to 1; Higher scores = more likely deleterious [28] | Provides a probability of a variant being damaging. |
| CADD | Integrates diverse genomic annotations into one score [30] | Phred-scaled score; Higher scores = more likely deleterious | Not trained solely on human clinical variants, reducing some circularity [30]. |
To perform a robust benchmark of VEPs, use data from Deep Mutational Scanning (DMS) experiments. DMS data provides several advantages: it does not rely on pre-assigned clinical labels (reducing variant-level circularity), and performance can be compared on a per-protein basis (reducing gene-level circularity) [31]. Studies show a strong correspondence between a VEP's performance on DMS benchmarks and its ability to classify clinical variants correctly, especially for predictors not directly trained on human variant data [31].
FAQ 7: How can I visualize the decision-making process of a machine learning model for variant classification?
The LEAP (Learning from Evidence to Assess Pathogenicity) model provides a framework for explainable machine learning in variant classification. It ranks evidence features by their contribution to the final prediction. The diagram below illustrates a simplified, generalizable workflow for how such a model might integrate different evidence categories to classify a variant.
The Scientist's Toolkit: Research Reagent Solutions
Table 4: Essential Research Reagents and Resources for Variant Analysis
| Reagent / Resource | Type | Function and Application |
|---|---|---|
| gnomAD Database | Population Database | Provides allele frequencies from a large population, serving as a key resource for assessing variant rarity and prioritizing benign variants [22] [29]. |
| ClinVar Database | Clinical Database | A public archive of reports on the relationships between human variants and phenotypes, with supporting evidence [22] [27]. |
| COSMIC Database | Disease Database | Catalogs somatic mutations in human cancer, useful for identifying driver mutations in oncology research [22]. |
| AlphaFold2 DB | Structural Database | Provides high-accuracy predicted protein structures for the human proteome, enabling structural analysis of variants when experimental structures are unavailable [23]. |
| ZoomVar Database | Integrated Resource | A database that allows programmatic annotation of missense variants with protein structural information and calculation of variant enrichment in different protein regions [22]. |
| CRISPR-Cas9 | Molecular Tool | Enables precise genome editing to introduce specific missense variants into model organisms (e.g., C. elegans) for functional validation [26]. |
| Yeast Complementation Assay | Functional Assay | A classical genetics technique adapted for high-throughput DMS to test the functional impact of human gene variants by rescuing a deficient yeast strain [25]. |
Advanced Computational Frameworks: AI, Knowledge Graphs, and Structural Biology
Graph Neural Networks for Disease-Specific Variant Interpretation
FAQs: Model Selection and Implementation
Q1: What are the key advantages of using a Graph Neural Network over traditional methods for variant interpretation?
Traditional methods often treat genetic variants as independent entities, overlooking the complex biological relationships between genes, proteins, and diseases. GNNs excel by integrating diverse biomedical data into a knowledge graph, allowing them to capture these relationships. For disease-specific prediction, a key advantage is the ability to predict edges between variant and disease nodes within a graph, essentially determining whether a variant is pathogenic in the context of a specific disease [32]. This is a more clinically useful approach than disease-agnostic models.
Q2: My GNN model for pathogenicity prediction is performing well on known disease genes but fails to generalize. What could be wrong?
This is a common challenge. Many models are not calibrated across the entire proteome, meaning their scores are not designed to compare variant deleteriousness in one gene versus another [33]. To address this, consider using a model like popEVE, which leverages both deep evolutionary data and shallow human population data (e.g., from gnomAD) to transform scores to reflect human-specific constraint. This provides a continuous, proteome-wide measure of deleteriousness, enabling more meaningful comparisons across different proteins [33].
Q3: How can I integrate protein structure data into my GNN model for variant interpretation?
You can leverage tools like AlphaFold2 to generate predicted protein structures for features. Rhapsody-2 is a machine learning tool that does precisely this; it uses AlphaFold2-predicted structures to generate a set of descriptors including 17 structural, 21 dynamics-based, and 33 energetics-based features [34]. These features can be incorporated as node or edge attributes in your biological network to provide a more mechanistic interpretation of variant pathogenicity.
Q4: What is the recommended way to handle Variants of Uncertain Significance (VUS) in a GNN framework?
A powerful approach is to build a comprehensive knowledge graph that interconnects various biomedical entities (proteins, diseases, phenotypes, drugs, etc.). You can then train a two-stage architecture: first, a Graph Convolutional Network (GCN) to encode the complex biological relationships in this graph, and second, a neural network classifier to predict disease-specific pathogenicity [32]. This method allows you to integrate domain knowledge and essentially predict new pathogenic links for VUS.
Troubleshooting Guide: Common Experimental Pitfalls and Solutions
Table: Troubleshooting Common GNN Experimental Issues
| Problem | Potential Cause | Solution |
|---|---|---|
| Poor model generalizability to new genes. | Model is overfitting to features of known disease genes and lacks proteome-wide calibration. | Incorporate population data (e.g., from gnomAD) to calibrate evolutionary scores, as done in popEVE, enabling cross-gene comparison of variant deleteriousness [33]. |
| Low contrast in model visualization hinders interpretation. | Color choices for graphs/charts do not meet accessibility standards. | Ensure a minimum contrast ratio of 3:1 for graphical objects like bars in a chart and 4.5:1 for text against backgrounds. Use tools like the WebAIM Contrast Checker [35]. |
| Model performance is biased towards specific ancestries. | Training data from population databases (e.g., GnomAD) over-represents certain groups. | Use methods that rely on coarse measures of variation ("seen" vs. "not seen") rather than precise allele frequencies, which can reduce population structure bias [33]. |
| Difficulty interpreting why the GNN made a specific prediction. | The GNN operates as a "black box," lacking explainability. | Employ interpretable GNN architectures. For pathway identification, combine GNNs with a Genetic Algorithm to identify key sub-netflows, or use methods that provide attention weights to highlight important nodes [36]. |
| Integrating genomic sequence data is computationally challenging. | Processing long DNA sequences into model inputs is non-trivial. | Use a DNA language model like HyenaDNA to generate dynamic gene embeddings directly from nucleotide sequences, which can then be used as features for downstream GNN tasks [36]. |
Experimental Protocols & Data Presentation
Detailed Methodology: A Two-Stage GNN for Disease-Specific Prediction
This protocol is adapted from a study that classified missense variants from ClinVar using a comprehensive knowledge graph [32].
Knowledge Graph Construction:
- Nodes: Incorporate 10+ types of biomedical entities (e.g., Protein, Disease, Drug, Phenotype, Pathway, Biological Process) [32].
- Edges: Connect nodes with 30+ relationship types (e.g., Disease-Gene association, Protein-Protein Interaction (PPI), Drug-Target). Enrich PPIs by classifying them as "transient" or "permanent" using time-course gene expression co-expression data [32].
- Variant Integration: Connect genetic variants to their associated gene nodes. Connect pathogenic variants to their known disease nodes, adding new disease nodes from ClinVar if necessary [32].
Feature Generation:
Model Training (Two-Stage Architecture):
- Stage 1 - Graph Encoding: Train a Graph Convolutional Neural Network (GCN) on the knowledge graph to encode the complex biological relationships [32].
- Stage 2 - Classification: Feed the graph encodings into a standard neural network classifier. The goal is to predict the existence of edges between variant and disease nodes, i.e., disease-specific pathogenicity [32].
Workflow Diagram: Two-Stage GNN for Variant Interpretation
Table 1: Performance of popEVE on Severe Developmental Disorder (SDD) Cohort
This table summarizes the model's ability to capture variant severity by analyzing De Novo Missense Mutations (DNMs) [33].
| Metric | Value / Observation | Context |
|---|---|---|
| Enrichment in SDD Cases | DNMs in cases were consistently shifted toward higher predicted deleteriousness. | Comparison of 31,058 SDD cases vs. unaffected controls [33]. |
| High-Confidence Threshold | Score threshold set at -5.056. | Variants below this threshold have a 99.99% probability of being highly deleterious [33]. |
| Fold Enrichment | 15-fold enriched in the SDD cohort. | Measured for variants below the high-confidence severity threshold [33]. |
| Performance vs. Other Methods | 5x higher enrichment than other methods (e.g., PrimateAI-3D). | Benchmarking against established tools [33]. |
A list of essential databases and tools used in the cited research.
| Resource Name | Type | Function in Research |
|---|---|---|
| ClinVar [32] [34] | Public Archive | Repository of human genetic variants and their relationships to phenotype (disease). |
| gnomAD [33] | Population Database | Catalog of human genetic variation from a large population, used to calibrate variant constraint. |
| AlphaFold DB [34] | Protein Structure DB | Provides predicted 3D structures for proteins, used to generate structural features for variants. |
| CCLE & TCGA [37] | Cancer Datasets | Provide genomic and transcriptomic data for cancer model systems and tumors. |
| DNA Language Models (e.g., HyenaDNA [36], DNABERT [32]) | Computational Tool | Generates numerical embeddings (representations) of DNA sequences for model input. |
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Computational Tools for GNN-based Variant Interpretation
| Item | Function | Example Tools / Databases |
|---|---|---|
| Knowledge Graph Database | Serves as the scaffold for integrating heterogeneous biological data. | Custom-built from databases like Hetionet; typically includes nodes for Protein, Disease, Phenotype, etc. [32]. |
| Variant Effect Predictor | Annotates and predicts the functional consequences of genetic variants. | LOFTEE, VEP (Variant Effect Predictor) [36]. |
| Pathogenicity Scoring Models | Provides pre-computed features or benchmark comparisons for variant deleteriousness. | EVE, ESM-1v, AlphaMissense, popEVE [33] [34]. |
| Graph Neural Network Framework | Provides the software environment to build, train, and test GNN models. | PyTorch Geometric, Deep Graph Library (DGL). GATv2Conv is used for directed graphs with edge attributes [37]. |
| DNA Language Model | Converts raw nucleotide sequences into numerical embeddings that capture genomic context. | HyenaDNA, DNABERT, Nucleotide Transformer [32] [36]. |
Knowledge Graph Structure Diagram
Leveraging AlphaFold2 and ESM Models for Structural Feature Extraction
Frequently Asked Questions
Q1: What is the fundamental difference between AlphaFold2 and ESMFold in their approach to structure prediction?
A1: The core difference lies in their use of evolutionary information. AlphaFold2 relies heavily on Multiple Sequence Alignments (MSAs) to find homologous sequences, which requires querying large biological databases and can be computationally intensive [38]. In contrast, ESMFold is a single-sequence method that uses a pre-trained protein language model (ESM-2) to infer evolutionary patterns directly from the primary sequence, making it a standalone and much faster tool that does not require external database searches [39].
Q2: My AlphaFold2 run failed with an error: "Could not find HHsearch database /data/pdb70". What does this mean and how can I resolve it?
A2: This error indicates a missing or incorrectly configured homology detection database, which AlphaFold2 requires for its template-based modeling step [40]. To resolve this:
- Check Database Installation: Ensure all necessary databases (including pdb70) have been fully downloaded and are in the correct directory path specified in your AlphaFold2 installation.
- Use a Managed Service: Consider using a managed platform like the Galaxy server, which offers a pre-configured AlphaFold2 environment with all dependencies already installed [40].
- Verify File Permissions: Confirm that the user running AlphaFold2 has read permissions for the database files.
Q3: For predicting the impact of a missense variant on protein structure, should I use AlphaFold2 or AlphaMissense?
A3: These tools have distinct purposes. AlphaFold2 is designed to predict the 3D structure of a protein from its sequence [38]. To assess a variant, you would need to run it twice (for the wild-type and mutant sequences) and compare the outputs. AlphaMissense, built on AlphaFold's architecture, is a specialized tool that directly predicts the pathogenicity of missense variants by analyzing sequence and evolutionary context, providing a simple pathogenicity score [41]. For high-throughput variant screening, AlphaMissense is more efficient. However, for detailed, atomistic insight into how a specific variant alters the structure, running AlphaFold2 remains valuable.
Q4: The predicted structure for my protein of interest has low confidence scores (pLDDT) in a specific loop region. How should I interpret this?
A4: Low pLDDT scores (typically below 70) indicate regions where the model is less reliable. These often correspond to intrinsically disordered regions (IDRs) or flexible loops that do not have a single, fixed conformation in solution [38]. In the context of missense variants, you should:
- Interpret with Caution: Be wary of over-interpreting structural changes due to mutations in these low-confidence regions.
- Use as a Hypothesis: The disordered nature itself can be biologically significant. The prediction can serve as a starting hypothesis, but these regions may require experimental validation.
Q5: Can I use ESMFold to predict multiple conformations or alternative folds for a protein?
A5: Current versions of ESMFold, like AlphaFold2, are primarily designed to predict a single, static protein structure [42]. They often struggle with proteins that have alternative conformations or are known as "metamorphic" proteins that can switch between different folds [42]. This is a known limitation of these AI-based prediction methods, and predicting the full conformational landscape of a protein remains an active area of research.
Troubleshooting Guides
Issue 1: Handling Low Confidence Predictions in AlphaFold2/ESMFold
Problem: A significant portion of your predicted model, or an entire domain, has low confidence metrics (pLDDT in AlphaFold2).
Diagnosis and Solutions:
Step 1: Verify the Input Sequence.
Step 2: Analyze the MSA (AlphaFold2 Specific).
- Low confidence often correlates with a shallow or poor-quality Multiple Sequence Alignment. Check the depth and diversity of the MSA generated by AlphaFold2. A lack of evolutionary homologs makes structure prediction more difficult [38].
Step 3: Cross-validate with ESMFold.
- Run the same sequence through ESMFold. As it uses a different methodology, it can serve as an independent check. Consistent low-confidence regions across both methods strongly suggest intrinsic disorder or a lack of evolutionary constraints in that area [39].
Step 4: Interpret Biologically.
- Map the low-confidence regions against known protein domains and functional annotations. They may be flexible linkers or disordered regions that are functionally important despite lacking a fixed structure.
Issue 2: AlphaMissense Misclassifies a Known Benign Variant as Pathogenic
Problem: When classifying missense variants for your gene of interest, AlphaMissense produces a high pathogenicity score for a variant that has been experimentally confirmed to be benign.
Diagnosis and Solutions:
Step 1: Understand the Limitation.
- This is a documented limitation. AlphaMissense can conflate a variant's effect on protein function with its relevance to disease. It may correctly predict that a variant is damaging to a protein's biophysical properties, but that change may not be the mechanism of disease for that specific gene [41].
Step 2: Conduct Structural Analysis with AlphaFold2.
- Use AlphaFold2 to model the wild-type and mutant protein structures.
- Compare the two models to see if the variant causes significant destabilization, disrupts a key active site, or interferes with critical protein-protein interactions. This provides mechanistic context beyond a simple pathogenicity score.
Step 3: Consult Multiple Predictors and Experimental Data.
- Do not rely on AlphaMissense alone. Aggregate predictions from other state-of-the-art supervised and unsupervised tools [41].
- Prioritize evidence from high-throughput experimental assays (MAVEs) if available for your gene, but be aware that they can sometimes be discordant with clinical labels [41].
Final Recommendation: As concluded in recent research, "AlphaMissense cannot replace wet lab studies as the rate of erroneous predictions is relatively high" [41]. Use it as a powerful prioritization tool, not a final arbiter.
Comparative Data for Tool Selection
The table below summarizes the key quantitative and technical differences between AlphaFold2, ESMFold, and AlphaMissense to guide your experimental planning.
