Forecasting the Viral Arms Race: Key Challenges and AI-Driven Solutions in Predicting Viral Evolution
This article examines the formidable challenges in predicting viral evolution, a critical task for proactive vaccine design and pandemic preparedness.
Forecasting the Viral Arms Race: Key Challenges and AI-Driven Solutions in Predicting Viral Evolution
Abstract
This article examines the formidable challenges in predicting viral evolution, a critical task for proactive vaccine design and pandemic preparedness. It explores the fundamental biological constraints, such as epistasis and vast mutational space, that limit predictability. The review then details cutting-edge computational methodologies, including AI-driven language models and biophysical frameworks, that are being developed to overcome these hurdles. We further analyze the limitations of current models and the strategies for their optimization, and present rigorous validation paradigms comparing predictive performance against real-world viral emergence. Synthesizing insights from recent research, this article provides a comprehensive overview for scientists and drug developers on the transition from reactive tracking to proactive forecasting of high-risk viral variants.
The Fundamental Hurdles: Why Predicting Viral Evolution is Inherently Complex
FAQs: Core Concepts and Challenges
FAQ 1: What is the primary challenge in predicting viable viral variants from a vast mutational space? The principal challenge is epistasis—the phenomenon where the effect of one mutation depends on the presence or absence of other mutations in the genetic background. This non-additive interaction means that a mutation beneficial in one genetic context might be neutral or even deleterious in another, making evolutionary trajectories hard to predict. Approximately 49% of functional mutations identified in adaptive enzyme trajectories were neutral or negative on the wild-type background, only becoming beneficial after other "permissive" mutations had first been established [1]. This severely constrains predictability.
FAQ 2: How can we experimentally measure the functional impact of thousands of mutations? Deep Mutational Scanning (DMS) is a key high-throughput technique. It involves creating a vast library of mutant genes or genomes, applying a selective pressure (e.g., antiviral treatment, host immune factors, or growth in a specific cell type), and then using next-generation sequencing to quantify the enrichment or depletion of every mutation before and after selection [2]. This links genotype to phenotype on a massive scale, revealing residues critical for viral replication, immune evasion, or drug resistance.
FAQ 3: What experimental strategies can help manage the problem of epistasis? Strategies include:
- Stability-Focused Filtering: When designing mutant libraries, computationally filter out mutations predicted to significantly destabilize the viral protein. This enriches libraries for functional variants, as many deleterious mutations are destabilizing [3].
- Stepwise Traversal: Mimic natural evolution by accumulating mutations step-by-step, re-assessing the fitness of each new mutation on the current genetic background rather than just the wild-type backbone. This can help identify positive epistasis that opens up new adaptive paths [1].
- Recombination: Crossing independently evolved, highly functional variants (that differ by many mutations) can help map the fitness landscape and identify which combinations of mutations are most productive [3].
FAQ 4: What is the mutation rate of SARS-CoV-2, and which mutation type is most common? Recent ultra-sensitive sequencing (CirSeq) of six SARS-CoV-2 variants indicates a mutation rate of approximately ~1.5 × 10⁻⁶ per base per viral passage. The mutation spectrum is heavily biased, dominated by C → U transitions, which occur about four times more frequently than any other base substitution [4].
FAQ 5: Which sequencing methods are best for detecting low-frequency variants in a viral population?
- Single-Genome Amplification (SGA): This method uses limiting-dilution PCR and Sanger sequencing to sequence individual viral templates from a mixed population. It prevents in vitro recombination, excludes Taq polymerase errors, and provides proportional representation of the viral population, offering deep resolution [5].
- Illumina-based Next-Generation Sequencing (NGS): This provides ultra-deep analysis of the viral population, capable of identifying minor variants that SGA might miss. It is ideal for quantifying viral barcode lineages, identifying CTL escape sites, and integration site analysis [5].
Troubleshooting Common Experimental Issues
Problem: Low diversity or high proportion of non-functional clones in mutant library.
- Potential Cause 1: The library design included a high number of destabilizing mutations.
- Solution: Incorporate a computational filtering step during library design. Use protein modeling software (e.g., Rosetta) to calculate the predicted change in folding free energy (ΔΔG) for each single-point mutation and exclude those predicted to be highly destabilizing (e.g., ΔΔG below a set threshold). This can exclude up to ~50% of possible mutations without losing beneficial ones [3].
- Potential Cause 2: Inefficient or error-prone library synthesis.
- Solution: Optimize the synthesis protocol. Consider using circular polymerase extension reaction (CPER) or yeast artificial chromosome (YAC) systems for more stable and efficient propagation of viral cDNA, especially for large RNA virus genomes [2].
Problem: Inconsistent fitness measurements for mutations across different experiments.
- Potential Cause: The genetic background of the virus used in the experiment has changed, leading to epistatic interactions.
- Solution: Always sequence the entire backbone of your viral clone before and after experiments to track unintended changes. When reporting results, clearly state the exact genetic background (parent strain and all accumulated mutations) on which the measurements were made [1].
Problem: Difficulty in distinguishing beneficial mutations from neutral "hitchhikers" during directed evolution.
- Potential Cause: Beneficial mutations can be linked to neutral or slightly deleterious mutations on the same genome, causing them to co-enrich.
- Solution: After a selection round, perform clonal isolation and analysis. Isolate individual variants and test their fitness individually. Site-directed mutagenesis can also be used to reintroduce a specific mutation into a "clean" background to confirm its effect [1] [3].
Data Tables
Table 1: Quantifying Mutational Landscapes and Epistasis
| Metric | Value / Finding | Experimental System | Citation |
|---|---|---|---|
| Proportion of epistatic functional mutations | ~49% of beneficial mutations were neutral or deleterious on the wild-type background | Analysis of 9 adaptive trajectories in enzymes | [1] |
| SARS-CoV-2 mutation rate | ~1.5 × 10⁻⁶ per base per viral passage | CirSeq of 6 variants (e.g., WA1, Alpha, Delta) in VeroE6 cells | [4] |
| Most common mutation type in SARS-CoV-2 | C → U transitions (~4x more frequent than other substitutions) | CirSeq mutation spectrum analysis | [4] |
| Proportion of predicted destabilizing single mutations | ~49.3% (2,839 of 5,758 possible single-site mutations) | Rosetta ΔΔG calculation on Kemp eliminase HG3 | [3] |
| Preferred sequence context for C→U mutations | 5'-UCG-3' | Nucleotide context analysis of SARS-CoV-2 mutation spectrum | [4] |
Table 2: Research Reagent Solutions for Viral Mutational Studies
| Reagent / Tool | Function in Research | Example Application / Note |
|---|---|---|
| Reverse Genetics System (plasmid/BAC) | Enables stable propagation and manipulation of viral genome as cDNA for mutagenesis. | Essential for constructing mutant libraries; systems with HCMV or T7 promoters allow direct viral RNA production [2]. |
| Circular Polymerase Extension Reaction (CPER) | A bacterium-free method to assemble and rescue infectious viral clones. | Reduces issues with bacterial toxicity and recombination of viral cDNA, improving library diversity [2]. |
| Viriation Tool (with NLP models) | Curates and summarizes functional annotations for viral mutations from literature. | Used in platforms like VIRUS-MVP to provide near-real-time functional insights on mutations [6]. |
| Single-Genome Amplification (SGA) | Provides high-fidelity, linked sequence data from individual viral templates in a quasispecies. | Critical for studying viral evolution, compartmentalization, and characterizing viral reservoirs without in vitro recombination [5]. |
| Barcoded Virus Libraries | Allows highly multiplexed tracking of specific viral lineages during complex infections. | Enables unprecedented identification and quantification of minor variants in plasma and tissues via NGS [5]. |
| VeroE6 Cells | A mammalian cell line highly susceptible to infection for viral culture and passage. | Preferred for COVID-19 research as it supports high viral replication and permits a higher degree of genetic diversity [4]. |
Detailed Experimental Protocols
Protocol 1: Deep Mutational Scanning (DMS) for Viral Fitness
Objective: To determine the effect of all possible single-amino-acid substitutions in a viral protein on viral replicative fitness.