Table 1: Comparison of AlphaFold2, ESMFold, and AlphaMissense
| Feature | AlphaFold2 | ESMFold | AlphaMissense |
|---|---|---|---|
| Primary Function | 3D Protein Structure Prediction [38] | 3D Protein Structure Prediction [39] | Missense Variant Pathogenicity Scoring [41] |
| Core Methodology | MSA-based & Physical Geometry [38] | Single-sequence Protein Language Model [39] | Unsupervised Deep Learning (based on AlphaFold) [41] |
| Key Input | Amino Acid Sequence (for MSA generation) [38] | Amino Acid Sequence (single) [39] | Amino Acid Sequence & Variant Position [41] |
| Key Output | 3D Atomic Coordinates, pLDDT Confidence Metric [38] | 3D Atomic Coordinates [39] | Pathogenicity Score (0-1) [41] |
| Relative Speed | Slow (hours/days, due to MSA) [39] | Fast (order of magnitude faster than AlphaFold2) [39] | Very Fast (for variant scoring) |
| Recommended Application | High-accuracy static structures; detailed mutant analysis | High-throughput screening of metagenomic proteins; quick structural overview [39] | Prioritizing pathogenic variants in large-scale genetic studies [41] |
Table 2: ESM Model Family Overview
| Model | Parameters | Key Capability | Context Length |
|---|---|---|---|
| ESM-2 | 650M to 15B [39] | General protein language model, base for ESMFold [39] | 1026 [39] |
| ESMFold | 8M (folding head) [39] | End-to-end atomic structure prediction [39] | 1026 [39] |
| ESM Cambrian | 300M, 600M, 6B [45] | Next-generation representation learning, outperforms ESM-2 [45] | 2048 (after training) [45] |
Experimental Protocols
Protocol 1: Comparative Structural Analysis of a Missense Variant using AlphaFold2
Objective: To generate and compare the 3D structures of wild-type and mutant proteins to hypothesize the molecular mechanism of a missense variant.
Materials:
- Wild-type protein sequence in FASTA format.
- Mutant protein sequence (simulated by introducing the single amino acid change into the wild-type FASTA).
- Computing environment with AlphaFold2 installed and configured.
Methodology:
- Input Preparation:
- Create two separate FASTA files.
- Wild-type:
>Protein_X_WT [organism=Homo sapiens] - Mutant:
>Protein_X_MUT [organism=Homo sapiens] - Ensure the sequence is in valid FASTA format, with no line breaks in the header [46].
Structure Prediction:
- Run AlphaFold2 independently for both the wild-type and mutant FASTA files. This process involves MSA creation, template searching, and structure generation via the Evoformer and structure module [38].
- The output will be PDB files for each and a per-residue confidence metric (pLDDT).
Structural Comparison & Analysis:
- Superimposition: Load both PDB files into molecular visualization software (e.g., PyMOL, ChimeraX) and superimpose the models based on conserved regions.
- Root-mean-square deviation (RMSD): Calculate the global and local RMSD to quantify structural differences. AlphaFold2 demonstrated a median backbone accuracy of 0.96 Å in CASP14 [38].
- Visual Inspection: Manually inspect the mutation site for changes in:
- Side-chain conformation and contacts.
- Local backbone geometry.
- Disruption of hydrogen bonds, salt bridges, or hydrophobic cores.
- Obstruction of functional sites (e.g., active sites, binding pockets).
Protocol 2: High-Throughput Variant Prioritization using AlphaMissense and ESMFold
Objective: To rapidly screen a list of missense variants from a genetic study to prioritize candidates for further experimental validation.
Materials:
- A list of missense variants (e.g., from whole-exome sequencing) with their gene names and amino acid changes.
- Access to the AlphaMissense database or model.
- Computing environment capable of running ESMFold.
Methodology:
- Pathogenicity Scoring:
- Query the pre-computed AlphaMissense database for your variants to obtain pathogenicity scores.
- Apply the recommended threshold (score > 0.56) to flag likely pathogenic variants [41].
Structural Context Validation:
- For the shortlisted high-scoring variants, run ESMFold for the corresponding wild-type protein sequence to quickly obtain a structural model.
- Note: ESMFold's speed allows you to do this for dozens to hundreds of proteins in a practical timeframe [39].
Integrative Analysis:
- Map the variant position onto the ESMFold-predicted structure.
- Assess the structural context: Is the residue buried in the core, exposed on the surface, or part of a known functional motif? This step helps to distinguish variants that are likely to be destabilizing from those that might have more subtle functional effects.
Workflow Visualization
The following diagram illustrates the integrated workflow for classifying pathogenic missense variants using the tools discussed in this guide.
The Scientist's Toolkit
Table 3: Essential Research Reagents and Resources
| Item / Resource | Function / Description | Relevance to Experimental Workflow |
|---|---|---|
| UniProt Knowledgebase | Comprehensive resource for protein sequences and functional information. | Source of canonical wild-type protein sequences for input into prediction models [45]. |
| Protein Data Bank (PDB) | Repository for experimentally determined 3D structures of proteins. | Used for validation of computational models and for template-based modeling in AlphaFold2 [47]. |
| FASTA Format File | Standard text-based format for representing nucleotide or amino acid sequences. | The required input format for all tools discussed (AlphaFold2, ESMFold). The header must start with ">" [46] [43]. |
| AlphaFold2 Database | Pre-computed protein structure predictions for the human proteome and other key organisms. | Allows researchers to download predicted structures without running the model, saving computational time. |
| AlphaMissense Database | Pre-computed pathogenicity scores for a vast number of possible human missense variants. | Enables instant lookup of variant scores for prioritization without running the model locally [41]. |
| ESM-2 / ESM Cambrian Models | Pre-trained protein language models available via Hugging Face Transformers or EvolutionaryScale. | Provides the foundational understanding of protein sequences used by ESMFold; can be fine-tuned for specific tasks [39] [45]. |
Frequently Asked Questions (FAQs)
Q1: What are the primary advantages of using a knowledge graph over traditional databases for variant pathogenicity prediction? Knowledge graphs (KGs) integrate disparate biomedical data into a unified network, enabling the discovery of complex, multi-hop relationships that are not apparent in isolated databases [48] [49]. They provide a semantically rich structure that captures diverse entity types (e.g., genes, diseases, drugs, phenotypes) and their relationships, offering a more holistic context for interpreting variants [50] [49]. Crucially, path-based reasoning on KGs can generate transparent and biologically meaningful explanations for predictions, moving beyond the "black-box" nature of some complex models [48] [51].
Q2: My model for predicting pathogenic gene interactions lacks interpretability. How can a knowledge graph help? You can employ a path-based approach, such as the ARBOCK framework, which mines frequently observed connection patterns (metapaths) between known pathogenic gene pairs in a KG [48] [52]. These patterns are used to train an interpretable decision set model—a set of IF-THEN rules. When a new gene pair is predicted to be pathogenic, the model can provide the specific subgraph (the entities and relationships) that led to the conclusion, offering a clear, visual explanation grounded in biological knowledge [48].
Q3: How can I make pathogenicity predictions disease-specific instead of general? To achieve disease-specific prediction, structure your knowledge graph to include clear connections between variants and specific diseases. Then, you can train a classifier, such as a graph neural network, to essentially predict edges between variant and disease nodes [53]. This approach allows the model to learn the contextual patterns of pathogenicity unique to a particular disease, rather than relying on a single, generalized threshold [53].
Q4: What are some common data integration challenges when building a biomedical knowledge graph? A major challenge is disease entity resolution, as diseases are represented differently across various ontologies (e.g., MONDO, ICD, Orphanet) and clinical guidelines [49]. Harmonizing these into a consistent schema is critical. Furthermore, integrating omics data with ontological knowledge requires robust ETL (Extract, Transform, Load) pipelines and often the development of custom ontologies, such as a chromosomal location ontology, to bridge genomic features with broader biomedical concepts [54] [49].
Q5: How can I handle the "black-box" nature of deep learning models for variant interpretation? Implement an Explainable AI (XAI) framework that uses a knowledge graph as its knowledge base [51]. After a deep learning model makes a prediction, the KG can be used to generate human-readable explanations. This involves translating the important nodes and paths from the graph that contributed to the prediction into textual explanations that align with how clinicians investigate variants, for example, by referencing guidelines like those from the American College of Medical Genetics and Genomics (ACMG) [51].
Troubleshooting Guides
Issue 1: Poor Predictive Performance on Novel Gene Pairs
Problem: Your KG model fails to identify novel pathogenic gene interactions outside of its training data.
Solution:
- Expand KG Connectivity: Ensure your KG integrates diverse and complementary biological networks. A gene-centric KG like BOCK showed that while individual networks (e.g., protein-protein interactions, co-expression) only partially connect known pathogenic pairs, their integration allows paths of lengths ≤3 to connect all pairs [48]. Incorporate networks such as:
- Leverage Multi-Hop Paths: Do not restrict your model to direct connections. Use a path traversal algorithm with a cutoff of 3 or 4 to capture long-range, indirect relationships between entities [48].
- Incorporate Pre-trained Embeddings: Enhance node features by integrating embeddings from biomedical language models (e.g., BioBERT) or genomic foundation models (e.g., HyenaDNA, Nucleotide Transformer) to provide rich, contextual information directly from textual descriptions or genomic sequences [53].
Issue 2: Inability to Generate Clinically Actionable Explanations
Problem: The model's predictions lack transparent explanations that clinicians can understand and trust.
Solution:
- Adopt a Rule-Based Model: Use association rule learning on the metapaths within your KG. The ARBOCK method generates a decision set of rules, where each rule is a specific pattern of connections frequently found in pathogenic cases [48] [52].
- Generate Instance-Specific Subgraphs: For every positive prediction, extract and visualize the exact subgraph of the KG that connects the gene pair, highlighting the specific biological entities and relationships that led to the conclusion [48].
- Align Explanations with Clinical Guidelines: Map the KG-derived explanations to established clinical frameworks. The XAI approach in [51] defines "X-Rules" that convert high-contribution nodes in the graph into text, ensuring the output references trusted sources like ClinVar and follows the logic of guidelines like those from the ACMG.
Issue 3: KG Fails to Capture Disease-Specific Variant Effects
Problem: Your pathogenicity predictions are not sensitive to the disease context.
Solution:
- Refine Graph Structure: Explicitly connect variants to their associated diseases. This can be done by linking variant nodes to disease nodes using edges from curated sources like ClinVar [53] [50].
- Implement a Disease-Specific Classifier: Train a two-stage model where a Graph Convolutional Neural Network (GCNN) first encodes the complex relationships in the KG, and a subsequent neural network classifier predicts the "variant-causes-disease" edge [53]. This forces the model to learn in the context of a specific disease.
Problem: The process of merging different databases, ontologies, and omics data into a coherent KG schema is error-prone and inefficient.
Solution:
- Use a Foundational Scaffold: Build your KG on top of a unified base ontology like the Unified Biomedical Knowledge Graph (UBKG) or UMLS, which provides a pre-integrated framework for hundreds of biomedical ontologies [54] [49].
- Develop Modular Ingestion Protocols: Follow the practice of frameworks like Petagraph, which uses modular protocols to add new omics datasets to the UBKG base. This allows for consistent and reproducible integration of new data sources [54].
- Create Hub Nodes: For core entities like genes and variants, create central hub nodes that link to their corresponding entries across all integrated databases. This simplifies data access and cross-referencing [51].
Experimental Protocols
Protocol 1: Constructing a Disease-Specific Pathogenicity Predictor Using a GCNN
Objective: To predict whether a missense variant is pathogenic for a specific disease using a graph neural network.
Methodology:
- Knowledge Graph Preparation:
- Obtain a base KG (e.g., from resources like PrimeKG [49] or build your own integrating genes, proteins, diseases, drugs, and phenotypes).
- Enrich the graph by splitting protein nodes into separate gene and protein nodes, connecting them with a
codes_foredge [53]. - Add variant nodes from ClinVar and link each variant to its corresponding gene with a
located_inedge. Connect pathogenic variants to their associated disease nodes with acausesedge [53].
- Feature Generation:
- Node Features: Generate initial feature vectors for all nodes using a biomedical language model like BioBERT. Use textual descriptions of the entities (e.g., disease summaries, gene names) as input [53].
- Variant Features: Use DNA language models (e.g., HyenaDNA, Nucleotide Transformer) to generate embeddings for variant nodes based on the genomic sequence surrounding the variant locus [53].
- Model Training:
- Implement a two-stage architecture:
- Stage 1 (Graph Encoding): A Graph Convolutional Neural Network (GCNN) takes the KG with its node features and learns to generate dense, low-dimensional representations (embeddings) for every node, capturing their topological context [53].
- Stage 2 (Classification): A neural network classifier takes the embeddings of a variant node and a disease node and predicts the probability of a
causesedge existing between them [53].
- Train the model using known variant-disease associations from ClinVar as positive examples and benign variants as negative examples.
- Implement a two-stage architecture:
Protocol 2: Implementing an Interpretable Rule-Based Predictor for Gene Interactions
Objective: To predict pathogenic gene-gene interactions with explainable rules derived from knowledge graph paths.
Methodology:
- Path Extraction:
- From your KG (e.g., BOCK [48]), traverse all paths up to a length of 3 that connect known pathogenic gene pairs from a database like OLIDA. Ignore paths that go directly through "Disease" or "OligogenicCombination" nodes to avoid data leakage [48] [52].
- For each path, abstract it into a metapath—a sequence of node and edge types (e.g., Gene–interactswith–Gene–participatesin–BiologicalProcess–participates_in–Gene).
- Rule Mining:
- Use association rule learning to identify frequently occurring metapath patterns in the set of pathogenic gene pairs [48].
- These patterns form the IF part of the rules (e.g.,
IF Gene_A and Gene_B are connected by metapath X).
- Model Building:
- Combine the discovered rules into a Decision Set classifier [48] [52]. This is an unordered collection of IF-THEN rules where a gene pair is predicted as pathogenic if it satisfies any of the rules.
- The model's explanation for a prediction is simply the specific rule (and the corresponding concrete subgraph in the KG) that was triggered.
Research Reagent Solutions
Table 1: Essential Resources for Knowledge Graph-Based Variant Research
| Resource Name | Type | Primary Function in Research | Key Features/Description |
|---|---|---|---|
| BOCK [48] [52] | Knowledge Graph | Exploring disease-causing genetic interactions. | Integrates oligogenic disease data (OLIDA) with multi-scale biological networks; designed for interpretable rule mining. |
| PrimeKG [49] | Knowledge Graph | Precision medicine analyses across a wide range of diseases. | Covers 17,080 diseases with multi-modal relationships (proteins, pathways, phenotypes, drugs including off-label use). |
| Petagraph [54] | Knowledge Graph Framework | Large-scale, unifying framework for biomolecular data. | Built on UBKG; embeds omics data into an ontological scaffold; highly modular for custom use cases. |
| AIMedGraph [50] | Knowledge Graph | Precision medicine, focusing on variant-drug relationships. | Integrates genes, variants, diseases, drugs, and clinical trials with evidence-based pathogenicity and drug susceptibility. |
| IDDB Xtra [55] | Specialized Database & KG | Infertility disease mechanism research and variant interpretation. | Manually curated genes, variants, and phenotypes for infertility; includes a dedicated infertility knowledge graph. |
| AlphaFold2 [8] | Structural Prediction Tool | Providing protein structural features for variant analysis. | Generates high-accuracy 3D protein structures; used to compute structural features for pathogenicity predictors. |
| BioBERT [53] | Language Model | Generating semantic node embeddings for the KG. | Pre-trained on biomedical literature; creates feature vectors from textual descriptions of KG entities. |
| DNA Language Models (e.g., HyenaDNA [53]) | Language Model | Generating variant embeddings from genomic sequence. | Captures genomic context directly from nucleotide sequences to enrich variant node features in the KG. |
| ClinVar [50] [51] | Clinical Database | Source of curated variant-pathogenicity associations. | Essential for training and validating disease-specific pathogenicity predictors; provides clinical ground truth. |
| DisGeNET [49] | Knowledge Base | Source of gene-disease and variant-disease associations. | Provides expertly curated relationships to populate and validate connections within the knowledge graph. |
Workflow and Pathway Visualizations
Diagram 1: Workflow for Disease-Specific Variant Pathogenicity Prediction
Diagram 2: Logic of an Interpretable Rule-Based Prediction
Mode-of-Action Prediction with SE(3)-Equivariant Graph Neural Networks
Accurately predicting the pathogenicity of missense variants is a fundamental challenge in clinical genetics and drug discovery [41]. SE(3)-equivariant Graph Neural Networks (GNNs) represent a transformative approach for this task, as they inherently respect the 3D geometric symmetries of molecular structures [56]. This technical support guide addresses common implementation challenges and provides proven solutions for researchers developing these models to classify pathogenic missense variants and elucidate their molecular mechanisms of action.
Frequently Asked Questions (FAQs)
Q1: Why should I use an SE(3)-equivariant GNN instead of a standard invariant model for variant effect prediction? Standard GNNs act only on scalar features (e.g., interatomic distances) and are invariant to rotations. While this ensures rotational invariance of the output, it discards all angular information. SE(3)-equivariant GNNs use features comprised of geometric tensors (scalars, vectors) and equivariant operations [56]. This allows the network to learn from both radial and angular information in a 3D atomic environment, leading to a more information-rich representation and significantly greater data efficiency [56].
Q2: My equivariant model achieves high accuracy but its predictions are a "black box." How can I interpret which structural features lead to a pathogenic classification? Interpretability is a known challenge for complex deep learning models [41]. To address this, integrate perturbation-based explanation methods like Substructure Mask Explanation (SME). SME identifies crucial substructures by systematically masking chemically meaningful fragments (e.g., BRICS substructures, functional groups) and monitoring prediction changes [57]. This provides interpretations that align with chemist intuition by highlighting functional groups or protein domains associated with pathogenicity.
Q3: During training, my model fails to converge when predicting on novel variants in genes absent from its training set. What could be wrong? This is a generalization issue. Supervised models trained on clinically labeled variants from databases like ClinVar can exhibit bias and fail to generalize to novel genes [41] [33]. Consider incorporating unsupervised or self-supervised approaches. Models like AlphaMissense (trained on evolutionary and structural data) or popEVE (which combines evolutionary sequences with human population data) are designed to make predictions across the proteome without relying on pre-existing clinical labels for every gene [41] [33].
Q4: How can I explicitly model molecular interactions, such as those in protein-ligand complexes, within my GNN architecture? Standard GNNs for single molecules may fail to capture intermolecular interactions. Use an architecture like SolvGNN, which employs a dual-graph system [58]. It combines atomic-level (local) graph convolution with molecular-level (global) message passing through an explicitly defined molecular interaction network. This allows the model to learn the specific interactions between different molecular components that influence biological activity.
Troubleshooting Guides
Poor Data Efficiency and Model Performance
Symptoms: Model requires thousands of training examples to achieve acceptable performance; poor accuracy on small datasets.
| Potential Cause | Solution | Evidence/Protocol |
|---|---|---|
| Invariant Model Architecture | Replace invariant convolutions with SE(3)-equivariant convolutions that operate on geometric tensors. | The NequIP model demonstrated state-of-the-art accuracy with up to three orders of magnitude fewer training data than other methods by using equivariant features [56]. |
| Inadequate Molecular Representation | Enhance the graph representation by incorporating non-covalent interactions (e.g., hydrogen bonds, electrostatic interactions) beyond just covalent bonds. | Studies show that integrating non-covalent interactions into graph representations notably enhances GNN performance for molecular property prediction [59]. |
| Simple Feature Set | Integrate Kolmogorov-Arnold Networks (KANs) into the GNN components. KANs use learnable univariate functions on edges instead of fixed activation functions, improving expressivity and parameter efficiency [59]. | KA-GNNs, which integrate KANs into node embedding, message passing, and readout, have consistently outperformed conventional GNNs in molecular benchmarks [59]. |
Experimental Protocol for Improved Data Efficiency:
- Model Selection: Implement an equivariant architecture like NequIP [56] or a KA-GNN [59].
- Feature Definition: Define node features using atomic number and type; for equivariant models, use vector features like relative position.
- Training: Train the model on a deliberately small subset (e.g., a few hundred samples) of your variant data.
- Validation: Benchmark its performance against a larger supervised model to quantify gains in data efficiency.
Lack of Model Interpretability
Symptoms: Inability to understand which atoms, residues, or substructures the model uses for prediction; results are not chemically intuitive.
Solution: Implement the Substructure Mask Explanation (SME) method [57].
Experimental Protocol for SME:
- Fragmentation: For each protein structure or molecule in your dataset, segment it into chemically meaningful substructures using a predefined scheme like BRICS or a functional group dictionary.
- Masking and Inference: For each segmented molecule, systematically mask out each substructure one at a time (set its features to zero).
- Prediction Shift: Run the masked molecules through your trained GNN and record the change in the predicted pathogenicity score for each masking operation.
- Attribution Calculation: Calculate the attribution score for each substructure based on the magnitude of the prediction shift. A large change indicates high importance.
- Validation: Correlate high-attribution substructures with known functional domains or clinically validated pathogenic regions (e.g., from databases like ClinVar).
Handling Multi-Component Molecular Systems
Symptoms: Model performs poorly when predicting interactions in systems with multiple molecules (e.g., protein-ligand binding, protein complexes).
Solution: Adopt an explicit molecular interaction GNN architecture [58].
Implementation Guide:
- Graph Construction: Create a two-level graph.
- Local Graph: Standard atomic-level graph with nodes as atoms and edges as covalent bonds.
- Global Interaction Graph: A graph where each node is an entire molecule (e.g., protein, drug molecule). Edges represent potential or known interactions between these molecules.
- Dual Message Passing:
- Perform standard message passing within each local atomic graph.
- Perform higher-level message passing on the global interaction graph to allow information exchange between molecules.
- Feature Readout: Combine node embeddings from both the local and global graphs to form a final representation for property prediction (e.g., binding affinity, variant pathogenicity).
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential computational tools and resources for MoA prediction with GNNs.
| Tool/Resource Name | Type | Function in Experiment |
|---|---|---|
| e3nn [56] | Software Library | Provides primitives and functions for building SE(3)-equivariant neural networks in PyTorch. Essential for implementing models like NequIP. |
| NequIP [56] | GNN Model | An E(3)-equivariant interatomic potential for learning from atomic structures with high data efficiency. A reference architecture for 3D molecular learning. |
| AlphaMissense [41] | Pre-trained Predictor | An unsupervised deep learning model that predicts missense variant pathogenicity using protein structure and evolutionary data. Useful for benchmarking and generating baseline scores. |
| SME (Substructure Mask Explanation) [57] | Interpretation Method | A perturbation-based method to explain GNN predictions by attributing importance to chemically meaningful substructures. |
| KA-GNN [59] | GNN Architecture | A GNN framework integrating Kolmogorov-Arnold Networks (KANs) for enhanced expressivity and interpretability in molecular property prediction. |
| SolvGNN [58] | GNN Architecture | An architecture designed to explicitly capture molecular interactions in multi-component systems via a dual local-and-global graph structure. |
| popEVE [33] | Prediction Model | A deep generative model that combines evolutionary and population data to provide proteome-wide, calibrated scores for variant deleteriousness. |
Overcoming Classification Challenges: VUS Resolution and Complex Mode-of-Action
Strategies for Variants of Uncertain Significance (VUS) Resolution
In the field of clinical genomics, Variants of Uncertain Significance (VUS) represent a critical diagnostic bottleneck. A VUS is a genetic variant for which the association with disease risk is unclear—it is neither confidently classified as pathogenic (disease-causing) nor benign. The resolution of VUS is therefore paramount for precise diagnosis, accurate risk assessment, and guiding therapeutic decisions in genetic disorders. This technical support guide outlines systematic strategies for VUS resolution, providing researchers and clinicians with standardized methodologies to overcome this challenge.
Foundational Framework: The ACMG/AMP Classification System
The cornerstone of modern variant interpretation is the five-tier classification system established by the American College of Medical Genetics and Genomics and the Association for Molecular Pathology (ACMG/AMP).
| Classification Tier | Clinical Significance | Typical Probability of Pathogenicity |
|---|---|---|
| Pathogenic | Disease-causing | >99% |
| Likely Pathogenic | Very high likelihood of being disease-causing | ~90% (Proposed) |
| Uncertain Significance | Unknown clinical significance | N/A |
| Likely Benign | Very high likelihood of being benign | ~90% (Proposed) |
| Benign | Not disease-causing | <1% |
This framework provides the logical structure for the VUS resolution process, which involves gathering evidence to reclassify a VUS into one of the other four categories.
The following table summarizes key types of evidence used in variant classification, highlighting those frequently underutilized for VUS according to recent analysis:
| Evidence Type | ACMG/AMP Code | Description | Reported Usage Frequency in VUS [60] |
|---|---|---|---|
| Population Data | PM2 | Allele frequency too low for disorder | Most widely used (as PM2_Supporting) |
| Computational/In Silico | PP3 | Multiple lines of computational evidence support deleterious effect | Used frequently |
| Computational/In Silico | BP4 | Multiple lines of computational evidence suggest no impact | Used frequently |
| Functional Data | PS3 | Well-established functional studies supportive of damaging effect | Underutilized |
| Segregation Data | PP1 | Co-segregation with disease in multiple affected family members | Underutilized |
| De Novo Observation | PS2 | Observed de novo (with confirmed paternity and maternity) | Underutilized |
| Missense in Gene | PP2 | Missense variant in a gene with a low rate of benign missense variation | Used frequently |
| Case-Control Data | PS4 | Prevalence in affecteds significantly higher than in controls | Underutilized |
Experimental Protocols for Evidence Generation
FAQ: What are the first steps I should take when trying to resolve a VUS?
The initial workflow involves a structured, multi-step process to gather evidence from public resources and clinical data before proceeding to functional assays.
Protocol 1: Comprehensive Database Interrogation
Objective: To collate existing population frequency, computational prediction, and literature-based evidence for the VUS.
Population Frequency Filtering:
- Tool: gnomAD (Genome Aggregation Database)
- Method: Query the allele frequency of your variant. Variants with high allele frequencies in population databases (e.g., >1% for dominant disorders) are unlikely to be pathogenic. The stringent application of allele frequency filters (PM2 criterion) is one of the most widely used pieces of evidence for VUS. [60]
Computational Prediction (PP3/BP4 Criteria):
- Tools: Utilize a suite of in silico prediction tools (e.g., SIFT, PolyPhen-2, REVEL, CADD). [61] [62]
- Method: Run the variant through multiple tools. Consistent predictions across tools (e.g., "deleterious") strengthen the evidence. The ACMG/AMP PP3 criterion is met when multiple lines of computational evidence support a deleterious effect, while BP4 is used when they suggest neutrality. [60]
Variant Database Cross-Referencing:
- Tools: ClinVar, ClinGen, HGMD (Human Gene Mutation Database), COSMIC (for cancer).
- Method: Check if the variant has been previously reported and classified. Data from reputable sources (ClinGen) can provide existing evidence or even support the use of the PS1 (established pathogenic variant) criterion. [63]
Protocol 2: Familial Segregation Analysis (PP1 Criterion)
Objective: To determine if the variant co-segregates with the disease phenotype within a family.
- Sample Collection: Obtain DNA samples from multiple affected and unaffected family members.
- Genotyping: Sequence the specific gene or perform broader testing (e.g., whole exome sequencing) to genotype the VUS in all family members.
- Statistical Analysis: Calculate a LOD (Logarithm of Odds) score to statistically evaluate the likelihood of co-segregation. The stronger the co-segregation (e.g., seen in all affected members and no unaffected members), the stronger the evidence for pathogenicity (PP1). This is a frequently underutilized but powerful strategy for VUS resolution. [60]
Protocol 3: Functional Assays (PS3/BS3 Criteria)
Objective: To provide direct experimental evidence of the variant's impact on protein function.
Methodology Overview:
- Plasmid Construction: Create expression vectors for both the wild-type and VUS-containing gene.
- Cell Culture & Transfection: Use an appropriate cell line (e.g., HEK293) and transfect with the constructed plasmids.
- Functional Readouts: The specific assay depends on the protein's known function.
- Enzymatic Activity: Measure activity if the protein is an enzyme.
- Protein-Protein Interaction: Use co-immunoprecipitation (Co-IP) or yeast-two-hybrid assays.
- Localization: Use immunofluorescence to detect mislocalization.
- Splicing Assays: Minigene assays can determine if the variant disrupts normal RNA splicing.
- Data Analysis: Compare the function of the variant protein to the wild-type and known pathogenic controls. A result consistent with a damaging effect supports the PS3 criterion, while a result showing normal function supports the BS3 (benign) criterion. [60]
Advanced Computational Tools and AI
FAQ: How can Artificial Intelligence (AI) and machine learning help resolve VUS?
AI and machine learning models are increasingly powerful for variant prioritization and interpretation, especially in challenging cases. [64] [62]
- Ensemble Predictors: Tools like REVEL and CADD combine scores from multiple individual algorithms into a more robust meta-score, improving the prediction of pathogenic missense variants. [61] [62]
- Disease-Specific Models: Newer tools are being trained on specific, challenging datasets. For example, VarPPUD is a random forest-based model trained on variants from the Undiagnosed Diseases Network (UDN). It is specifically designed to distinguish truly pathogenic variants from other deleterious but non-causal candidates in difficult-to-diagnose cases, showing an 18.6% improvement in accuracy over traditional predictors. [61]
- Splicing Prediction: Deep learning models (e.g., CADD-Splice) can more accurately predict the impact of variants on RNA splicing, a common disease mechanism. [64]
Comparison of Advanced Computational Tools
| Tool Name | Underlying Model | Primary Application | Key Strength |
|---|---|---|---|
| REVEL [61] | Ensemble Machine Learning | Missense Pathogenicity | Integrates multiple in silico scores |
| CADD [62] | Support Vector Machine | Genomic Variant Prioritization | Combines diverse genomic annotations |
| VarPPUD [61] | Random Forest | VUS Post-Prioritization | Trained on real-world unsolved cases; improved interpretability |
| CADD-Splice [64] | Deep Learning | Splice-Altering Variant Prediction | High accuracy for non-coding effects |
The Scientist's Toolkit: Research Reagent Solutions
Successful VUS resolution relies on a suite of key reagents and tools.
| Research Reagent / Tool | Function in VUS Resolution | Example/Provider |
|---|---|---|
| ACMG/AMP Guidelines [21] | Provides the standardized evidence-based framework for variant classification. | ClinGen SVI Recommendations [63] |
| Control DNA Samples | Essential positive/negative controls for functional and segregation studies. | Coriell Institute, ATCC |
| Expression Vectors | Backbone for constructing wild-type and mutant clones for functional assays. | Addgene, commercial vectors (e.g., pcDNA3.1) |
| Genome Databases | Provide population frequency and control data to filter common polymorphisms. | gnomAD, 1000 Genomes |
| Variant Databases | Centralize known variant classifications and literature evidence. | ClinVar, ClinGen, LOVD |
| In Silico Prediction Suites | Computational first pass to predict variant impact (PP3/BP4 evidence). | REVEL, CADD, PolyPhen-2, SIFT |
| Phenotype-Gene Prioritization Tools | Link patient symptoms to likely causative genes to prioritize VUS. | Phen2Gene [60] |
Resolving a VUS is rarely achieved by a single experiment. It is an iterative process of evidence accumulation, requiring integration of clinical, familial, populational, computational, and functional data within the ACMG/AMP framework. Furthermore, data sharing through curated public databases like ClinVar and ClinGen is critical for the global community to advance the interpretation of VUS, ultimately improving diagnostic yields and patient care.
Frequently Asked Questions
FAQ 1: Why is differentiating between GOF and LOF mechanisms critical for therapy development? Therapeutic strategies must align with the underlying molecular mechanism. LOF variants are often treatable with approaches that restore function, such as gene replacement therapy. In contrast, GOF and DN variants typically require interventions that suppress or inhibit the aberrant protein activity, such as small-molecule inhibitors, gene silencing, or gene editing [65]. Using an incorrect therapeutic strategy can be ineffective or even harmful.