Methodology:
- Library Construction:
- Use site-directed mutagenesis or error-prone PCR on the gene of interest cloned within an infectious cDNA clone or a subgenomic plasmid to generate a comprehensive mutant library. Aim for coverage that includes all possible single-amino-acid changes [2].
- Virus Recovery:
- Application of Selective Pressure:
- Propagate the rescued virus library under the desired condition. This could be:
- Passaging in a specific cell type (e.g., human vs. animal cells) to study adaptation.
- Treatment with a neutralizing antibody or antiviral drug to identify escape mutations.
- Growth under innate immune pressure [2].
- Important: Use a low multiplicity of infection (MOI ~0.1) during passaging to minimize co-infection and complementation, which can mask the effect of deleterious mutations [4].
- Propagate the rescued virus library under the desired condition. This could be:
- Sequencing and Data Analysis:
- Extract viral RNA from the virus population both pre- and post-selection.
- Prepare sequencing libraries for the target gene and perform high-depth next-generation sequencing (Illumina NGS is standard) [2] [5].
- Fitness Score Calculation: For each mutation, a fitness score is calculated by comparing its frequency in the post-selection population to its frequency in the pre-selection population (or the plasmid library), often using a log2 ratio. Normalize scores to synonymous mutations, which are generally assumed to be neutral [2].
Protocol 2: Stability-Informed Library Design for Directed Evolution
Objective: To create a "smart" mutant library enriched for functional, well-folded protein variants by excluding predicted destabilizing mutations.
Methodology:
- Saturation List Definition:
- Define the set of residues to saturate based on the experimental goal (e.g., all residues within 6 Å of the active site, all surface residues, or the entire protein) [3].
- In silico Stability Filtering:
- For every residue in the saturation list, calculate the predicted change in folding free energy (ΔΔG) for all 19 possible amino acid substitutions. Use a computational tool like the Cartesian ΔΔG protocol in the Rosetta software suite [3].
- Set a ΔΔG threshold (e.g., -0.5 Rosetta Energy Units) and exclude all mutations predicted to be more destabilizing than this threshold from the final library design.
- Oligo Pool Design and Gene Synthesis:
- Design DNA oligonucleotides (oligos) covering the entire gene, incorporating the filtered set of mutations. This can be done using short oligo fragments (e.g., ~200 bp) that are later assembled into full-length genes via overlap extension PCR [3].
- Library Assembly and Screening:
- Assemble the full-length gene library and clone it into an appropriate expression vector.
- Screen or select the resulting variant library for the desired function (e.g., catalytic activity, binding affinity). The enriched library will have a higher probability of containing improved, stable variants, accelerating the engineering process [3].
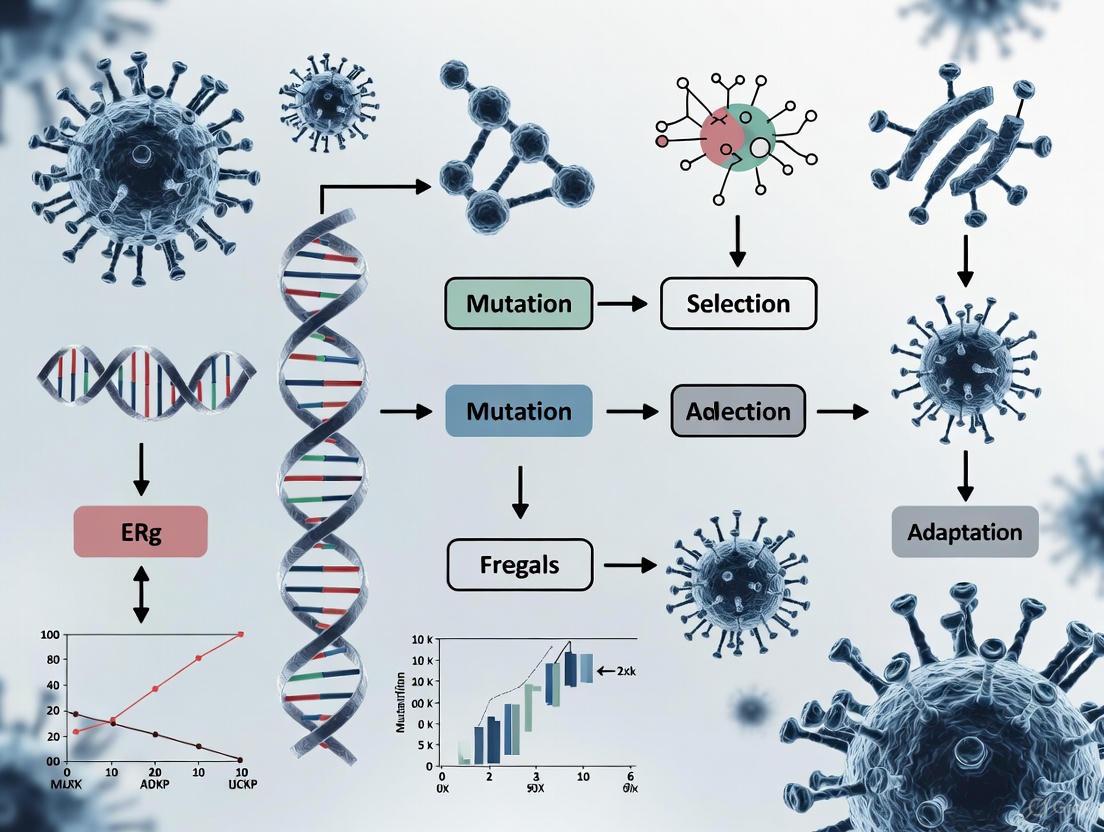
Experimental Workflow Visualizations
DMS Workflow for Viral Fitness
Epistasis in Evolutionary Trajectories
Stability-Informed Library Design
FAQs & Troubleshooting Guides
Fitness Profiling and Sequence Analysis
Q: My fitness profiling experiment identifies functional residues that are not evolutionarily conserved. Are these results valid?
- A: Yes, this is a recognized and biologically significant phenomenon. Conventional sequence conservation analysis can produce both false positives (conserved but functionally silent residues) and false negatives (functional but non-conserved, type-specific residues) [7]. Your results likely highlight type-specific functional residues, which are prevalent but not identifiable through conservation analysis alone. You can validate these findings by coupling the fitness profiling data with computational protein stability predictions to distinguish residues essential for function from those critical for structural stability [7].
Q: How can I experimentally identify functional residues in a viral protein without relying on sequence conservation?
- A: A proven methodology involves coupling high-throughput experimental fitness profiling with computational protein stability prediction [7].
- Create Mutant Libraries: Use a "small library" strategy where you generate a mutant library (e.g., via error-prone PCR) for a region coverable by a single sequencing read. This ensures only one mutation per genome is present, simplifying fitness calculations [7].
- Perform Fitness Selection: Rescue the mutant virus library and passage it in a relevant cell line (e.g., A549 cells for influenza) to apply selective pressure [7].
- Deep Sequencing & Analysis: Sequence the plasmid library (pre-selection) and the viral population post-selection. Identify mutations that change in frequency to calculate fitness effects [7].
- Integrate Stability Data: Use available protein structural information to computationally predict the stability effect of each substitution. This integration helps pinpoint residues under functional constraint, independent of their conservation status [7].