FAQ 2: My gene of interest shows both dominant and recessive inheritance patterns. What does this suggest? This pattern, known as mixed inheritance, is a strong indicator of intragenic mechanistic heterogeneity. This means different variants within the same gene cause disease through distinct molecular mechanisms. Recent research indicates that 43% of dominant and 49% of mixed-inheritance genes harbor both LOF and non-LOF mechanisms [65]. Your experimental design should account for the possibility that variants may need to be analyzed and treated on a case-by-case basis.
FAQ 3: Current variant effect predictors (VEPs) perform poorly on my gene. What could be the reason? Many computational predictors are systematically biased toward identifying LOF variants and show reduced accuracy for GOF and DN mutations [66]. This is because they often rely on features like severe protein destabilization, which is characteristic of LOF but not non-LOF variants. For genes where non-LOF mechanisms are suspected, you should prioritize methods specifically designed to detect them, such as those analyzing 3D variant clustering [66].
FAQ 4: How can I experimentally distinguish between a LOF and a folding-deficient variant? A variant that reduces protein abundance can be a simple LOF or a folding-deficient variant that burdens the cellular proteostasis network [67]. To differentiate, you can perform a pharmacological chaperone assay. If a small-molecule stabilizer (correctors) can rescue the protein's expression and function, it strongly suggests the primary defect is folding and stability, a common LOF mechanism [68].
Troubleshooting Guides
Problem: Inconclusive Results from Standard Pathogenicity Predictors
Symptoms: Variants of Uncertain Significance (VUS) in a gene where known pathogenic variants act through both GOF and LOF mechanisms. Standard in silico tools (e.g., SIFT, PolyPhen-2) provide conflicting or low-confidence scores.
| Investigation Step | Methodology & Tools | Interpretation of Results |
|---|---|---|
| 1. Protein Structure Analysis | Calculate predicted ΔΔG using FoldX [66] or ESM-IF [69]. Calculate the Extent of Disease Clustering (EDC) metric [65]. | LOF-like: High |ΔΔG|, variants dispersed. Non-LOF-like: Low |ΔΔG|, variants clustered in 3D space [65] [66]. |
| 2. Calculate an mLOF Score | Use the published mLOF likelihood score method, combining EDC and ΔΔGrank into a single score [65]. | An mLOF score above 0.508 suggests a LOF mechanism. A score below 0.508 suggests a non-LOF (GOF/DN) mechanism [65]. |
| 3. Check Paralogous Variants | Use multiple sequence alignment to find variants at the same conserved position in paralogous genes [14]. | A pathogenic variant at a conserved site in a paralog provides strong evidence (LR+ ~13.0) for pathogenicity and can inform mechanism [14]. |
Problem: Validating a Suspected Dominant-Negative (DN) Mechanism
Symptoms: A heterozygous missense variant in a gene encoding a homomultimeric protein leads to a severe dominant phenotype, but the variant protein does not appear to have a new or enhanced function.
| Investigation Step | Methodology & Tools | Interpretation of Results |
|---|---|---|
| 1. Identify Protein Interfaces | Analyze AF2 structural models to locate protein-protein interaction interfaces [66] [70]. | DN variants are highly enriched at protein interfaces compared to buried residues or solvent-exposed surfaces [66]. |
| 2. Functional Complementation Assay | Co-express wild-type and mutant proteins in a null background (e.g., yeast, mammalian cells) and measure complex activity [66]. | A significant reduction in activity in the co-expression state compared to wild-type alone is indicative of a DN effect, where the mutant "poisons" the complex. |
| 3. Assess Complex Assembly | Use techniques like size-exclusion chromatography or co-immunoprecipitation to examine the formation and composition of the protein complex [66]. | The presence of aberrant complex formations or the incorporation of mutant subunits into otherwise wild-type complexes supports a DN model. |
Problem: Confirming a Gain-of-Function (GOF) Mechanism
Symptoms: A variant is associated with a novel or opposite phenotype compared to LOF variants in the same gene, such as hyperactivation rather than loss.
| Investigation Step | Methodology & Tools | Interpretation of Results |
|---|---|---|
| 1. Define Baseline Activity | Establish a robust assay for the protein's native activity (e.g., kinase activity, ion conductance, transcriptional activation) [70]. | A significant increase in basal activity or altered specificity in the variant protein, independent of protein abundance, suggests a GOF mechanism. |
| 2. Deep Mutational Scanning (DMS) | Perform or consult a DMS study that measures functional activity and abundance separately for many variants [71] [69]. | Variants that show high functional scores but normal abundance scores are strong GOF candidates. This separates function from stability effects. |
| 3. Chemoproteomic Profiling | Integrate chemoproteomic data for residues like cysteine, lysine, and tyrosine [72]. | Pathogenic variants are enriched near chemoproteomic-detected amino acids (CpDAAs), which are often functionally important sites. Altered reactivity can indicate GOF. |
Quantitative Data on Molecular Mechanisms
Table 1: Prevalence of Molecular Disease Mechanisms Across Genetic Phenotypes Data derived from a large-scale analysis of 2,837 phenotypes in 1,979 Mendelian disease genes [65].
| Mechanism Category | Prevalence in Dominant Genes | Key Structural Features | Common Therapeutic Strategies |
|---|---|---|---|
| Loss-of-Function (LOF) | ~52% of phenotypes | Highly destabilizing (high |ΔΔG|), widespread in structure [65] [66] | Gene replacement, pharmacological chaperones [65] [68] |
| Gain-of-Function (GOF) | Part of the combined 48% | Mild structural impact (low |ΔΔG|), clustered in functional sites [65] [66] | Small-molecule inhibitors, allele-specific silencing [65] |
| Dominant-Negative (DN) | Part of the combined 48% | Mild structural impact, highly enriched at protein interfaces [66] | Suppression of mutant allele, small-molecule disruptors [65] |
Table 2: Performance of Computational Methods on Different Mechanisms A summary of the ability of different computational approaches to identify pathogenic variants by their mechanism [65] [66] [70].
| Prediction Method | Performance on LOF Variants | Performance on GOF/DN Variants | Key Limitation |
|---|---|---|---|
| Standard VEPs (e.g., CADD, SIFT) | Moderate to High | Lower performance | Trained on features associated with LOF and conservation [66] |
| Stability Predictors (e.g., FoldX) | Good (AUC ~0.68) [66] | Poor | Rely on significant destabilization, which GOF/DN variants lack [66] |
| Structure/Clustering (mLOF Score) | Good (Sensitivity 0.72) [65] | Good (Specificity 0.70) [65] | Requires a set of pathogenic variants and a 3D structure [65] |
| Specialized Tools (e.g., LoGoFunc) | High (designed for both) | High (designed for both) | Requires specific training and feature sets [70] |
Experimental Protocols
Protocol 1: Differentiating LOF Mechanisms Using Abundance-Function Assays
This protocol is based on the FunC-ESMs computational framework and multiplexed experimental approaches to distinguish variants that cause LOF through instability from those that directly disrupt function [69].
1. Predict Variant Effects: * Input: Protein sequence and an AlphaFold2-predicted or experimental structure. * Step A - Predict Deleteriousness: Use the ESM-1b language model to generate a score predicting whether a variant is deleterious (loss-of-function). * Step B - Predict Stability Effect: For variants deemed deleterious, use the ESM-IF model to predict the change in folding free energy (ΔΔG). * Classification: Variants are classified as: * WT-like: Not deleterious. * Total-loss: Deleterious and destabilizing. These cause LOF by reducing protein abundance/stability. * Stable-but-inactive: Deleterious but not destabilizing. These cause LOF by directly disrupting functional sites (e.g., active sites, interaction interfaces) [69].
2. Experimental Validation (Multiplexed Assay of Variant Effects - MAVE): * Construct a variant library containing all possible missense changes in your gene of interest. * Perform separate, parallel selections to measure: * Protein Abundance: Using FACS with an epitope tag, without permeabilization, to measure surface expression for membrane proteins, or similar assays for intracellular proteins [68] [69]. * Protein Function: Using a growth-based selection, reporter assay, or other functional readout specific to the protein's role [69]. * Integrate Data: Plot functional scores against abundance scores. Variants that cluster along the diagonal are likely stability-dependent (Total-loss). Variants that show low function but high abundance are likely direct functional disruptors (Stable-but-inactive) [69].
The workflow for this experimental design is outlined below.
Protocol 2: Rescuing Destabilized LOF Variants with Pharmacological Chaperones
This protocol is based on research demonstrating that small molecule stabilizers can rescue the surface expression of nearly all missense variants in a GPCR that cause disease through loss of abundance [68].
1. Identify Candidate Variants: * Use the mLOF score or abundance-function MAVE data to identify variants that are poorly expressed, suggesting a primary defect in protein folding, stability, or trafficking [65] [68].
2. Select a Pharmacological Chaperone (PC): * Choose a high-affinity ligand or small molecule known to bind the native folded state of your target protein. This does not need to be a clinical drug; research compounds can be used (e.g., tolvaptan for the Vasopressin 2 Receptor) [68].
3. Treatment and Measurement: * Transfert cells with plasmids expressing the wild-type or mutant variants. * Treat the cells with the selected PC or a vehicle control (e.g., DMSO) for a period sufficient to allow for protein synthesis and trafficking (e.g., 16-24 hours). * Quantify Functional Protein: * For membrane proteins (e.g., GPCRs, ion channels): Use FACS-based surface expression staining (non-permeabilized) with an epitope tag antibody [68]. * For intracellular proteins: Measure total protein abundance via western blot or a functional enzymatic/activity assay. * Dose-Response Analysis: For responsive variants, perform a dose-response curve with the PC to determine EC₅₀.
4. Interpret Results: * Rescued Variants: Show a significant, dose-dependent increase in protein abundance/function upon PC treatment. This confirms that LOF is due to destabilization, and the protein is functionally competent if it can fold. * Non-rescued Variants: Show no improvement. This suggests the variant may cause LOF through a direct, irreparable functional defect or may disrupt the PC binding site itself [68].
The Scientist's Toolkit
Table 3: Key Research Reagent Solutions for GOF/LOF Studies
| Research Reagent | Function & Application in GOF/LOF Studies |
|---|---|
| AlphaFold2 (AF2) Models | Provides high-quality predicted protein structures for genes without experimental structures; essential for in silico stability (ΔΔG) calculations and mapping variant clusters in 3D [69] [70]. |
| Saturation Mutagenesis Libraries | Plasmid libraries containing all possible single amino acid changes in a gene; the foundation for Deep Mutational Scanning (DMS) experiments to measure variant effects on abundance and function at scale [68] [69]. |
| Pharmacological Chaperones (PCs) | Small molecules that bind and stabilize specific target proteins; used to experimentally test if a variant's pathogenicity is due to protein destabilization and to explore therapeutic strategies [68]. |
| ESM-1b & ESM-IF Models | Pre-trained machine learning models for zero-shot prediction of variant deleteriousness (ESM-1b) and protein stability changes (ESM-IF); enable fast, proteome-wide computational classification of variant mechanisms [69]. |
| Paralogous Gene Alignments | Curated multiple sequence alignments for gene families; used to transfer knowledge of variant pathogenicity and mechanism from well-characterized genes to less-studied paralogs [14]. |
Analytical Workflow for Mechanism Determination
The following diagram provides a consolidated, step-by-step workflow for determining the molecular mechanism of a missense variant, integrating the FAQs and protocols detailed above.
Integrating Chemoproteomic Data for Functional Site Delineation
Frequently Asked Questions (FAQs)
FAQ: How can chemoproteomic data help in classifying variants of uncertain significance (VUS)?
Chemoproteomic-detected amino acids (CpDAAs) are enriched at and around sites with known pathogenic missense variants. By analyzing regions at or around CpDAAs in proteins like fumarate hydratase (FH), researchers have found an enrichment of both VUSs and pathogenic variants. This enrichment provides functional evidence that can help reclassify a VUS as likely pathogenic. For example, altered FH oligomerization states have been experimentally validated for variants near CpDAAs, providing a functional consequence that supports pathogenicity [73].
FAQ: Which amino acids are typically profiled in chemoproteomic studies and why?
Chemoproteomic studies often focus on privileged amino acids with reactive side chains, most commonly cysteine, lysine, and tyrosine. These residues are targeted because their chemical reactivity allows for covalent binding with activity-based probes. This reactivity enables the mapping of functional sites on proteins, which are often critical for catalytic activity or molecular interactions and are frequently disrupted by pathogenic mutations [73].
FAQ: What is the evidence that chemoproteomic-detected sites are biologically important?
Genes where amino acids are detected via chemoproteomics are significantly enriched for monogenic-disease phenotypes. This indicates that the reactive sites identified through chemoproteomics are functionally important in human health and disease. The enrichment occurs at both one-dimensional protein sequences and three-dimensional protein structures, suggesting these sites represent fundamental functional domains [73].
FAQ: How does chemoproteomics complement genomic-based prediction tools for variant classification?
While genomic tools provide genome-wide assessments of deleteriousness, chemoproteomics adds a layer of functional protein-based measurement. Genomic predictors primarily use sequence conservation and structural features, whereas chemoproteomics directly measures amino acid reactivity and functional site engagement. This integration is particularly valuable for providing experimental evidence for variant impact, especially for VUS reclassification [73] [8].
FAQ: Can chemoproteomic data be integrated with other biological data types for enhanced variant interpretation?
Yes, advanced integration approaches are emerging. Some methods combine chemoproteomic data with heterogeneous biomedical knowledge graphs containing information about proteins, diseases, drugs, phenotypes, pathways, molecular functions, and biological processes. This multi-modal integration allows for more comprehensive variant interpretation by contextualizing chemoproteomic findings within broader biological systems [32].
Troubleshooting Experimental Challenges
Issue: Low Coverage of Target Amino Acids in Chemoproteomic Profiling
Problem: Key functional residues are not detected in chemoproteomic experiments, creating gaps in functional site maps.
Solution: Implement multi-warhead profiling strategies.
- Step 1: Utilize complementary probe chemistries that target different amino acid types or different reactive properties.
- Step 2: Employ competitive ABPP with broad-spectrum vs. selective probes to identify functional residues.
- Step 3: Optimize reaction conditions (pH, time, temperature) to maximize coverage while maintaining specificity.
- Validation: Confirm detected sites through orthogonal methods like mutagenesis or functional assays [74].
Issue: High Background Signal in Enrichment Experiments
Problem: Non-specific binding or background interference complicates the identification of true functional sites.
Solution: Implement rigorous control experiments and computational filtering.
- Step 1: Include control samples with non-reactive probes or pre-blocked with irreversible inhibitors.
- Step 2: Use quantitative proteomics with isobaric tags (TMT, iTRAQ) to distinguish specific from non-specific interactions.
- Step 3: Apply statistical thresholds based on fold-change and abundance rather than presence/absence.
- Step 4: Integrate with structural data to prioritize biologically plausible sites [73] [74].
Issue: Translating Chemoproteomic Hits to Functional Validation
Problem: Determining which detected sites are functionally relevant for variant classification.
Solution: Prioritize sites using integrated genomic and structural evidence.
- Step 1: Overlap CpDAAs with known pathogenic variant clusters and evolutionary conserved regions.
- Step 2: Prioritize sites where VUSs are statistically enriched around CpDAAs.
- Step 3: Validate functional impact through directed mutagenesis and biochemical assays (e.g., oligomerization state, catalytic activity).
- Step 4: Assess whether identified sites correspond to known functional domains or allosteric regulatory sites [73].
Table 1: Performance Metrics for Integrated Variant Prediction Methods
| Method | Accuracy | Sensitivity | Specificity | Application Scope |
|---|---|---|---|---|
| Disease-Specific Knowledge Graph + GCN [32] | 85.6% | 90.5% | 89.8% | Disease-specific variant pathogenicity |
| Paralogous Variant Conservation (para-SAME) [14] | LR+ = 13.0 | - | - | Cross-paralog pathogenicity evidence |
| Paralogous Variant Conservation (para-DIFF) [14] | LR+ = 6.0 | - | - | Cross-paralog pathogenicity evidence |
| MissenseNet with Structural Features [8] | Superior to conventional methods | - | - | General missense pathogenicity |
Table 2: Chemoproteomic Data Impact on Variant Interpretation
| Metric | Gene-Specific Evidence Only | With Paralogous Integration | Fold Increase |
|---|---|---|---|
| Classifiable Amino Acid Residues [14] | 22,071 | 83,741 | 3.8x |
| Genes with Monogenic Disease Enrichment [73] | Significant enrichment in CpDAA genes | - | - |
| Pathogenic Variant Enrichment at CpDAAs [73] | Significant 3D enrichment around detected sites | - | - |
Experimental Protocols
Protocol 1: Activity-Based Protein Profiling for Functional Site Identification
Principle: Activity-based protein profiling uses chemical probes with three components: (1) reactive warhead, (2) spacer linker, and (3) reporter or bio-orthogonal handle to label functional sites in complex proteomes [74].