Q: What could explain sudden, rapid evolutionary bursts in a viral population maintained in a constant laboratory environment?
- A: In a constant environment, where external triggers are absent, evolutionary bursts can be caused by endogenous factors [8].
- Primary Cause: Chromosomal rearrangements, particularly segmental duplications, are a major trigger for the strongest bursts, as they can create new genetic material for innovation [8].
- Other Mechanisms: Bursts can also be initiated by fitness valley crossing (where a deleterious mutation is fixed, potentially leading to a fitter genotype) or movement along neutral ridges (neutral mutations that eventually lead to a beneficial one) [8].
- Troubleshooting: If you observe such bursts, analyze your genomic data not just for single-nucleotide substitutions, but also for larger structural variations and duplications.
Predictive Modeling and Variant Forecasting
Q: How can I accurately predict which viral variants will become dominant, given that mutations often interact (epistasis)?
- A: Previous models that did not account for epistasis had limited accuracy. For more robust predictions, use a biophysics-aware model that quantitatively links viral fitness to specific biophysical properties [9].
- Key Parameters: Model the variant's binding affinity to host receptors and its ability to evade neutralizing antibodies [9].
- Incorporating Epistasis: Ensure the model explicitly factors in epistasis—the phenomenon where the effect of one mutation depends on the presence of others. This is essential because evolution is non-linear, and epistatic interactions can unlock new adaptive pathways [9].
Q: We have limited experimental capacity. How can we prioritize which variants to test for transmissibility and immune evasion?
- A: Implement an AI-driven active learning framework like VIRAL (Viral Identification via Rapid Active Learning) [9].
- Workflow: This framework combines a biophysical model with artificial intelligence to iteratively select the most promising variant candidates for experimental testing [9].
- Efficiency: This approach can identify high-risk SARS-CoV-2 variants up to five times faster than conventional methods, requiring less than 1% of the experimental screening effort [9].
- Procedure: The AI proposes candidates based on predicted fitness; you test these experimentally and feed the results back into the model to refine subsequent predictions, creating a highly efficient feedback loop.
Experimental Protocols & Data
Protocol: High-Throughput Fitness Profiling of a Viral Protein
This protocol is adapted from the "small library" approach used to profile the influenza A virus PA polymerase subunit [7].
Library Design and Construction:
- Amplicon Generation: Use error-prone PCR to introduce random mutations into a 240 bp segment of the target gene.
- Vector Preparation: Generate the corresponding vector backbone via high-fidelity PCR.
- Cloning: Digest both the mutated amplicon and the vector with type IIs restriction enzymes (e.g., BsaI/BsmBI) and ligate them to create the plasmid mutant library. Aim for a library of ~50,000 clones for sufficient coverage [7].
Virus Rescue and Selection:
- Transfection: Co-transfect the plasmid mutant library with the remaining wild-type plasmids of the viral reverse genetics system into a packaging cell line (e.g., 293T cells) [7].
- Infection: Harvest the rescued viral mutant library and use it to infect a susceptible cell line (e.g., A549 cells) for 24 hours to apply selective pressure [7].
Sequencing and Fitness Calculation:
- Sample Preparation: Subject the initial plasmid mutant library (DNA control), the post-transfection library, and the post-infection library to deep sequencing [7].
- Variant Frequency Analysis: Map sequencing reads to the reference genome and count the frequency of each mutation in the pre- and post-selection populations.
- Fitness Score: Calculate the relative fitness of a mutation based on the change in its frequency after selection. A mutation that enriches is likely beneficial or functionally important, while one that depletes is likely deleterious.
Protocol: Forecasting High-Risk Variants with VIRAL Framework
This protocol outlines the use of the VIRAL (Viral Identification via Rapid Active Learning) framework for SARS-CoV-2 spike protein [9].
Define the Prediction Goal: Clearly state the objective, such as identifying spike protein mutations that enhance ACE2 binding affinity and/or confer antibody evasion.
Implement the Biophysical Model:
- Develop or use an existing model that computes viral fitness based on biophysical parameters. The model must incorporate epistatic interactions between mutations [9].
Integrate Active Learning Loop:
- The AI proposes a small batch of variant candidates predicted to have the highest fitness.
- These candidates are synthesized and tested experimentally for binding and neutralization.
- The experimental results are fed back into the model to refine its future predictions.
Validation: The process iterates until high-fitness variants are identified with high confidence. The output is a ranked list of variants most likely to become dominant.
Quantitative Data on Viral Evolution
Table 1: Causes of Evolutionary Bursts in Viral Populations in a Constant Environment [8]
| Cause of Burst | Description | Relative Contribution |
|---|---|---|
| Segmental Duplication | Duplication of a genomic segment, providing new material for evolution. | Major trigger for the strongest bursts. |
| Fitness Valley Crossing | Fixation of a deleterious mutation that eventually allows access to a fitter genotype. | Occurs occasionally. |
| Neutral Ridge Traveling | Neutral mutations that do not affect fitness until a beneficial mutation is found. | Occurs occasionally. |
Table 2: Performance of Predictive Frameworks for Viral Variants [9]
| Framework / Method | Key Feature | Reported Efficiency Gain |
|---|---|---|
| Conventional Approaches | Often lacks epistasis; tests variants broadly. | Baseline (1x) |
| VIRAL (AI + Biophysical Model) | Incorporates epistasis; focuses experiments via active learning. | Identifies variants 5x faster, using <1% of experimental screening. |
Workflow and Conceptual Diagrams
Fitness Profiling Workflow
Fitness Landscape and Evolutionary Bursts
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Tools for Viral Fitness and Evolutionary Studies
| Tool / Resource | Function / Application | Example / Note |
|---|---|---|
| Reverse Genetics System | Rescues infectious virus from plasmid DNA; essential for introducing mutant libraries. | 8-plasmid system for Influenza A/WSN/33 [7]. |
| "Small Library" Mutagenesis | Generates mutant libraries with only one mutation per genome, simplifying fitness analysis. | 240 bp amplicon covered by a single sequencing read [7]. |
| Type IIs Restriction Enzymes | Enables seamless, directional cloning of mutated amplicons into the vector backbone. | BsaI or BsmBI [7]. |
| Deep Sequencing Platform | Tracks the frequency of thousands of mutations before and after selection in parallel. | Illumina MiSeq [7]. |
| Biophysical Modeling Software | Predicts how mutations affect viral traits like receptor binding and antibody escape. | Core component of the VIRAL forecasting framework [9]. |
| Evolutionary Simulation Platform | Models long-term viral evolution in silico to test hypotheses and study dynamics. | Aevol platform for simulating virus-like genomes [8]. |
| Software Packaging (Conda/Bioconda) | Manages tool dependencies and installation, ensuring computational reproducibility. | Simplifies use of complex evolutionary bioinformatics tools [10]. |
| Integrative Framework (Galaxy) | Provides a unified web interface for combining multiple analytical tools into workflows. | Offers access to hundreds of tools without command-line installation [10]. |
In the field of viral evolution, a significant challenge complicates predictions: epistasis, the phenomenon where the effect of a genetic mutation depends on the presence of other mutations in the genome [11]. This non-linearity means that the fitness effect of a mutation in one viral variant may be beneficial, but the same mutation could be neutral or even deleterious in the genetic background of a different variant [11] [12]. For researchers forecasting the emergence of high-risk viral strains, this interaction creates a complex, rugged fitness landscape where evolutionary paths are difficult to anticipate. The ability to predict which variants will dominate, such as in influenza or SARS-CoV-2, is therefore substantially hampered by these unpredictable genetic interactions [13] [14]. Understanding and accounting for epistasis is not merely an academic exercise; it is a critical step toward improving the accuracy of evolutionary forecasts and developing more resilient therapeutic strategies.