Step-by-Step Workflow:
- Probe Design: Select appropriate warhead for target enzyme class (e.g., fluorophosphonates for serine hydrolases).
- Labeling Reaction: Incubate proteome with probe under physiological conditions.
- Visualization/Enrichment: Use fluorescent tags for SDS-PAGE detection or biotin tags for streptavidin enrichment.
- Mass Spectrometry Analysis: Digest enriched proteins, analyze by LC-MS/MS, and identify labeled sites via database searching.
- Data Integration: Map detected sites to protein structures and variant databases [74].
Critical Steps:
- Optimize probe concentration and labeling time to minimize non-specific binding.
- Include control with pre-incubation with broad-spectrum inhibitor.
- Use bio-orthogonal handles (azide/alkyne) for minimal perturbation.
Protocol 2: Integrating Chemoproteomic Data with Variant Pathogenicity Prediction
Principle: Leverage chemoproteomic-detected functional sites to prioritize missense variants based on spatial proximity and functional constraint.
Implementation:
- Data Collection: Compile CpDAAs from published chemoproteomic datasets for cysteine, lysine, and tyrosine.
- Variant Mapping: Map missense variants from ClinVar and gnomAD to protein positions.
- Enrichment Analysis: Calculate statistical enrichment of pathogenic variants at and around CpDAAs (0-10Å in 3D space).
- VUS Prioritization: Score VUSs based on proximity to CpDAAs and co-localization with pathogenic variant clusters.
- Experimental Validation: Select high-priority VUSs for functional validation (e.g., oligomerization assays, enzyme activity) [73].
Visual Workflows and Pathways
Chemoproteomic-Variant Integration Workflow
Workflow for Integrating Chemoproteomic Data with Variant Interpretation
Paralogous Variant Evidence Integration
Paralogous Variant Evidence Integration Logic
Research Reagent Solutions
Table 3: Essential Research Reagents for Chemoproteomic-Variant Integration Studies
| Reagent/Category | Specific Examples | Function/Application |
|---|---|---|
| Activity-Based Probes | Fluorophosphonate probes, HA-tagged probes, Biotinylated probes | Covalently label active sites of enzyme families for functional profiling |
| Bio-orthogonal Handles | Azide/Alkyne tags, Tetrazine/trans-cyclooctene | Enable click chemistry conjugation for visualization and enrichment |
| Mass Spectrometry Reagents | TMT/iTRAQ tags, Trypsin/Lys-C proteases, Stable isotope labels | Enable quantitative proteomic analysis and site identification |
| Variant Databases | ClinVar, gnomAD, HGMD | Provide pathogenic and population variant data for correlation analysis |
| Structural Prediction Tools | AlphaFold2, FEATURE framework | Generate 3D structural contexts for variant impact assessment |
| Validation Assay Reagents | Antibodies for immunoprecipitation, Activity assay substrates | Functionally validate impact of prioritized variants |
Addressing Data Sparsity with Transfer Learning and Active Learning
In the field of human genetics, classifying the pathogenicity of missense variants—single nucleotide changes that result in an amino acid substitution—is a fundamental challenge for disease gene discovery, clinical diagnostics, and therapeutic development. A central obstacle in this domain is data sparsity: despite millions of possible missense variants in the human genome, only about 2% have been definitively classified as pathogenic or benign through experimental or clinical evidence [8]. This severe imbalance and scarcity of high-quality annotated data significantly hinder the development of robust machine learning (ML) models, which traditionally require large, well-labeled datasets for training.
Transfer Learning (TL) and Active Learning (AL) have emerged as powerful computational strategies to overcome these data limitations. Transfer learning allows knowledge gained from data-rich proteins or related tasks to be applied to proteins with sparse annotation, while active learning intelligently selects the most informative variants for experimental validation, optimizing resource allocation. This technical support center provides troubleshooting guides and FAQs to help researchers effectively implement these approaches within their missense variant classification pipelines.
Core Concepts & Terminology
Foundational Knowledge
- Missense Variant: A single nucleotide change in the coding region of a gene that results in the substitution of one amino acid for another in the corresponding protein.
- Pathogenicity: The potential of a genetic variant to cause or contribute to disease.
- Data Sparsity: The phenomenon where the number of variants with known pathological effects is extremely small compared to the vast space of all possible variants.
- Transfer Learning (TL): A machine learning technique where a model developed for one task is reused as the starting point for a model on a second, related task. In this context, it often involves training on one set of proteins and applying the knowledge to another.
- Active Learning (AL): A machine learning paradigm where the algorithm iteratively queries an "oracle" (e.g., an experimental assay) to label the data points from which it will learn the most, thereby reducing the number of experiments required to achieve high performance.
- Cross-Protein Transfer Learning: A specific TL approach where a model is trained on functional data from a limited number of proteins and then applied to make predictions across the entire human proteome [75].
Research Reagent Solutions
The table below details key computational tools and data resources essential for implementing TL and AL in missense variant research.
Table 1: Essential Research Reagents & Computational Tools
| Item Name | Type | Primary Function/Benefit |
|---|---|---|
| Deep Mutational Scanning (DMS) Data | Dataset | Provides high-throughput functional measurements for thousands of variants in a single protein, serving as a rich source for pre-training TL models [75]. |
| AlphaFold2 | Tool/Feature | Provides highly accurate predicted protein structures, enabling the calculation of structural features (e.g., residue interactions, solvent accessibility) that boost prediction accuracy for variants in proteins without experimental structures [75] [8]. |
| CPT (Cross-Protein Transfer) Framework | Model/Protocol | A robust TL framework that integrates DMS data, protein sequence models (EVE, ESM-1v), and AlphaFold2 structural features to achieve state-of-the-art pathogenicity prediction on unseen proteins [75]. |
| PreMode | Model/Tool | Uses deep graph representation learning on protein sequence and structure to predict the specific mode-of-action (e.g., gain-of-function vs. loss-of-function) of missense variants, which is critical for therapeutic strategies [76]. |
| Paralogous Meta-Domains | Data/Concept | Structurally equivalent positions across related protein domains from different genes; can be used to aggregate variant data and augment evidence for classifying novel missense variants, directly addressing data sparsity [77]. |
Troubleshooting Guides & FAQs
FAQ 1: How can I build an accurate predictor for a protein with no clinical variant data?
Answer: The recommended solution is to employ a Cross-Protein Transfer Learning framework. This approach leverages functional data from well-studied proteins to create a model that generalizes to novel proteins.
Experimental Protocol: Implementing a CPT Framework
Feature Engineering: Compile a diverse set of predictive features for your variants of interest. Essential features include:
- Variant Effect Predictors: Pre-computed scores from zero-shot models like EVE and ESM-1v, which are trained on general protein sequence families [75].
- Evolutionary Conservation: Features derived from multiple sequence alignments (MSAs) of closely related species (e.g., 100 vertebrates), which provide a strong, complementary signal [75].
- Structural Features: Use AlphaFold2 to generate a protein structure, then compute features such as:
Model Training & Selection:
- Training Data: Train a model (e.g., a deep neural network) on a curated set of DMS data from a few proteins (e.g., CALM1, MTHFR, SUMO1). This data is exhaustive and less biased than clinical collections [75].
- Feature Selection: Use cross-validation on the DMS training set to select the most informative and non-redundant features for the final model [75].
Evaluation: Benchmark the model's performance on a fully independent set of ClinVar variants in genes that were not part of the training process. Key metrics should focus on the high-sensitivity regime, which is crucial for clinical applications [75].
Table 2: Performance Comparison of CPT-1 vs. Other Methods on Independent ClinVar Data
| Method | Training Data Type | AUROC (ClinVar) | Specificity at 95% Sensitivity |
|---|---|---|---|
| CPT-1 | DMS (5 proteins) | ~0.96 | 68% |
| EVE | Protein MSAs (unsupervised) | ~0.92 | 55% |
| ESM-1v | Protein MSAs (unsupervised) | ~0.89 | 27% |
| REVEL | Clinical variants (supervised) | Varies (held-out genes) | Lower than CPT-1 |
Note: AUROC = Area Under the Receiver Operating Characteristic Curve. Data adapted from [75].
FAQ 2: My model's performance is biased toward the majority class (e.g., benign variants). How can I improve detection of rare pathogenic variants?
Answer: This is a classic class imbalance problem. Mitigation strategies can be applied at the data and algorithm levels.
Technical Guide: Addressing Class Imbalance
Data-Level Solutions:
- Synthetic Oversampling: Apply techniques like SMOTE (Synthetic Minority Over-sampling Technique) to generate synthetic examples of the pathogenic (minority) class in the feature space. This helps prevent the model from being overwhelmed by the benign class [78] [79].
- Data Augmentation with Physical Models: Use biophysical models or simulation data to generate additional, realistic pathogenic variant examples, enriching the minority class [78].
Algorithm-Level Solutions:
- Cost-Sensitive Learning: Modify the learning algorithm to assign a higher misclassification cost to the minority (pathogenic) class. This forces the model to pay more attention to correctly predicting these rare cases [79].
- Ensemble Methods: Use ensemble models like Random Forests or XGBoost, which can be combined with sampling techniques like RF-SMOTE to improve robustness against imbalance [78].
Evaluation Metric Correction:
- Stop using accuracy alone. In imbalanced scenarios, accuracy is misleading. Instead, use a suite of metrics:
- Precision-Recall (PR) Curves and Area Under the PR Curve (AUPRC)
- F1-Score: The harmonic mean of precision and recall.
- Matthew's Correlation Coefficient (MCC): A balanced measure for binary classes [79].
- Stop using accuracy alone. In imbalanced scenarios, accuracy is misleading. Instead, use a suite of metrics:
FAQ 3: I have a limited budget for functional assays. Which variants should I prioritize for experimental testing to improve my model most efficiently?
Answer: Implement an Active Learning loop to iteratively select the most "informative" variants for experimental validation.
Experimental Protocol: Active Learning for Variant Prioritization
- Initialization: Start with a small, initial set of variants with known pathogenicity (a "seed" set) to train a preliminary model.
- Iteration:
- Step 1 - Prediction: Use the current model to predict pathogenicity scores for all unlabeled variants in your pool.
- Step 2 - Query Strategy: Select the most informative variants for experimental testing. Common strategies include:
- Uncertainty Sampling: Prioritize variants where the model is most uncertain (e.g., prediction score closest to 0.5).
- Query-by-Committee: Use an ensemble of models and select variants where the models disagree the most.
- Step 3 - Experimentation: Send the top-ranked variants from Step 2 for functional assay (the "oracle").
- Step 4 - Model Update: Retrain your model with the newly labeled variants added to the training set.
- Convergence: Repeat the iteration until the model performance plateaus or the experimental budget is exhausted. This approach has been shown to enable efficient study design for deep mutational scans and fitness optimization [76].
The following diagram illustrates this iterative workflow:
FAQ 4: How can I leverage protein structures from AlphaFold2 to compensate for a lack of variant data?
Answer: Integrating predicted structural features can significantly boost performance, especially for proteins with few known variants, by providing a strong, orthogonal signal.
Technical Guide: Extracting and Using AlphaFold2 Structural Features
- Structure Prediction: Input your protein sequence of interest into a local or cloud-based AlphaFold2 implementation to obtain a predicted 3D structure.
- Feature Calculation: Compute the following features for each residue position and the specific amino acid change:
- Residue Environment: Calculate the solvent accessibility and hemispheric exposure of the wild-type residue.
- Interaction Networks: Within a 6Å radius, identify and count different interaction types: aromatic-aromatic, aromatic-sulfur, hydrogen bonds (backbone-side chain and side chain-side chain), and hydrophobic interactions [8].
- Graph-Theoretic Metrics: Model the protein structure as a graph where residues are nodes and interactions are edges. Calculate:
- Betweenness Centrality: Identifies residues that act as bridges in the network.
- Eigenvector Centrality: Identifies residues that are connected to other well-connected residues.
- Local Structure Quality: Use the per-residue confidence score (pLDDT) from AlphaFold2 to weight the reliability of the structural features [8].
- Model Integration: Concatenate these structural features with your existing evolutionary and sequence-based features (from Step 1 of the CPT protocol) and use them as input to your chosen classifier (e.g., a deep learning model like MissenseNet) [8].
Advanced Strategy: Leveraging Paralogous Domains
How can I find more data for my gene of interest if direct experiments are not feasible?
Answer: Aggregate data across paralogous protein domains. Proteins often share conserved structural domains. Pathogenic or benign variants at structurally equivalent positions in these paralogous domains can provide moderate evidence for classifying a novel variant in your gene of interest [77].
Experimental Protocol:
- Use databases like PFam to identify the protein domain architecture of your target gene.
- Map the specific amino acid position to its structurally equivalent position in all other human proteins containing the same domain (creating a "meta-domain").
- Aggregate all clinically annotated missense variants at these equivalent positions from sources like ClinVar.
- Use this aggregated data as additional features or as a form of transfer learning. This approach has been shown to increase the sensitivity of classifying pathogenic missense variants from 27% to 41% [77].
Benchmarking Predictive Performance and Clinical Translation
Frequently Asked Questions (FAQs)
Q1: Why are Sensitivity and Specificity both critical for evaluating pathogenicity predictors, and what is the trade-off between them?
Sensitivity and Specificity are fundamental because they evaluate a model's performance from two distinct and clinically crucial perspectives. Sensitivity measures the ability to correctly identify pathogenic variants, minimizing false negatives, which is critical as missing a true pathogenic variant could have severe clinical consequences. Specificity measures the ability to correctly identify benign variants, minimizing false positives, which is vital to prevent unnecessary patient anxiety and interventions [80].
The trade-off between them is managed by adjusting the model's classification threshold. No single threshold simultaneously maximizes both metrics. A higher threshold might increase specificity but reduce sensitivity, meaning fewer benign variants are mislabeled, but at the cost of missing more true pathogenic ones. Conversely, a lower threshold might increase sensitivity but reduce specificity [81]. The choice of the optimal threshold depends on the clinical context—for example, in screening for a highly penetrant cancer gene, you might prioritize high sensitivity.
Q2: My model has high accuracy on a balanced dataset, but performance drops severely on real-world, imbalanced data. What is going wrong and how can I fix it?
This is a common pitfall. Accuracy can be a misleading metric when your dataset is imbalanced, meaning one class (e.g., benign variants) significantly outnumbers the other (e.g., pathogenic variants). A model can achieve high accuracy by simply always predicting the majority class, while failing miserably at identifying the minority class of interest [82].
To address this, you should:
- Use metrics robust to class imbalance: The Area Under the Precision-Recall Curve (AUPRC) is often more informative than AUC-ROC for imbalanced datasets, as it focuses on the model's performance on the positive class [80]. The F1-score (the harmonic mean of precision and recall) and the Geometric Mean (G-mean) are also valuable for evaluating the balance of performance on both classes [80].
- Examine the Precision-Recall Curve: This curve will give you a realistic picture of the trade-offs when dealing with the actual class distribution in your data [81].
Q3: What does the AUC-ROC score tell me, and how should I interpret its value when comparing different tools?
The Area Under the Receiver Operating Characteristic Curve (AUC-ROC) provides a single measure of a model's ability to discriminate between two classes across all possible classification thresholds [81] [82].
- AUC = 1.0: Perfect classifier. The model can perfectly separate all positive and negative instances.
- AUC = 0.5: No discriminative power. The model performs no better than random guessing.
- AUC < 0.5: The model performs worse than random guessing.
- AUC between 0.5 and 1.0: The higher the value, the better the model is at ranking a randomly chosen positive instance higher than a randomly chosen negative one [81].
When comparing tools, a model with a higher AUC is generally considered to have better overall discriminatory performance [81]. For example, a study benchmarking 28 predictors found that MetaRNN and ClinPred achieved the highest AUC on rare variants, indicating their superior ranking capability [80].
Q4: How can I determine the optimal classification threshold for my clinical application?
The optimal threshold is not a statistical given; it is a clinical and practical decision based on the relative costs of false positives and false negatives [81].
- Minimize False Negatives: If the cost of missing a pathogenic variant is very high (e.g., in a highly penetrant cancer gene), you should choose a threshold that favors high Sensitivity. This might be a point on the ROC curve closer to (0,1) [81].
- Minimize False Positives: If the cost of a false alarm is high (e.g., leading to invasive procedures), you should choose a threshold that favors high Specificity.
- Balance the Two: If the costs are roughly equivalent, a common approach is to select the threshold that maximizes the Youden's Index (Sensitivity + Specificity - 1) or is closest to the top-left corner of the ROC plot.
Q5: Why do some pathogenicity predictors perform well on some genes but poorly on others?
Performance can be gene-specific due to differences in the underlying biological mechanisms of pathogenesis and the data used to train the models [83]. Many tools are trained on aggregated multi-gene "truth sets," which may not capture gene-specific patterns. For instance, a study found that common predictors showed inferior sensitivity for pathogenic TERT variants and inferior specificity for benign TP53 variants [83]. This highlights the importance of using disease-specific or even gene-specific models where possible, as they can capture relevant biological context and lead to more accurate predictions [84] [32].
Performance Benchmarking Tables
This table summarizes the performance of various tools from recent benchmarking studies, providing a comparative overview. AUC values are highlighted for easy comparison.
| Tool Name | Type / Model | Key Features / Inputs | Reported AUC | Key Strengths / Context |
|---|---|---|---|---|
| ClinPred [85] | Ensemble ML | Incorporates conservation, other predictor scores, and allele frequency [80]. | 0.792 (BRCA) | Top performer in BRCA variant classification [85]. |
| MetaRNN [80] | RNN Ensemble | Integrates multiple annotation scores and allele frequency [80]. | High (Rare Variants) | High predictive power for rare variants [80]. |
| Extra Trees [84] | Ensemble ML (Extra Trees) | Disease-specific training on breast cancer genes; uses conservation, functional annotations [84]. | ~0.999 (Breast Cancer) | Demonstrates superiority of disease-specific modeling [84]. |
| popEVE [33] | Deep Generative Model | Combines evolutionary sequences and human population data for proteome-wide calibration [33]. | State-of-the-Art | Calibrated for comparing variant deleteriousness across different genes [33]. |
| REVEL [83] | Random Forest Ensemble | Integrates scores from multiple individual tools and conservation metrics [83]. | Varied | Widely used ensemble meta-predictor. |
| CADD [83] | Linear Model | Incorporates genomic, evolutionary, and functional annotations; includes splice information [83]. | Varied | Popular genome-wide annotation tool. |
Table 2: Impact of Allele Frequency on Predictor Performance
This table synthesizes findings on how the rarity of a variant influences the performance of prediction methods, based on a large-scale evaluation of 28 methods [80].
| Performance Metric | Trend as Allele Frequency Decreases | Practical Implication for Rare Variant Analysis |
|---|---|---|
| Specificity | Shows a large decline [80]. | Tools are more likely to misclassify rare benign variants as pathogenic (higher false positive rate). |
| Sensitivity | Tends to decline, but less drastically than specificity [80]. | The ability to find true pathogenic variants remains relatively stable but is still impacted. |
| Overall Metrics | Most performance metrics (e.g., Accuracy, F1-score) tend to decline [80]. | Overall tool reliability is lower for very rare variants compared to more common ones. |
| Recommendation | Use tools specifically designed/trained for rare variants, like MetaRNN or ClinPred [80]. | Always check the design and intended use of a prediction tool for your specific variant frequency range. |
Experimental Protocols
Protocol 1: Benchmarking a Novel Predictor Against Existing Tools
Objective: To rigorously evaluate the performance of a new pathogenicity prediction model and compare it against established benchmarks.
Materials: The "Scientist's Toolkit" table in Section 4 lists essential resources.
Methodology:
- Curate a Benchmark Dataset: Use a high-quality, recent dataset from ClinVar, filtering for variants with a review status of 'expert panel' or 'multiple submitters' and classifications of 'Pathogenic'/'Likely Pathogenic' or 'Benign'/'Likely Benign'. Exclude variants used in the training of existing tools to avoid bias [80].
- Annotate with Prediction Scores: Run all variants in the benchmark set through your novel predictor and a selection of established tools (e.g., those listed in Table 1).
- Calculate Performance Metrics: For each tool, calculate the following metrics using the known labels:
- Sensitivity and Specificity: Calculate at the tool's recommended default threshold [80].
- AUC-ROC: Calculate to evaluate overall ranking performance across all thresholds [80].
- Precision, F1-score, MCC (Matthews Correlation Coefficient): These provide a more comprehensive view, especially for imbalanced datasets [80].
- Statistical Comparison: Use statistical tests (e.g., DeLong's test for AUC comparisons) to determine if performance differences between your model and the best existing tools are statistically significant.
Protocol 2: Determining a Gene-Specific Classification Threshold
Objective: To establish an optimal classification threshold for a specific gene where default thresholds are suboptimal [83].
Materials: A curated, gene-specific dataset with confirmed pathogenic and benign variants.
Methodology:
- Data Collection: Assemble a gene-specific "truth set" of variants with definitive pathogenic/benign classifications from clinical and functional evidence [83].
- Generate Scores: Obtain the prediction scores for your chosen tool for every variant in the truth set.
- Plot ROC and Precision-Recall Curves: Generate these curves based on the truth set labels and the prediction scores.
- Identify Optimal Threshold: Choose a threshold based on clinical needs:
- For high sensitivity, select a threshold corresponding to a point on the ROC curve with high True Positive Rate.
- For high specificity, select a threshold with a low False Positive Rate.
- For a balanced approach, maximize the Youden's Index or select the threshold that gives the best balance of precision and recall on the PR curve.
- Validate: If possible, validate the chosen threshold on a separate, held-out validation dataset.
The Scientist's Toolkit
Research Reagent Solutions
| Item Name | Function / Application | Example Use in Research |
|---|---|---|
| ClinVar Database | Public archive of reports on the relationships between human variants and phenotypes, with supporting evidence [80]. | Serves as the primary source for benchmarking "truth sets" of pathogenic and benign variants [80]. |
| dbNSFP Database | A comprehensive database compiling pre-computed pathogenicity prediction scores from dozens of tools [80]. | Allows for efficient large-scale annotation of variant datasets and benchmarking of multiple predictors without running each tool individually [80]. |
| Knowledge Graphs | Heterogeneous networks integrating multiple biological entities (genes, diseases, drugs, pathways, phenotypes) [32]. | Provides rich, interconnected biological context for training disease-specific variant pathogenicity models using graph neural networks [32]. |
| Evolutionary Scale Modeling (ESM) | Protein language models that learn from millions of natural protein sequences to predict fitness effects [32] [33]. | Used to generate embeddings of variant effects directly from sequence, capturing structural and functional constraints without manual feature engineering [32]. |
| gnomAD / ExAC | Public catalogues of human genetic variation from large-scale sequencing projects [80]. | Provides allele frequency data crucial for filtering common polymorphisms and for use as a feature in training predictors [80]. |
Conceptual Diagrams
ROC Curve Decision Guide
Model Evaluation Workflow
Comparative Analysis of Traditional Tools vs. Deep Learning Approaches
## FAQs: Choosing and Using Pathogenicity Prediction Tools
Q1: What is the key practical limitation of newer deep learning tools like AlphaMissense that I should be aware of?
A1: While tools like AlphaMissense represent significant advances, a key limitation is their reduced sensitivity in predicting pathogenic variants within intrinsically disordered regions (IDRs) of proteins. These are regions that lack a well-defined 3D structure. One study found that the sensitivity of AlphaMissense and other state-of-the-art predictors is consistently lower in these disordered regions compared to ordered regions [86]. This is crucial because IDRs constitute about 30% of the human proteome, and an estimated 10-20% of disease-causing mutations occur within them [86].
Q2: My research focuses on a specific disease, like breast cancer. Are general genome-wide predictors sufficient?
A2: Evidence suggests that disease-specific models can significantly outperform general genome-wide predictors. For example, one study developed an Extra Trees machine learning model specifically for breast cancer-related missense variants. This model achieved an accuracy of 99.1% on an independent ClinGen dataset, substantially outperforming general tools like REVEL (75.1% accuracy) and ClinPred (75.6% accuracy) [84] [87]. Disease-specific models capture biological context and variant features that broader models often overlook.
Q3: Beyond simple "pathogenic vs. benign" classification, can new tools predict how a variant affects protein function?
A3: Yes, this is a key area of innovation. Newer methods are being developed to predict a variant's mode-of-action (MoA), such as gain-of-function (GoF) or loss-of-function (LoF). For instance, PreMode is a deep learning tool designed specifically for gene-specific MoA prediction [88]. This is critical because GoF and LoF variants in the same gene can lead to distinct clinical conditions and require different treatments [88].
Q4: How does the performance of a deep learning tool like AlphaMissense compare to established tools in a real-world clinical cohort?
A4: Performance in real-world cohorts can be more modest than in initial benchmarks. An evaluation of AlphaMissense on a rare disease cohort of 7,454 individuals found that for expertly curated pathogenic variants, its precision was 32.9% and its recall was 57.6% at the recommended threshold [27]. This indicates that while it can find more than half of the true pathogenic variants, a high proportion of its "likely pathogenic" predictions were incorrect in this specific clinical context.
Q5: How can I validate a computational prediction in the lab?
A5: A robust validation workflow involves several steps, from in silico analysis to functional assays. Key experimental approaches include:
- Cell-based Assays: For example, testing the impact of PSEN1, PSEN2, and APP gene variants on Aβ40 and Aβ42 peptide levels in mouse neuroblastoma cells [89].
- Deep Mutational Scans (DMS): Systematically measuring the functional effects of thousands of variants in parallel [88].
- In Vivo Models: Using model organisms, such as humanized C. elegans (worm) models, to assess the phenotypic impact of a variant [90].
## Troubleshooting Guides
Problem: Inconsistent or conflicting predictions between tools.
- Cause: Different tools are trained on different datasets and use different underlying features and algorithms.
- Solution:
- Do not rely on a single predictor. Use a consensus approach.
- Consult the evidence behind the prediction. Tools that incorporate protein structure (e.g., AlphaMissense, PreMode) or functional data may be more reliable for your specific case.
- Prioritize disease-specific models if they are available for your gene or disease of interest [84].
- If the variant is in an intrinsically disordered region, treat all computational predictions with caution and seek additional functional or clinical evidence [86].
Problem: Needing to predict the molecular mechanism of a variant, not just pathogenicity.
- Cause: Standard pathogenicity predictors are designed for binary classification and do not distinguish between GoF and LoF mechanisms.
- Solution: Employ next-generation tools specifically designed for mode-of-action prediction, such as PreMode [88]. Additionally, examine whether the variant resides in a specific protein domain or structural feature known to be associated with a particular mechanism (e.g., an ion channel pore).
Problem: Needing to increase the reliability of predictions for a critical variant.
- Cause: All computational predictions have an error rate and should be considered as one piece of evidence.
- Solution: Implement an integrated computational and experimental workflow. Use consensus among top-performing tools to shortlist variants, and then validate them using targeted functional assays. The diagram below illustrates a robust workflow for variant prioritization and validation.
## Performance Data Comparison
The following tables summarize key performance metrics for various traditional and deep learning tools as reported in recent studies.
Table 1: Performance in Specific Disease Contexts
| Tool | Type | Test Context | Key Performance Metric | Value | Citation |
|---|---|---|---|---|---|
| Extra Trees (Disease-Specific) | Machine Learning | Breast Cancer Genes (Independent Test) | Accuracy | 99.1% | [84] [87] |
| AlphaMissense | Deep Learning | Rare Disease Cohort (Real-World) | Precision / Recall | 32.9% / 57.6% | [27] |
| Deep Neural Network (DNN) | Deep Learning | PMM2 Gene (with MD features) | Average ROC-AUC | 0.90 | [90] |
| MVP | Deep Learning | Constrained Genes (Cancer Hotspots) | AUC | 0.91 | [91] |
Table 2: Performance in Intrinsically Disordered vs. Ordered Regions
| Tool | Type | Performance in Ordered Regions | Performance in Disordered Regions | Key Finding | Citation |
|---|---|---|---|---|---|
| AlphaMissense | Deep Learning | Higher Sensitivity | Lower Sensitivity | Largest sensitivity gap between ordered and disordered regions | [86] |
| VARITY | Machine Learning | Higher Sensitivity | Lower Sensitivity | Consistently reduced sensitivity in IDRs | [86] |
| ESM1b | Deep Learning | Higher Sensitivity | Lower Sensitivity | Reduced sensitivity in IDRs | [86] |
## Experimental Protocols
Protocol 1: Benchmarking a New Predictor Against Functional Assay Data
This protocol is adapted from studies that validated computational predictions using laboratory-measured biomarkers [89].
- Variant Selection: Curate a set of missense variants (e.g., Variants of Uncertain Significance - VUS) for your gene(s) of interest from clinical databases or sequencing studies.
- Computational Prediction: Run the variants through the computational tools you wish to benchmark (e.g., AlphaMissense, CADD, REVEL).
- Functional Assay: Perform a cell-based assay to measure the molecular function impacted by the variants.
- Example: For genes like PSEN1, PSEN2, and APP, transfect variant constructs into a suitable cell line (e.g., neuroblastoma N2A cells with endogenous genes knocked out) and measure the resulting Aβ42/Aβ40 ratio via ELISA [89].
- Statistical Correlation: Calculate correlation coefficients (e.g., Pearson's) between the computational pathogenicity scores and the quantitative results from the functional assay.
- Performance Analysis: Perform Receiver Operating Characteristic (ROC) analysis if established pathogenic/benign variants are included, using the functional data as the ground truth.
Protocol 2: Integrating Molecular Dynamics for Enhanced Prediction
This protocol outlines the workflow used in the "Dynamicasome" project, which combined molecular dynamics (MD) simulations with AI for high-accuracy prediction [90].
- Structure Modeling: Generate a 3D structural model for the wild-type protein and for each missense variant, using an experimental structure or a high-confidence AlphaFold2 model.
- Molecular Dynamics Simulation (MDS): For each model, run an MD simulation (e.g., 10 ns) in a simulated physiological environment to observe the dynamic structural consequences of the mutation.
- Feature Extraction: From each MDS trajectory, extract quantitative biophysical features, including:
- Root Mean Square Deviation (RMSD)
- Solvent Accessible Surface Area (SASA)
- Radius of Gyration (Rg)
- Number of Hydrogen Bonds
- Stability Free Energy
- Secondary Structure Elements
- Model Training and Prediction: Train a machine learning model (e.g., Random Forest, Deep Neural Network) using the extracted MD features to predict pathogenicity. This model can then be used to classify VUS.