Frequently Asked Questions (FAQs)
Q1: What exactly is epistasis, and why is it a "challenge" in my viral variant research? Epistasis refers to genetic interactions where the effect of one mutation is dependent on the genetic background of other mutations [11]. It is a challenge because it violates the assumption of additivity that underpins many simple predictive models. When epistasis occurs, you cannot simply add up the individual effects of mutations to know a variant's overall fitness. This non-linearity makes it difficult to forecast which viral genotypes will emerge and become dominant, complicating tasks like vaccine selection and drug development [13] [15].
Q2: Are there predictable patterns of epistasis, or are all interactions completely idiosyncratic? Research shows that while specific interactions can be unique, global patterns often emerge. The most commonly observed pattern is "diminishing-returns" epistasis, where a beneficial mutation has a smaller fitness advantage in already-fit genetic backgrounds compared to less-fit backgrounds [11]. Conversely, "increasing-costs" epistasis describes deleterious mutations becoming more harmful in fitter backgrounds [11]. However, the shape and strength of these global patterns can themselves be altered by environmental factors like drug concentration [15].
Q3: How does the environment influence epistasis in my experiments? The environment can powerfully modulate epistatic interactions. For example, a study on P. falciparum showed that the same set of drug-resistance mutations exhibited diminishing-returns epistasis at low drug concentrations but switched to increasing-returns epistasis at high concentrations [15]. This means that the genetic interactions you map in one environmental condition (e.g., a specific drug dose) may not hold true in another. Your experimental conditions are not just a backdrop; they are an active participant in shaping the fitness landscape.
Q4: What is the difference between global epistasis and idiosyncratic epistasis?
- Global Epistasis describes a consistent, predictable relationship between the fitness effect of a mutation and the fitness of its genetic background. It can often be captured by a simple mathematical function, making it somewhat predictable [11] [15].
- Idiosyncratic Epistasis describes interactions that are highly specific to particular combinations of mutations and cannot be predicted from general rules like background fitness. These require detailed, case-by-case experimental mapping [15].
The balance between global and idiosyncratic epistasis for a given set of mutations can be visualized on a "map of epistasis," and this position can shift with environmental change [15].
Q5: Can we still predict evolution despite widespread epistasis? Yes, but with limitations. Short-term predictions in controlled environments are most feasible [13]. Approaches include:
- Leveraging patterns of global epistasis to model the distribution of fitness effects [11].
- Using high-throughput deep mutational scanning to empirically measure interactions in a focal gene [11] [16].
- Applying co-occurrence analysis of mutation hotspots in sequence data to flag potential high-risk variants [14]. However, long-term prediction remains challenging due to environmental fluctuations and the accumulation of complex, higher-order genetic interactions [13] [16].
Troubleshooting Common Experimental Problems
Problem 1: Unpredictable Fitness Measurements in Different Genetic Backgrounds
Symptoms: A mutation known to be beneficial in one viral strain shows neutral or deleterious effects when introduced into a new strain. Your fitness predictions fail when crossing genetic backgrounds.
Diagnosis: This is a classic symptom of idiosyncratic epistasis [11] [15]. The effect of your focal mutation is being modified by specific, unaccounted-for genetic variants in the new background.
Solutions:
- Map the Interaction: Systematically measure the fitness of the focal mutation across a panel of isogenic strains that differ at the other suspect loci.
- Quantify Epistasis: Calculate epistasis (ε) using the formula:
ε = log(f~12~/f~0~) - [log(f~1~/f~0~) + log(f~2~/f~0~)] where f~0~ is the ancestral genotype fitness, f~1~ and f~2~ are single mutant fitnesses, and f~12~ is the double mutant fitness [12].
- Account for Environment: Re-run your assays across a range of relevant environmental conditions (e.g., drug concentrations, host cell types) to see if the interaction is stable or context-dependent [15].
Problem 2: Inconsistent Evolutionary Trajectories in Replicate Populations
Symptoms: In experimental evolution studies, replicate populations started from the same genotype evolve along different genetic paths, leading to different adaptive outcomes.
Diagnosis: Epistasis can create a rugged fitness landscape with multiple peaks. Small, stochastic events early on (e.g., which beneficial mutation arises first) can send populations down different, inaccessible paths due to negative epistatic interactions between mutations [11].
Solutions:
- Increase Replication: Use a large number of replicate lines to fully capture the distribution of possible evolutionary outcomes.
- Deep Sequencing: Perform high-temporal-resolution whole-genome sequencing to identify the order and identity of fixed mutations.
- Reconstruct Histories: Genetically reconstruct the evolutionary histories in different orders to test for historically contingent effects, where the effect of a late mutation depends on earlier mutations that paved the way [11].
Problem 3: Poor Performance of Models Trained on Data from a Single Environment
Symptoms: A predictive model for variant fitness, trained on data from one environment (e.g., a specific drug dose), performs poorly when applied to data from a different environment.
Diagnosis: Gene-by-Environment (GxE) interactions are modulating the underlying epistatic interactions, effectively changing the topography of the fitness landscape [15].
Solutions:
- Incorporate Environmental Variance: Train your models on fitness data collected across a gradient of environmental conditions relevant to your forecasting goals.
- Use a "Map of Epistasis": For key mutations, quantify how the strength (variance of fitness effects) and nature (R² of global epistasis model) of epistasis change across environments, as shown in the table below [15].
- Model Underlying Traits: Consider if a non-linear mapping from an unobserved biophysical trait (e.g., protein stability) to fitness can explain the changing patterns across environments [11].
Table: How Drug Dose Modulates Global Epistasis for Different Mutations in P. falciparum DHFR [15]
| Mutation | Low Drug Dose Pattern | High Drug Dose Pattern | Change in Epistasis Strength | Change in Globalness (R²) |
|---|---|---|---|---|
| C59R | Diminishing Returns | Increasing Returns | Constant (var ~1) | Decreases |
| I164L | Diminishing Returns | Diminishing Returns | Constant (var ~1) | Increases |
| N51I | Idiosyncratic | Weak Epistasis | Decreases | Variable |
| S108N | Partly Global | Highly Idiosyncratic | Constant | Decreases |
Key Experimental Protocols for Characterizing Epistasis
Protocol 1: Deep Mutational Scanning to Map a Local Fitness Landscape
Objective: To empirically measure the fitness effects of all single mutants and many double mutants within a viral gene of interest (e.g., the Spike protein) in a single, high-throughput experiment [11] [17].
Methodology:
- Library Construction: Use site-directed mutagenesis or synthetic gene synthesis to create a comprehensive library of viral gene variants, encompassing all single amino acid changes and a selected set of double mutants.
- Selection Experiment: Package the variant library into pseudoviruses and subject them to a selective pressure (e.g., convalescent serum, a monoclonal antibody, or a host cell line). The workflow for this process is outlined below.
- Deep Sequencing: Sequence the variant library before and after selection using high-throughput sequencing to quantify the frequency of each variant.
- Fitness Calculation: Calculate the relative fitness of each variant as the log~2~ ratio of its frequency after selection to its frequency before selection.
- Epistasis Calculation: Identify epistatic pairs by comparing the measured fitness of double mutants to the expected fitness under an additive or multiplicative model [12].
Protocol 2: Measuring Global Epistasis Across Genetic Backgrounds
Objective: To determine how the fitness effect of a focal mutation changes as a function of the fitness of its genetic background [11] [15].
Methodology:
- Background Selection: Select a diverse set of 10-15 genetically distinct variants (e.g., natural isolates or engineered strains) that span a wide range of fitness values. These will serve as your genetic backgrounds.
- Generate Isogenic Lines: Use reverse genetics to introduce the precise focal mutation into each of the selected genetic backgrounds, creating a matched set of mutant strains.
- Fitness Assays: In a controlled environment, perform head-to-head competition assays between each mutant strain and its respective parental background. Alternatively, measure growth rates or viral titers for each strain individually.
- Data Analysis: Calculate the fitness effect (Δf) of the focal mutation in each background as the fitness difference between the mutant and its parent. Plot Δf against the fitness of the parental background (f(B)).
- Model Fitting: Fit a linear (or other) regression model to the data. The slope and R² of this model describe the pattern and "globalness" of epistasis, respectively [15].
Research Reagent Solutions
Table: Essential Materials for Epistasis Research in Viral Variants
| Reagent / Material | Function in Experiment | Specific Examples / Notes |
|---|---|---|
| Comprehensive Mutant Library | Provides the genetic diversity to screen for interactions. | Can be generated for a single gene (e.g., Spike) via oligo synthesis [17]. |
| Pseudotyped Virus System | Safely study entry of variants for high-risk pathogens. | Allows testing of spike mutations without full BSL-3 constraints [14]. |
| Monoclonal Antibodies / Convalescent Sera | Provides selective pressure to map antibody escape. | Critical for defining the antigenic landscape [14]. |
| Susceptible Cell Lines | Host for viral replication and competition assays. | e.g., A549 cells expressing hACE2 for SARS-CoV-2 entry assays [14]. |
| High-Throughput Sequencer | Quantify variant frequency pre- and post-selection. | Essential for Deep Mutational Scanning [11] [17]. |
| Reverse Genetics System | Engineer specific mutations into desired genetic backgrounds. | Key for testing causal effects and generating isogenic lines [15]. |
Frequently Asked Questions (FAQs)
FAQ 1: Why do my stochastic models of viral evolution become computationally prohibitive when simulating large population sizes, and how can I overcome this?
Answer: This is a common challenge when modeling viral populations where large wild-type populations coexist with small, stochastically emerging mutant sub-populations. Traditional fully stochastic algorithms, like Gillespie's method, become computationally expensive because the average time step decreases as the total population size increases [18] [19].
A recommended solution is to implement a hybrid stochastic-deterministic algorithm. This approach treats large sub-populations (e.g., established wild-type virus) with deterministic ordinary differential equations (ODEs), while simulating small, evolutionarily important sub-populations (e.g., nascent mutants) with stochastic rules. This method approximates the full stochastic dynamics with sufficient accuracy at a fraction of the computational time and allows for the quantification of key evolutionary endpoints that pure ODEs cannot capture, such as the probability of mutant existence at a given infected cell population size [18] [19].
FAQ 2: My analysis of viral sequence data fails to detect recombination events that I know are present. What are the primary technical challenges in recombination detection?
Answer: The accurate detection of recombination is methodologically challenging. A major hurdle is distinguishing genuine recombination from other evolutionary signals, particularly when the genomic lineage evolution is driven by a limited number of single nucleotide polymorphisms or when sequences are highly similar [20]. Furthermore, the statistical power to detect recombination is low when the same genomic variants arise independently in different lineages (convergent evolution) [21].
To improve detection, ensure you are using multiple analytical procedures specifically designed for this purpose. Methods vary and include those based on phylogenetic incompatibility, compatibility matrices, and statistical tests for the breakdown of linkage disequilibrium. Always use a combination of these tools, not just one, and be aware that next-generation sequencing technologies, while offering new opportunities, also present serious analytical challenges that must be considered [21].
FAQ 3: In the context of HIV, under what conditions does recombination significantly accelerate the evolution of drug resistance?
Answer: The impact of recombination is not constant and depends critically on the effective viral population size (Ne) within a patient. Stochastic models show that for small effective population sizes (e.g., around 1,000), recombination has only a minor effect, as beneficial mutations typically fix sequentially. However, for intermediate population sizes (104 to 105), recombination can accelerate the evolution of drug resistance by up to 25% by bringing together beneficial mutations [22].
The fitness interactions (epistasis) between mutations also determine the outcome. If resistance mutations interact synergistically (positive epistasis), recombination can actually break down these favorable combinations and slow down evolution. The predominance of positive epistasis in HIV-1 in the absence of drugs suggests recombination may not facilitate the pre-existence of drug-resistant virus prior to therapy [22].
Troubleshooting Guides
Issue 1: Inaccurate Projection of Variant Emergence
Problem: Models fail to forecast the emergence of high-risk viral variants that combine multiple mutations.
Solution:
- Incorporate Epistasis: Update your fitness models to account for non-linear interactions between mutations. "Evolution isn't linear — mutations interact, sometimes unlocking new pathways for adaptation" [9]. Factoring in these relationships is key to forecasting the emergence of dominant variants.
- Implement Advanced Forecasting Frameworks: Adopt computational frameworks like VIRAL (Viral Identification via Rapid Active Learning), which combines biophysical models (e.g., spike protein binding affinity and antibody evasion capacity) with artificial intelligence. This framework can identify high-risk SARS-CoV-2 variants up to five times faster than conventional approaches, focusing experimental validation on the most concerning candidates [9].
- Validate with Multiscale Data: Use a multiscale model that quantitatively links biophysical features of viral proteins (like binding affinity) to a variant's likelihood of surging in global populations. Cross-reference model predictions with epidemiological data on variant frequency [9].
Issue 2: Modeling the Impact of Multiple Infection and Cell-to-Cell Transmission
Problem: The evolutionary consequences of multiple infection of cells, particularly via virological synapses, are neglected or oversimplified in the model.
Solution:
- Model Structure: Formulate your model to track cells infected with
icopies of the virus, whereiranges from 0 to a maximum N. Include separate transmission terms for free-virus infection (typically adding one virus genome) and synaptic transmission (which can addSviruses at once) [18] [19]. - Account for Intracellular Interactions: Within multiply infected cells, model key interactions:
- Complementation: Where a defective mutant is rescued by a functional virus co-infecting the same cell.
- Interference: Where an advantageous mutant has its fitness reduced by competition with co-infecting viruses.
- Use a Hybrid Algorithm: Apply a hybrid stochastic-deterministic approach to efficiently simulate this system, where the large population of singly infected cells is modeled deterministically, and the smaller sub-populations of multiply infected cells are modeled stochastically [18] [19]. This is crucial, as synaptic transmission can promote the co-transmission of distinct virus strains, enhancing the effects of complementation and interference, and thereby promoting viral evolvability.
Data Presentation
Table 1: Estimated Effective Population Size (Ne) of HIV from Various Studies
This parameter is critical for determining the stochastic versus deterministic dynamics of mutation and recombination [22].
| Study | Patient Group | Population Sampled | Gene(s) | Estimated Ne |
|---|---|---|---|---|
| Leigh Brown [22] | Untreated | Free virus | env | 1,000 - 2,100 |
| Nijhuis et al. [22] | Before & During Therapy | Free virus | env | 450 - 16,000 |
| Rodrigo et al. [22] | Before & During Therapy | Provirus | env | 925 - 1,800 |
| Rouzine and Coffin [22] | Untreated & On Therapy | Free virus/Provirus | pro | 100,000 |
| Seo et al. [22] | Untreated & On Therapy | Free virus/Provirus | env | 1,500 - 5,500 |
| Achaz et al. [22] | Untreated | Free virus | gag-pol | 1,000 - 10,000 |
Table 2: Comparison of Computational Approaches for Simulating Viral Evolution
A guide to selecting the appropriate modeling framework for your research question [18] [19].
| Method | Best Use Case | Key Advantages | Key Limitations |
|---|---|---|---|
| Fully Stochastic (e.g., Gillespie) | Small, well-mixed populations where all sub-populations are subject to stochasticity. | Precisely captures random fluctuations and extinction probabilities. | Computationally prohibitive for large population sizes. |
| Deterministic (ODEs) | Modeling the average behavior of very large populations where stochastic effects are minimal. | Computationally efficient; provides a single, clear trajectory for the system. | Cannot model the emergence of new mutants from zero; cannot compute distributions or probabilities of rare events. |
| Hybrid Stochastic-Deterministic | Large populations containing both large and very small sub-populations (e.g., acute HIV infection). | Balances accuracy and efficiency; allows calculation of evolutionary endpoints like mutant distributions. | More complex implementation than pure ODEs. |
Experimental Protocols
Protocol 1: Quantifying the Impact of Recombination on Drug Resistance In Silico
This protocol outlines a stochastic population genetic model to simulate the emergence of drug resistance in HIV, incorporating mutation and recombination [22].