## Workflow and Pathway Visualizations
Variant Pathogenicity Prediction Workflow
Variant Validation Workflow
## The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Computational and Experimental Resources
| Item / Resource | Type | Primary Function | Key Consideration |
|---|---|---|---|
| AlphaMissense | Computational Tool | Predicts pathogenic potential of missense variants using AlphaFold2 structure and population data. | Lower sensitivity in intrinsically disordered regions [27] [86]. |
| PreMode | Computational Tool | Predicts mode-of-action (GoF/LoF) of missense variants for specific genes. | Crucial for understanding functional impact beyond simple pathogenicity [88]. |
| Molecular Dynamics (MD) Simulation Software | Computational Method | Models atomic-level movement of protein variants to extract stability and dynamics features. | Computationally intensive; provides features that boost prediction accuracy (e.g., RMSD) [90]. |
| ClinVar / HGMD | Database | Curated public archives of human genetic variants and their relationships to phenotype. | Serves as a source of benchmark data; be aware of potential false positives in training data [27] [91]. |
| Cell Line with Gene Knockout (e.g., N2A Psen1/2 KO) | Biological Reagent | Provides a null-background for functional assays of specific genes (e.g., PSEN1, PSEN2). | Essential for controlled measurement of variant impact without interference from endogenous protein [89]. |
| Deep Mutational Scan (DMS) | Experimental Method | High-throughput functional profiling of thousands of protein variants in parallel. | Generates large-scale datasets for training and validating computational models [88]. |
Frequently Asked Questions: Technical Support for Variant Scientists
FAQ 1: What are the primary sources of bias when using public databases like ClinVar to benchmark my new functional assay, and how can I mitigate them?
Benchmarking against public databases is common but introduces specific risks that can compromise your assay's validation.
- Underlying Issue: Public variant databases, such as ClinVar, can contain misclassified variants and have an uneven distribution of data. Relying on them for benchmarking can build these existing errors and biases into your new assay's performance metrics [41]. A significant problem is the small size of "benign" variant sets in many genes, which is the primary driver for achieving high evidence strength for pathogenicity (PS3) during assay validation [92].
- Troubleshooting Guide:
- Action 1: Systematically Curate Benign Truth Sets. Do not rely solely on existing benign classifications in ClinVar. Instead, apply a systematic framework to concurrently assess all possible missense variants in your gene of interest for (likely) benign classification. This involves using established ACMG/AMP evidence codes, such as population frequency (BA1), in silico evidence, and case-control data, to build a larger, more robust benign truth set [92].
- Action 2: Utilize Multiple, Independent Data Sources. Supplement your ClinVar benchmarking with data from other sources, such as large population biobanks (e.g., UK Biobank) to calculate variant-level odds ratios for disease enrichment [93] or data from Multiplex Assays of Variant Effect (MAVEs) that are independent of clinical classifications [41].
- Action 3: Check for Gene-Specific Discordance. Be aware that some computational tools may systematically misclassify variants in genes with specific mechanisms, such as gain-of-function. Always check the literature for known issues in your gene of interest [41].
FAQ 2: I've found a significant discrepancy between my functional assay results and the predictions from a state-of-the-art computational tool like AlphaMissense. Which result should I trust?
This is a common point of confusion, as computational and experimental data are both valuable but have different strengths and limitations.
- Underlying Issue: Advanced computational predictors like AlphaMissense, while powerful, have limitations. They can lack interpretability, may not be disease-specific, and can conflate a variant's effect on protein function with its actual relevance to disease [41]. For example, AlphaMissense has been shown to misclassify experimentally confirmed benign variants at a high rate in some genes and may incorrectly label loss-of-function variants in genes where only gain-of-function is pathogenic [41].
- Troubleshooting Guide:
- Action 1: Interrogate the Biological Mechanism. Determine the established disease mechanism for your gene. Is it loss-of-function, gain-of-function, or dominant-negative? A tool that predicts general "damage" may be irrelevant if the disease requires a specific gain-of-function. Trust your assay if it is specifically designed to measure the clinically relevant molecular function [41].
- Action 2: Calibrate Tools with Gene-Specific Data. Computational tools often have general thresholds calibrated on bulk data. Their performance can be improved by using gene-specific pipelines that select and optimize the most informative in silico tools for that particular gene and disease [94].
- Action 3: Prioritize Experimental Evidence. In cases of clear, validated experimental results that contradict a computational prediction, the experimental data should generally carry more weight in a clinical classification framework. The ACMG/AMP guidelines treat strong functional data (PS3) as a key piece of evidence for pathogenicity [92].
FAQ 3: My functional data suggests a variant is damaging, but it is common in population databases. How do I resolve this conflict for a clinical classification?
This conflict between functional and population evidence is a classic challenge in variant interpretation.
- Underlying Issue: A variant's high population frequency is often strong evidence for benignity (ACMG/AMP code BA1). However, your functional assay may be accurately measuring a molecular defect that does not fully correlate with the clinical disease penetrance due to other genetic or environmental modifiers [95] [4].
- Troubleshooting Guide:
- Action 1: Scrutinize Population Grouping. Check if the high frequency is driven by a specific sub-population. A variant that is common in one ancestry group but utterly absent in others might still be pathogenic in the latter.
- Action 2: Investigate Genetic Modifiers. It is possible that the variant requires a specific genetic background to be fully penetrant. The observed high frequency could be due to many carriers having protective genetic modifiers that offset the variant's effect [4]. Consider using polygenic risk scores (PRS) to see if the phenotype is modified by the carrier's background.
- Action 3: Re-evaluate the Clinical Disease Definition. Ensure that the disease phenotype you are associating with the variant is correct. The functional defect might predispose to a subclinical or different condition than the one initially considered.
FAQ 4: What is the best way to submit my functional data to ClinVar to ensure it has the maximum impact on variant classification?
Proper data submission is critical for sharing your findings with the clinical and research communities.
- Underlying Issue: Incomplete or poorly documented submissions can delay the integration of your data into the clinical interpretation process.
- Troubleshooting Guide:
- Action 1: Prepare a Comprehensive Submission. ClinVar requires specific minimum information for a submission [96]:
- Submitter information (organization and contact).
- A valid variant description (HGVS expression or chromosome coordinates).
- The condition/phenotype for which the variant was interpreted.
- The clinical interpretation (e.g., Pathogenic, Uncertain significance).
- Collection method (e.g., clinical testing, research).
- Allele origin (germline or somatic).
- Affected status (was the variant observed in affected or unaffected individuals).
- Action 2: Submit Variants Individually. For the most utility to the community, submit each variant on a separate row in the submission spreadsheet, even if they were observed in a compound heterozygous state. You can note the co-occurrence and mode of inheritance in the submission [97].
- Action 3: Provide Supporting Evidence. Strongly encourage including supporting evidence in a structured or text form. This includes the number of observations, literature citations, and a summary of the functional data that led to your interpretation [96].
- Action 1: Prepare a Comprehensive Submission. ClinVar requires specific minimum information for a submission [96]:
Experimental Protocols & Data Presentation
Table 1: Comparison of Advanced Pathogenicity Prediction Tools
| Tool Name | Underlying Methodology | Key Input Features | Strengths | Documented Limitations |
|---|---|---|---|---|
| AlphaMissense [41] | Unsupervised deep learning (based on AlphaFold2) | Protein sequence, evolutionary conservation, predicted 3D structure | High performance without training on clinical labels; reduces database bias. | Lacks interpretability; not disease-specific; high false-positive rate in some genes (e.g., IRF6, CPA1) [41]. |
| ESM1b [4] | Unsupervised protein language model | Evolutionary-scale sequence data from UniRef | Predicts variant severity on a continuous scale; can distinguish between GOF and LOF mechanisms. | Performance is gene-dependent; may not capture all context-specific effects. |
| MissenseNet [98] | Supervised deep learning (ShuffleNet architecture) | Traditional predictive features + AlphaFold2 structural insights | Integrates structural data adaptively; shows high accuracy in benchmarks. | Relies on quality of structural predictions; model complexity may limit interpretability. |
| Rigid/Adaptive Classifiers (e.g., for MEFV) [94] | Ensemble machine learning (XGBoost, Random Forest) | Multiple in-silico tool scores, local outlier factor analysis | Gene-specific optimization improves accuracy; classifies VUS into an ordinal likelihood scale. | Requires significant gene-specific tuning and a robust training set of known variants. |
Table 2: Calibration of Population Odds Ratios as ACMG/AMP Evidence (PS4)
This table summarizes how evidence strength for the ACMG/AMP PS4 criterion can be calibrated using variant-level odds ratios (ORs) calculated from large biobanks, as demonstrated in one study [93].
| Phenotype / Gene Example | Odds Ratio (OR) Range | Calibrated ACMG/AMP Evidence Strength | Notes / Context |
|---|---|---|---|
| High LDL (LDLR) | OR ≥ 5.0, lower 95% CI ≥ 1 | Strong (PS4) | Aligns with existing gene-specific criteria for Familial Hypercholesterolemia. |
| Various Actionable Disorders | Varies by phenotype and gene | Can reach "Moderate", "Strong", or "Very Strong" | The strength is not uniform and must be calibrated for each gene-phenotype pair. |
| General Framework | Statistical significance and effect size | Supporting to Very Strong | Enables use of biobank data as quantitative evidence for variant classification. |
Protocol 1: Systematic Framework for Constructing a Benign Truth Set
Purpose: To build a robust set of benign missense variants for the validation of multiplex assays of variant effect (MAVEs), which is crucial for applying the ACMG/AMP PS3 evidence code [92].
Methodology:
- Variant Enumeration: Start by considering all possible missense variants in the gene of interest.
- Concurrent ACMG/AMP Assessment: Systematically evaluate each variant using a combination of established evidence codes:
- Population Frequency (BA1): Identify variants that exceed a defined allele frequency threshold in population databases (e.g., gnomAD), which is a stand-alone evidence for benignity.
- In Silico Evidence (BP4): Incorporate multiple computational predictions to support a benign interpretation.
- Case-Control Data (BS4): Utilize data from case-control studies showing no significant enrichment in affected individuals.
- Classification Aggregation: Apply ACMG/AMP combination rules to assign a (likely) benign classification to variants that meet the requisite criteria.
- Truth Set Application: Use the resulting, expanded set of benign variants as the ground truth for validating your MAVE data.
Protocol 2: Leveraging Biobank Data for Population Evidence (PS4) Calibration
Purpose: To extract and calibrate quantitative evidence of pathogenicity from large population cohorts for variant classification [93].
Methodology:
- Cohort and Phenotype Definition: Obtain exome or genome data from a large biobank (e.g., UK Biobank). Define clinical endpoints or endophenotypes for the disorder of interest using electronic health records.
- Variant Filtering: Focus on rare, nonsynonymous variants within the target gene(s).
- Odds Ratio Calculation: For each variant, calculate a variant-level odds ratio (OR) measuring its enrichment in individuals with the disease versus controls.
- Evidence Strength Calibration: Calibrate the ORs and their confidence intervals to the ACMG/AMP PS4 evidence levels (Supporting, Moderate, Strong, Very Strong). This calibration must be performed specifically for each gene and phenotype, as the same OR may correspond to different evidence strengths in different contexts.
- Data Integration: Combine this population evidence with computational and functional data to enable scalable reclassification of VUSs.
The Scientist's Toolkit: Research Reagent Solutions
| Item / Resource | Function in Research | Key Consideration for Use |
|---|---|---|
| ClinVar Database [95] [99] | Public archive of reports of genotype-phenotype relationships. | Critically assess the "review status" of submissions; be aware of conflicting interpretations. |
| gnomAD Database [95] | Public catalog of human genetic variation from large population cohorts. | Used to filter common variants (benign evidence BA1) and assess variant rarity. |
| Multiplex Assays of Variant Effect (MAVEs) [92] [41] | High-throughput experiments that measure the functional impact of thousands of variants simultaneously. | Require rigorous validation against a robust "truth set" of known pathogenic and benign variants. |
| ACMG/AMP Guidelines [95] [92] | Standardized framework for interpreting sequence variants. | Evidence codes (e.g., PS3, PS4, BA1) provide a common language for translating data into classifications. |
| AlphaFold2 Protein Structure Predictions [41] [98] | Provides highly accurate 3D structural models of proteins. | Structural features (e.g., residue exposure, interaction networks) can enhance pathogenicity prediction models. |
Workflow and Relationship Visualizations
Experimental Validation Workflow
Resolving Data Discordance
Statistical Evidence for Paralog-Based and Conservation-Based Methods
Frequently Asked Questions & Troubleshooting Guides
Interpreting Prediction Scores and Method Selection
Q1: How do I interpret the scores from paralog-based prediction tools, and what thresholds should I use for reliability?
Paralog-based prediction tools often use integrative scoring systems. For Paralog Explorer, which is built on the DIOPT framework, the "DIOPT score" represents the number of algorithms (out of 17 total) that support a given paralog prediction. Higher scores indicate greater confidence [100].
| DIOPT Score Range | Confidence Level | Percentage of Pairs (Human) |
|---|---|---|
| ≥6 | High | 36% [100] |
| ≥4 | Moderate | 62% [100] |
| ≥2 | Low | 100% (Baseline) [100] |
Troubleshooting Tip: If your candidate paralog pair has a DIOPT score <4, be cautious in interpreting functional redundancy. Supplement your analysis with additional evidence, such as gene expression correlation data from integrated resources like GTEx or CCLE [100].
Q2: A pathogenic variant in my gene of interest is located at a position conserved in its paralog. How strong is this as evidence for pathogenicity?
Statistical evidence strongly supports using paralog-conserved variants for pathogenicity assessment. Evidence from a 2025 study demonstrates that the presence of a pathogenic variant at the equivalent position in a paralogous gene significantly increases the likelihood that your variant is pathogenic [14].
| Evidence Type | Description | Positive Likelihood Ratio (LR+) |
|---|---|---|
| para-SAME | Pathogenic paralog variant with identical amino acid change. | 13.0 [14] |
| para-DIFF | Pathogenic paralog variant with a different amino acid change. | 6.0 [14] |
Troubleshooting Tip: This "paralogous variant" evidence is most powerful when the genes belong to a family with high sequence similarity and shared functional domains. Always check the multiple sequence alignment to confirm residue conservation [14].
Addressing Technical Challenges and Limitations
Q3: My analysis involves a missense variant that sophisticated tools like AlphaMissense flag as pathogenic, but my functional assays suggest it is benign. What could explain this discrepancy?
This is a recognized limitation. AlphaMissense, while powerful, is a deep learning model that can systematically misclassify variants. Key reasons for discrepancy include [41]:
- Conflating Functional Impact with Pathogenicity: The tool may correctly predict a variant disrupts protein function, but that disruption might not be the disease mechanism. For example, it misclassified loss-of-function variants in the CPA1 gene as pathogenic for pancreatitis, even though the disease is caused by gain-of-function variants [41].
- Lack of Disease Context: The model provides a general pathogenicity score calibrated on bulk data, not a disease-specific prediction. It does not indicate the mode-of-action (e.g., gain vs. loss of function) [41] [101].
Troubleshooting Guide:
- Consult Gene-Specific Literature: Verify the established molecular mechanisms for your gene. Is the disease driven by LoF or GoF?
- Use a Specialized Tool: Employ next-generation predictors like PreMode, which are specifically designed for gene-specific mode-of-action (G/LoF) prediction [101].
- Validate with Functional Assays: Computational predictions are probabilistic. A robust functional assay is often required for definitive classification [41].
Q4: I have identified a pair of paralogs, but I am unsure how to design a functional experiment to test for synthetic lethality. What is a established experimental workflow?
Paralog-based synthetic lethality is a promising therapeutic strategy in cancer, where targeting one paralog (e.g., ARID1B) is lethal to cells that have lost the other (e.g., ARID1A) [102]. A common validation workflow uses genetic perturbation:
Experimental Workflow for Synthetic Lethality
Troubleshooting Tip: Ensure your model system (e.g., cell line) has a genetic background relevant to the disease. For instance, use a cancer cell line known to have a homozygous deletion of your gene of interest for a cleaner result [102].
Featured Experimental Protocols
Protocol 1: Paralog-Based Yeast Complementation Assay for Variant Pathogenicity
This method uses functional complementation in yeast to assess whether a human gene can rescue the loss of its yeast ortholog or paralog. Pathogenicity is inferred if a variant fails to complement [103].