1. Model Formulation:
- Genome: Represent a viral genome as two loci with two alleles each (e.g., a/A and b/B), where lowercase denotes drug-sensitive wild-type and uppercase denotes drug-resistant mutants.
- Population: Model a finite population of N infected cells, each carrying one or two proviruses. The frequency of doubly infected cells is
f, making the total number of proviruses (1 + f)N. - Life Cycle: Simulate discrete generations with these stochastic steps:
- Infection: Target cells are infected by virions, which can be homozygous or heterozygous.
- Reverse Transcription: During this process, template switching between the two genomic RNA strands in heterozygous virions occurs at a defined recombination rate.
- Selection: Newly infected cells (now proviruses) undergo selection based on their genotype fitness in the presence of drug therapy.
2. Key Parameters:
- Mutation Rate (μ): Use ( 3.4 \times 10^{-5} ) per base pair per replication cycle [22].
- Effective Population Size (Ne): varied between 103 and 105 based on empirical estimates [22].
- Fitness Values: Assign fitness to different genotypes (ab, Ab, aB, AB) based on empirical data, exploring both additive and synergistic (epistatic) interactions.
- Recombination Rate: Define the probability of template switching per replication cycle.
3. Simulation and Output:
- Run multiple stochastic simulations to account for random drift.
- Primary output: The number of generations or the probability for the double mutant (AB) to reach fixation in the population under different recombination rates and population sizes.
Protocol 2: A Hybrid Stochastic-Deterministic Algorithm for Simulating Mutant Evolution in Acute HIV Infection
This protocol details a method to overcome computational bottlenecks when simulating viral evolution in large populations with rare mutants [18] [19].
1. Define the Mathematical Model:
- Use a compartmental model that includes both free-virus transmission and direct cell-to-cell synaptic transmission.
- Define compartments for uninfected cells (x0) and cells infected with
icopies of the virus (xi), whereiranges from 1 to N. - Incorporate parameters for infection rates, viral production, cell death, and the number of viruses transferred per synaptic event (S).
2. Implement the Hybrid Algorithm:
- Set a Threshold: Choose a population threshold (e.g., 100 cells). Sub-populations below this threshold are modeled stochastically.
- Algorithm Flow:
- At each time step, calculate the propensities of all possible events (infection, death, etc.).
- For sub-populations below the threshold, use a stochastic method (e.g., tau-leaping) to update their numbers.
- For sub-populations above the threshold, update their numbers deterministically using ODEs derived from the model's reaction rates.
- Ensure conservation rules are maintained when moving cells between stochastically and deterministically modeled compartments.
3. Application:
- Use this algorithm to study how multiple infection and intracellular complementation facilitate the spread of otherwise disadvantageous mutants, a process heavily promoted by virological synapses [18] [19].
Mandatory Visualization
Diagram 1: Workflow of a Hybrid Stochastic-Deterministic Model for Viral Evolution
Hybrid Model Logic Flow
Diagram 2: Recombination and Mutant Formation in a Heterozygous Virion
Viral Recombination Mechanism
The Scientist's Toolkit: Research Reagent Solutions
| Reagent / Tool | Function in Research |
|---|---|
| Population Genetic Model (Stochastic) | To simulate the evolution of drug-resistant viral strains in finite populations, incorporating the interplay of mutation, recombination, genetic drift, and selection [22]. |
| Hybrid Stochastic-Deterministic Algorithm | A computational method to efficiently simulate mutant evolution in large viral populations (e.g., acute HIV) where very large (wild-type) and very small (mutant) sub-populations coexist [18] [19]. |
| Bioinformatic Recombination Detection Pipelines | Software tools for detecting, characterizing, and quantifying recombination events in viral sequence data, often leveraging high-throughput sequencing data [21]. |
| Multiscale Biophysical Model | A model that links quantitative biophysical features (e.g., protein binding affinity, antibody evasion) to viral fitness and variant spread in populations, often incorporating epistasis [9]. |
| VIRAL (Viral Identification via Rapid Active Learning) | A computational framework combining biophysical models with AI to accelerate the identification of high-risk viral variants that enhance transmissibility and immune escape [9]. |
The Predictive Toolkit: AI, Biophysical Models, and Integrative Frameworks
Troubleshooting Guides
Common Errors and Solutions
Problem: Model Fails to Converge During Training
- Symptoms: Training loss fluctuates wildly or plateaus at a high value; model generates nonsensical sequence predictions.
- Potential Causes & Solutions:
- Cause 1: Inadequate Data Preprocessing. Viral sequences may contain artifacts or mis-annotations.
- Solution: Implement a rigorous quality control pipeline. Use multiple sequence alignment (MSA) tools to verify sequence integrity and filter out outliers.
- Cause 2: Incorrect Hyperparameter Tuning. The learning rate may be too high, or the model architecture may be too complex for the available data.
- Solution: Perform a systematic hyperparameter sweep. Start with known values from similar studies (e.g., using a smaller transformer model) and use a validation set for guidance.
- Cause 3: Data Imbalance. The training set may overrepresent certain viral clades, causing the model to perform poorly on underrepresented variants.
- Solution: Apply data augmentation techniques or weighted loss functions to balance the influence of different sequence groups.
- Cause 1: Inadequate Data Preprocessing. Viral sequences may contain artifacts or mis-annotations.
Problem: Poor Generalization to Unseen Viral Variants
- Symptoms: Model performs well on training data but fails to accurately predict the fitness or properties of novel variants.
- Potential Causes & Solutions:
- Cause 1: Epistatic Interactions Not Captured. The model may focus on single-point mutations and miss complex, interdependent mutations.
- Solution: Incorporate probabilistic graphical models or attention mechanisms that explicitly model interactions between distant sites in the sequence.
- Cause 2: Lack of Structural or Functional Context. The model is trained solely on sequence data without biological constraints.
- Solution: Integrate protein structure prediction tools (e.g., AlphaFold2) into the pipeline. Use the predicted structures as additional input features to ground the language model's predictions in biophysical reality.
- Cause 1: Epistatic Interactions Not Captured. The model may focus on single-point mutations and miss complex, interdependent mutations.
Technical Implementation Issues
Problem: Memory Overflow with Large Language Models
- Symptoms: Training runs crash with "out of memory" errors, especially with long sequence lengths.
- Solution:
- Reduce the batch size during training.
- Use gradient accumulation to simulate a larger batch size.
- Employ model parallelism or use libraries optimized for memory efficiency (e.g., DeepSpeed).
- Consider using a model with a more efficient attention mechanism, such as Longformer or Performer, for very long viral genomes.
Frequently Asked Questions (FAQs)
Q1: What type of language model is best suited for analyzing viral sequences? A: While standard Transformer-based models (like BERT or GPT) are a good starting point, models tailored for biological sequences often perform better. Architectures like CNN-LSTM hybrids or models employing attention mechanisms trained on millions of diverse protein sequences (e.g., ESM, ProtTrans) have shown great promise as they inherently capture biophysical properties.
Q2: How much data is required to train a effective model for a specific virus? A: The amount of data required is highly variable. For well-studied viruses like Influenza or SARS-CoV-2, thousands of sequences may be sufficient for fine-tuning a pre-trained model. For emerging viruses with limited data, techniques like few-shot learning or transfer learning from models trained on broad viral families are essential. The quality and diversity of the data are often more critical than the sheer volume.
Q3: How can I validate that my model has learned biologically meaningful rules and is not just overfitting? A: Use a rigorous, multi-faceted validation approach:
- Hold-out Validation: Reserve a temporally recent set of variants (ones that emerged after your training data was collected) to test predictive accuracy.
- Wet-lab Collaboration: Collaborate with experimentalists to synthesize a few model-predicted high-fitness variants and test their viability in the lab (e.g., using pseudovirus assays). This is the gold standard.
- In-silico Mutagenesis: Systematically introduce mutations and check if the model's predictions align with known deleterious or advantageous mutations from literature.
Q4: What are the key computational resources needed for this research? A: A typical setup involves:
- Hardware: Access to high-performance computing (HPC) clusters or cloud computing platforms (AWS, GCP, Azure) is almost mandatory. Training large models requires multiple GPUs (e.g., NVIDIA A100 or V100) with substantial VRAM.
- Software: Python is the primary language, using deep learning frameworks like PyTorch or TensorFlow. Domain-specific libraries like Biopython are essential for sequence handling.
Experimental Protocol: Decoding Viral Grammar with a Transformer Model
Objective
To train a transformer-based language model to predict viable future viral variants by learning the evolutionary "grammar" from a curated dataset of historical viral genome sequences.
Step-by-Step Methodology
Data Curation & Preprocessing
- Source: Download all available nucleotide or amino acid sequences for your target virus (e.g., SARS-CoV-2 Spike protein) from public databases like GISAID or NCBI Virus.
- Alignment: Perform a multiple sequence alignment (MSA) using tools like MAFFT or ClustalOmega to ensure all sequences are positionally homologous.
- Filtering: Remove sequences with excessive ambiguity (e.g., too many 'X' or 'N' characters) and deduplicate the dataset.
- Split: Split the data chronologically: e.g., sequences up to a certain date for training/validation, and sequences after that date for testing temporal generalization.
Model Architecture & Training
- Architecture: Implement a decoder-only Transformer model (GPT-style) or an encoder model (BERT-style). The input is the aligned sequence, tokenized at the amino acid or codon level.
- Training Objective: Use a masked language modeling (MLM) objective, where the model learns to predict randomly masked tokens in the sequence. This forces it to learn the contextual constraints of the sequence.
- Hyperparameters:
- Optimizer: AdamW
- Learning Rate: 1e-4 to 1e-5 (with a warmup schedule)
- Batch Size: As large as GPU memory allows (32, 64, 128).
- Training Epochs: Until validation loss plateaus (monitor closely to avoid overfitting).
Variant Prediction & Analysis
- Fitness Scoring: For a given wild-type sequence, generate in-silico all possible single-point mutants. The model's log-likelihood or perplexity score for each mutant can be used as a proxy for its predicted fitness (lower perplexity = higher fitness).
- Evolutionary Tracing: Use the attention weights from the model to identify which parts of the sequence the model deems most critical when making predictions. These "important" positions can be mapped onto 3D protein structures to suggest functional hotspots.
Experimental Validation (Collaboration)
- Design: Select a shortlist of model-predicted high-fitness and low-fitness variants for synthesis.
- Testing: Partner with a BSL-2/3 lab to test these variants for functionality (e.g., binding affinity, replication rate) using appropriate assays.
The workflow for this protocol is as follows:
Data Presentation
| Model Architecture | Training Data Size (Sequences) | Perplexity (↓) | Top-10 Accuracy (%) (↑) | Temporal Generalization Score* (↑) |
|---|---|---|---|---|
| LSTM | 50,000 | 4.5 | 62 | 0.55 |
| Transformer (Base) | 50,000 | 3.1 | 78 | 0.71 |
| ESM-1b (Fine-tuned) | 50,000 | 2.4 | 85 | 0.82 |
| CNN-LSTM Hybrid | 50,000 | 3.8 | 70 | 0.63 |
*The Temporal Generalization Score is defined as the Pearson correlation between the model's predicted fitness score and the actual observed frequency of novel variants in the held-out test set over a 3-month period.
Table 2: In-silico Prediction vs. Experimental Validation for Selected Model-Predicted SARS-CoV-2 Variants
| Predicted Variant (Spike Protein) | Model Fitness Score (Perplexity) | Predicted Category | Experimental Binding Affinity (nM) (↓) | Experimental Replication Rate (Relative to WT) (↑) | Model-Experiment Concordance? |
|---|---|---|---|---|---|
| N501Y | 2.1 | High Fitness | 0.8 | 1.4 | Yes |
| E484K | 2.3 | High Fitness | 1.1 | 1.3 | Yes |
| A570D | 5.7 | Low Fitness | 12.5 | 0.7 | Yes |
| P681H | 2.9 | Neutral | 2.5 | 1.0 | Partial |
| K417T | 6.1 | Low Fitness | 15.2 | 0.6 | Yes |
Visualization of Core Concepts
Viral Grammar Decoding Workflow
Model Architecture Schematic
Table 3: Key Research Reagent Solutions for Viral Grammar Studies
| Item / Resource | Function / Application | Example Product / Tool |
|---|---|---|
| Pre-trained Protein Language Model (pLM) | Provides a strong foundational understanding of general protein sequence-structure relationships, enabling effective transfer learning for specific viruses. | ESM-2, ProtTrans |
| Multiple Sequence Alignment (MSA) Tool | Aligns homologous viral sequences to ensure positional correspondence, which is critical for accurate model training and analysis. | MAFFT, ClustalOmega |
| Deep Learning Framework | Provides the core software environment for building, training, and evaluating complex neural network models. | PyTorch, TensorFlow |
| Gradient Checkpointing Library | A software technique that reduces GPU memory consumption during training, allowing for the use of larger models or batch sizes on limited hardware. | torch.utils.checkpoint |
| Pseudovirus Assay System | A safe (BSL-2) experimental system to functionally validate model predictions by measuring the infectivity of predicted viral variants without handling live, high-containment viruses. | Commercial lentiviral pseudotype kits (e.g., for SARS-CoV-2) |
| High-Performance Computing (HPC) Cluster | Provides the necessary computational power (multiple GPUs, high RAM) to train large language models on millions of sequence data points in a feasible timeframe. | In-house cluster or Cloud (AWS, GCP) |
Frequently Asked Questions (FAQs)
Q1: What is a fitness model in the context of viral evolution, and why is it important? A fitness model is a computational framework that predicts the evolutionary success of a viral variant. It integrates quantitative traits like binding affinity (how strongly the virus attaches to a host cell receptor) and immune evasion (its ability to escape neutralization by antibodies) into a single fitness score. These models are crucial because they move beyond simply counting mutations; they help researchers anticipate which viral variants are likely to dominate, guiding the development of future vaccines and therapeutics [23] [13].
Q2: Our predictions of high-risk variants are often inaccurate. What key factors might we be missing? A primary challenge in evolutionary prediction is the reliance on incomplete data. Common missing factors include:
- Neoantigen Quality and Expression: It's not just the number of mutations, but their quality (strength of binding to MHC and T-cell receptors) and expression level that determine immune recognition. Down-regulation of highly immunogenic neoantigens is a key immune escape mechanism [24].