Key Research Reagents:
| Reagent / Resource | Function in the Experiment |
|---|---|
| S. cerevisiae Strain | Engineered yeast strain with a non-lethal, scorable phenotype (e.g., growth defect) due to deletion of a specific yeast gene. |
| Expression Plasmid | Vector for expressing the wild-type human cDNA (positive control), variant human cDNA (test), and empty vector (negative control) in yeast. |
| Selective Medium | Medium that selects for the plasmid and may amplify the phenotypic difference (e.g., minimal medium, medium with a stressor). |
| Human Paralog cDNA | The wild-type and mutant sequences of the human gene being tested. The gene is a paralog of the deleted yeast gene. |
Methodology Overview:
- Strain & Construct Preparation: Clone the wild-type and mutant versions of the human paralog cDNA into the yeast expression plasmid [103].
- Transformation: Introduce the plasmids into the engineered yeast strain lacking the essential yeast gene.
- Complementation Assay: Plate transformed yeast on selective medium and measure growth (e.g., by colony size or optical density) over several days.
- Data Interpretation: Failure of the variant plasmid to rescue the growth defect, compared to the wild-type plasmid, provides functional evidence for pathogenicity [103].
Yeast Complementation Workflow
Protocol 2: Computational Prediction of Variant Mode-of-Action Using PreMode
PreMode is a deep learning model that moves beyond binary pathogenicity prediction to classify variants as gain-of-function (GoF) or loss-of-function (LoF), which is critical for understanding disease mechanisms and selecting treatments [101].
Key Research Reagents (Computational):
| Resource / Feature | Function in the Model |
|---|---|
| Protein Structure | AlphaFold2-predicted or experimental structures provide 3D structural context. |
| Multiple Sequence Alignment (MSA) | Provides evolutionary conservation information. |
| Protein Language Model Embeddings | ESM2 embeddings capture deep semantic information from protein sequences. |
| Graph Neural Network (GNN) | Models the protein as a graph of residues to learn complex structural relationships. |
Methodology Overview:
- Input Feature Generation: The model takes a protein structure and generates node features for each residue, including MSA-derived conservation, secondary structure, and ESM2 embeddings [101].
- Graph Representation Learning: An SE(3)-equivariant graph neural network processes the protein structure graph. This architecture is aware of 3D rotational geometry, improving generalization [101].
- Transfer Learning for Mode-of-Action:
- The model is first pre-trained on a large set of pathogenic/benign variants to learn a general "distance from wild-type" (parameter r).
- It is then fine-tuned on smaller, gene-specific datasets with known GoF/LoF labels to learn the "direction of change" (parameter θ) [101].
- Prediction Output: The final model provides a classification or score indicating the likelihood of a variant being GoF or LoF for a specific gene.
PreMode Prediction Workflow
Conclusion
The integration of AI-driven methodologies with structural biology and multi-omics data is transforming the classification of pathogenic missense variants, moving the field beyond binary pathogenicity predictions toward nuanced understanding of mode-of-action and disease-specific impacts. Key advances include graph neural networks that incorporate biomedical knowledge graphs, AlphaFold2-enabled structural feature extraction, and paralog-based evidence transfer that significantly expands classifiable variant residues. Future directions must focus on translating these computational advances into clinically actionable insights through robust validation, standardization of mode-of-action predictions for therapeutic development, and creating integrated platforms that bridge computational predictions with experimental functional assays. For biomedical researchers and drug developers, these advancements offer powerful new frameworks for target validation, patient stratification, and developing targeted therapies for genetic disorders.
References
- 1. Landmark Study Reveals Magnitude of Uncertain Results ... [https://www.biospace.com/landmark-study-reveals-magnitude-of-uncertain-results-in-clinical-genetic-testing-for-hereditary-disease-points-to-evidence-based-solutions-to-reach-definitive-results]
- 2. Systematic gaps in reporting variants of uncertain ... [https://www.sciencedirect.com/science/article/pii/S1098360025001480]
- 3. Systematic gaps in reporting variants of uncertain ... [https://pubmed.ncbi.nlm.nih.gov/40542645/]
- 4. Investigating the sources of variable impact of pathogenic ... [https://www.nature.com/articles/s41467-025-60339-7]
- 5. “The Biggest Struggle:” Navigating Trust and Uncertainty in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11588501/]
- 6. Advancements in Prenatal Genetic Screening and Testing [https://www.mdpi.com/2075-4418/15/20/2579]
- 7. Genetic Counselors' Practices and Protocols in Variant ... [https://digitalcommons.liu.edu/symposium_postbeyond/2025/posters/22]
- 8. Enhancing Missense Variant Pathogenicity Prediction with ... [https://www.mdpi.com/2218-273X/14/9/1105]
- 9. Increasing pathogenic germline variant diagnosis rates in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12374290/]
- 10. Elucidating Common Structural Features of Human ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4876038/]
- 11. Structure-based network analysis predicts pathogenic ... [https://www.nature.com/articles/s41525-024-00416-w]
- 12. SIGMA leverages protein structural information to predict the ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10831939/]
- 13. Structural biology in variant interpretation: Perspectives and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12120175/]
- 14. Conserved missense variant pathogenicity and correlated ... [https://genomebiology.biomedcentral.com/articles/10.1186/s13059-025-03663-x]
- 15. Top 10 Bioinformatics Tools in 2025: Features, Pros, Cons ... [https://www.cotocus.com/blog/top-10-bioinformatics-tools-in-2025-features-pros-cons-comparison/]
- 16. Top 10 Free Bioinformatics Tools You Must Know [https://bversity.io/blog/top-10-free-bioinformatics-tools-you-must-know]
- 17. Expasy - SIB Swiss Institute of Bioinformatics [https://www.expasy.org/]
- 18. Calibration of additional computational tools expands ... [https://www.sciencedirect.com/science/article/pii/S1098360025000498]
- 19. 20 Free Bioinformatics Tools for Genomic Data Analysis [https://ngscloud.com/20-free-bioinformatics-tools-for-genomic-data-analysis/]
- 20. The role of gene duplication and paralog specialisation in ... [https://www.nature.com/articles/s41467-025-61216-z]
- 21. Standards and Guidelines for the Interpretation of Sequence ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4544753/]
- 22. Pathogenic missense protein variants affect different ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8110273/]
- 23. Predicted mechanistic impacts of human protein missense ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11160786/]
- 24. The genetic architecture of protein stability [https://www.nature.com/articles/s41586-024-07966-0]
- 25. A framework for exhaustively mapping functional missense ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5740498/]
- 26. Functional Testing of Human Disease Missense Variants in ... [https://www.sciencedirect.com/science/article/pii/S2468024925004759]
- 27. Discordance between a deep learning model and clinical ... [https://www.nature.com/articles/s41525-025-00480-w]
- 28. Prediction tools and score range | Franklin Help Center [https://help.genoox.com/en/articles/4341424-prediction-tools-and-score-range]
- 29. LEAP: Using machine learning to support variant ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7317941/]
- 30. The Evaluation of Tools Used to Predict the Impact of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4409520/]
- 31. Variant effect predictor correlation with functional assays is ... [https://genomebiology.biomedcentral.com/articles/10.1186/s13059-025-03575-w]
- 32. Disease-Specific Prediction of Missense Variant ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12562010/]
- 33. Proteome-wide model for human disease genetics [https://www.nature.com/articles/s41588-025-02400-1]
- 34. Accurate identification and mechanistic evaluation of ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12067267/]
- 35. Data Visualizations, Charts, and Graphs - Digital Accessibility [https://accessibility.huit.harvard.edu/data-viz-charts-graphs]
- 36. DNA Language Model and Interpretable Graph Neural ... [https://arxiv.org/html/2410.15367v1]
- 37. Causality-aware graph neural networks for functional ... [https://www.nature.com/articles/s41540-025-00567-1]
- 38. Highly accurate protein structure prediction with AlphaFold [https://www.nature.com/articles/s41586-021-03819-2]
- 39. ESM [https://huggingface.co/docs/transformers/en/model_doc/esm]
- 40. AlphaFold2 Error - Could not find HHsearch database /data ... [https://help.galaxyproject.org/t/alphafold2-error-could-not-find-hhsearch-database-data-pdb70-pdb70/8593/2]
- 41. Making sense of missense: challenges and opportunities in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11683568/]
- 42. Proteins with alternative folds reveal blind spots in ... [https://www.sciencedirect.com/science/article/pii/S0959440X24002008]
- 43. FASTA format [https://en.wikipedia.org/wiki/FASTA_format]
- 44. FASTA format requirements [https://www.ampliseq.com/otherContent/help-content/help_html/GUID-279D6BB2-F70A-4179-BFEB-6E0D44D577F3.html]
- 45. ESM Cambrian: Revealing the mysteries of proteins with ... [https://www.evolutionaryscale.ai/blog/esm-cambrian]
- 46. FASTA Format for Nucleotide Sequences - NCBI - NIH [https://www.ncbi.nlm.nih.gov/genbank/fastaformat]
- 47. Before and after AlphaFold2: An overview of protein structure ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10011655/]
- 48. A knowledge graph approach to predict and interpret disease-causing gene interactions | BMC Bioinformatics | Full Text [https://bmcbioinformatics.biomedcentral.com/articles/10.1186/s12859-023-05451-5]
- 49. Building a knowledge graph to enable precision medicine | Scientific Data [https://www.nature.com/articles/s41597-023-01960-3]
- 50. AIMedGraph: a comprehensive multi-relational knowledge graph for precision medicine - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9976745/]
- 51. Explainable AI for Estimating Pathogenicity of Genetic ... [https://www.mdpi.com/2072-6694/15/4/1118]
- 52. A knowledge graph approach to predict and interpret disease ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10463539/]
- 53. Disease-Specific Prediction of Missense Variant Pathogenicity with DNA Language Models and Graph Neural Networks | MDPI [https://www.mdpi.com/2306-5354/12/10/1098]
- 54. Petagraph: A large-scale unifying knowledge graph ... [https://www.nature.com/articles/s41597-024-04070-w]
- 55. Deciphering the comprehensive knowledgebase ... [https://www.sciencedirect.com/science/article/abs/pii/S0010482524001896]
- 56. E(3)-equivariant graph neural networks for data-efficient and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9068614/]
- 57. Chemistry-intuitive explanation of graph neural networks ... [https://www.nature.com/articles/s41467-023-38192-3]
- 58. Capturing molecular interactions in graph neural networks [https://pubs.rsc.org/en/content/articlelanding/2023/dd/d2dd00045h]
- 59. Kolmogorov–Arnold graph neural networks for molecular ... [https://www.nature.com/articles/s42256-025-01087-7]
- 60. The recommendation of re-classification of variants ... [https://www.nature.com/articles/s10038-024-01263-4]
- 61. VarPPUD: Variant post prioritization developed for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11065012/]
- 62. Artificial intelligence in clinical genetics | European Journal ... [https://www.nature.com/articles/s41431-024-01782-w]
- 63. ClinGen Variant Classification Guidance [https://clinicalgenome.org/tools/clingen-variant-classification-guidance/]
- 64. Artificial intelligence in clinical and genomic diagnostics [https://genomemedicine.biomedcentral.com/articles/10.1186/s13073-019-0689-8]
- 65. Prevalence of loss-of-function, gain-of-function and ... [https://www.nature.com/articles/s41467-025-63234-3]
- 66. Loss-of-function, gain-of-function and dominant-negative ... [https://www.nature.com/articles/s41467-022-31686-6]
- 67. When “loss-of-function” means proteostasis burden [https://www.sciencedirect.com/science/article/pii/S0002929724004440]
- 68. A small molecule stabilizer rescues the surface expression ... [https://www.nature.com/articles/s41594-025-01659-6]
- 69. Decoding molecular mechanisms for loss-of-function ... [https://elifesciences.org/reviewed-preprints/108160]
- 70. Genome-wide prediction of pathogenic gain- and loss-of ... [https://genomemedicine.biomedcentral.com/articles/10.1186/s13073-023-01261-9]
- 71. Decoding missense variants pleiotropy in the immune ... [https://pubmed.ncbi.nlm.nih.gov/41232508/]
- 72. Prioritizing disease-associated missense variants with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12256893/]
- 73. Prioritizing disease-associated missense variants with ... [https://pubmed.ncbi.nlm.nih.gov/40412387/]
- 74. Chemical proteomics for a comprehensive understanding of ... [https://pubs.rsc.org/en/content/articlehtml/2025/cs/d5cs00381d]
- 75. Cross-protein transfer substantially improves disease learning ... variant [https://genomebiology.biomedcentral.com/articles/10.1186/s13059-023-03024-6]
- 76. PreMode predicts mode-of-action of missense variants by ... [https://pubmed.ncbi.nlm.nih.gov/40764308/]
- 77. Evaluating the use of paralogous protein domains to increase data ... [https://pubmed.ncbi.nlm.nih.gov/38087376/]
- 78. A review of machine learning methods for imbalanced data ... [https://pubs.rsc.org/en/content/articlehtml/2025/sc/d5sc00270b]
- 79. A Survey of Methods for Addressing Imbalance Data ... [https://www.mdpi.com/2072-4292/17/3/454]
- 80. Assessing the performance of 28 pathogenicity prediction ... [https://bmcgenomics.biomedcentral.com/articles/10.1186/s12864-025-11787-4]
- 81. Classification: ROC and AUC | Machine Learning [https://developers.google.com/machine-learning/crash-course/classification/roc-and-auc]
- 82. AUC ROC Curve in Machine Learning [https://www.geeksforgeeks.org/machine-learning/auc-roc-curve/]
- 83. The performance of in silico prediction tools for variant ... [https://www.medrxiv.org/content/10.1101/2025.07.29.25331316v1.full-text]
- 84. Precision in prediction: tailoring machine learning models for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12632190/]
- 85. Comparative Evaluation of AI-Based Pathogenicity ... [https://www.sciencedirect.com/science/article/pii/S1877050925035574]
- 86. Deep learning tools predict variants in disordered regions with ... [https://bmcgenomics.biomedcentral.com/articles/10.1186/s12864-025-11534-9]
- 87. 精准预测:基于机器学习的乳腺癌错义变异致病性预测模型研究 [https://www.ebiotrade.com/newsf/2025-11/20251121091431035.htm]
- 88. PreMode predicts mode-of-action of missense variants by ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12325985/]
- 89. Benchmarking AlphaMissense pathogenicity predictions ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12145806/]
- 90. [论文评述] Dynamicasome: a molecular dynamics-guided ... [https://www.themoonlight.io/zh/review/dynamicasome-a-molecular-dynamics-guided-and-ai-driven-pathogenicity-prediction-catalogue-for-all-genetic-mutations]
- 91. MVP predicts the pathogenicity of missense variants by ... [https://www.nature.com/articles/s41467-020-20847-0]
- 92. Availability of benign missense variant "truthsets" for ... [https://pubmed.ncbi.nlm.nih.gov/40925377/]
- 93. Extracting and calibrating evidence of variant pathogenicity ... [https://www.sciencedirect.com/science/article/pii/S0002929725002435]
- 94. A novel seven-tier framework for the classification of MEFV ... [https://www.nature.com/articles/s41598-025-94142-7]
- 95. Computational and experimental methods for classifying ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9059783/]
- 96. ClinVar Instructions - ClinGen | Clinical Genome Resource [https://www.clinicalgenome.org/share-your-data/laboratories/clinvar-instructions/]
- 97. Instructions for ClinVar submission spreadsheets - NCBI [https://www.ncbi.nlm.nih.gov/clinvar/docs/spreadsheet/]
- 98. Enhancing Missense Variant Pathogenicity Prediction with ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11429773/]
- 99. ClinVar Genomic variation as it relates to human health - NCBI [https://www.ncbi.nlm.nih.gov/clinvar/variation/90454]
- 100. Paralog Explorer: A resource for mining information about ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9712503/]
- 101. PreMode predicts mode-of-action of missense variants by ... [https://www.nature.com/articles/s41467-025-62318-4]
- 102. Paralog-based synthetic lethality: rationales and applications [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2023.1168143/full]
- 103. Identifying pathogenicity of human variants via paralog-based ... [https://journals.plos.org/plosgenetics/article?id=10.1371/journal.pgen.1006779]