- Eco-evolutionary Feedback Loops: Viral evolution is shaped by its environment, including the host immune response. This creates feedback loops where the environment changes as the virus evolves, making long-term predictions challenging [13].
- Spatiotemporal Scales: Evolutionary rates and selective pressures differ between within-host and between-host dynamics. Integrating these scales is a significant hurdle [23].
Q3: How can AI help in designing vaccines against future viral variants? AI and computational biophysics enable a proactive approach to vaccine design. Methods like EVE-Vax can generate a panel of synthetic viral spike proteins designed to foreshadow potential future immune escape variants. This allows researchers to evaluate and optimize vaccines and therapeutics against predicted future strains, rather than only reacting to those that have already emerged [25].
Q4: What is the difference between a fitness model and a simple binding affinity measurement? While binding affinity is a critical component of fitness, a comprehensive fitness model incorporates a broader set of parameters. The table below outlines the key differences:
Table 1: Fitness Model vs. Binding Affinity
| Aspect | Fitness Model | Binding Affinity Measurement |
|---|---|---|
| Scope | Holistic; integrates multiple selective pressures (e.g., infectivity, immune evasion, stability) | Narrow; focuses solely on virus-receptor interaction strength |
| Output | A predictive score for viral variant success and prevalence | A physical binding constant (e.g., KD) |
| Evolutionary Context | Dynamic; considers trade-offs and co-occurrence of mutations in a population | Static; a snapshot of one molecular property |
| Primary Use | Forecasting variant spread, guiding vaccine updates | Informing drug design, understanding entry mechanisms |
Q5: Our experimental evolution in cell culture does not match observations from patient samples. How can we improve our laboratory systems? Traditional monolayer cell cultures often provide an unnaturally permissive environment. To better mimic in vivo conditions, consider:
- Using Advanced Cell Models: Transition to non-tumoral cells, 3D cultures, or organoids. These systems better reflect selective pressures like the innate immune response [23].
- Incorporating Immune Components: Co-culture viruses with immune cells to simulate immune pressure and study immunoediting.
- Validating with Field Data: Constantly contrast findings from laboratory systems with sequencing and clinical data from natural infections to identify discrepancies and refine your models [23].
Troubleshooting Guides
Issue 1: Low Predictive Power in Variant Fitness Models
Problem: Your computational model fails to accurately rank the fitness of emerging viral variants.
Solution: Follow this systematic troubleshooting protocol to identify and rectify the issue.
Table 2: Troubleshooting Low Predictive Power in Fitness Models
| Step | Action | Expected Outcome |
|---|---|---|
| 1. Data Audit | Verify the quantitative data integrated into your model. Are you using only binding affinity (e.g., from docking) and ignoring immune evasion metrics? | A checklist of all parameters in your current model, identifying key gaps. |
| 2. Integrate Immune Evasion | Incorporate a neoantigen fitness cost metric. This measures the immunogenic strength of mutations based on MHC binding and T-cell receptor recognition potential, not just mutation count [24]. | Improved correlation between your model's predictions and observed variant prevalence in epidemiological data. |
| 3. Check for Trade-offs | Analyze if high binding affinity variants show a trade-off with other traits, like reduced viral stability or replication rate. Use multivariate analysis. | Identification of evolutionary constraints that prevent certain high-fitness genotypes from emerging. |
| 4. Validate Experimentally | Synthesize top-predicted variants and test them using pseudotyped virus entry assays in the presence of convalescent sera to measure functional immune escape [14]. | Experimental confirmation of your model's predictions, building confidence in its accuracy. |
Experimental Protocol: Pseudotyped Virus Entry Assay for Variant Validation
This protocol is used to functionally validate the infectivity and immune evasion capabilities of predicted high-risk variants.
- Plasmid Construction: Synthesize genes for viral spike proteins (e.g., SARS-CoV-2 Spike) encoding the wild-type and predicted high-risk variant sequences (e.g., S494P, V503I) [14].
- Virus Production: Co-transfect HEK-293T cells with:
- A spike protein plasmid (wild-type or variant).
- A packaging plasmid (e.g., psPAX2).
- A reporter plasmid (e.g., pLV with luciferase or GFP).
- Harvest and Titration: Collect pseudotyped virus supernatants at 48-72 hours post-transfection. Concentrate and quantify viral titer via p24 ELISA or RT-qPCR.
- Infection Assay: Infect target cells expressing the relevant viral receptor (e.g., A549-ACE2) with normalized amounts of pseudotyped viruses.
- Immune Evasion Test: Pre-incubate viruses with serial dilutions of neutralizing antibodies or convalescent patient serum before adding to cells.
- Quantification: Measure reporter signal (e.g., luciferase activity) 48-72 hours post-infection. Normalized luciferase activity is a proxy for viral entry efficiency. Compare variant entry efficiency and antibody resistance to the wild-type control.
Issue 2: Inconsistent Evolutionary Rates Across Timescales
Problem: The evolutionary rate you infer from recent outbreak data is much higher than the rate calculated from long-term archival sequences, leading to unreliable molecular dating.
Solution: This is a known challenge where short-term rates are systematically higher. Your analysis should account for this time-dependent rate phenomenon.
- Model Selection: Use phylogenetic software (e.g., BEAST2) that allows you to apply relaxed molecular clock models. These models do not assume a constant evolutionary rate across all branches of the phylogenetic tree.
- Incorporate Older Sequences: Integrate data from older isolates, permafrost samples, or archival specimens to calibrate your tree over longer timescales [23].
- Separate Analyses: Clearly state the timescale of your data. Avoid extrapolating a short-term rate to make predictions about long-term evolution.
Issue 3: Computational Strain in Binding Affinity Simulations
Problem: Molecular dynamics (MD) simulations or mutational scanning of viral proteins (like the spike) are computationally expensive and slow, limiting the number of variants you can test.
Solution: Implement a hybrid AI-biophysics pipeline to improve efficiency.
- Initial Coarse Screening: Use a fast, statistical co-occurrence analysis of mutation hotspots in viral sequence databases to identify a shortlist of potentially high-risk variants [14].
- Focused Energetic Analysis: Apply rigorous computational methods only to the shortlisted variants. This includes:
- AI-Powered Prediction: Train a machine learning model on the results from step 2. The model can learn to predict binding affinity and fitness from sequence alone, allowing for rapid screening of millions of virtual variants.
The Scientist's Toolkit: Key Research Reagents & Solutions
Table 3: Essential Resources for Fitness Modeling and Validation
| Research Reagent / Tool | Function / Application |
|---|---|
| EVE-Vax Computational Method [25] | AI-based method for designing viral antigens that foreshadow future immune escape variants for proactive vaccine evaluation. |
| Polymerase Chain Reaction (PCR) & Sequencing Primers | For amplifying and sequencing viral genomes from clinical or environmental samples to track diversity. |
| HEK-293T Cell Line | A standard workhorse cell line for producing pseudotyped viruses for safe viral entry assays. |
| ACE2-Expressing Cell Line (e.g., A549-ACE2) | Target cell line for viruses that use the ACE2 receptor (e.g., SARS-CoV-2); essential for functional entry assays. |
| Luciferase Reporter Gene Plasmid | A standard reporter system packaged into pseudotyped viruses; luminescence upon infection quantifies viral entry efficiency. |
| Convalescent Sera or Monoclonal Antibodies | Used in neutralization assays to quantify the immune evasion capability of a viral variant. |
| Structure Prediction Software (e.g., AlphaFold2) | To generate 3D protein structures for viral variants when experimental structures are unavailable, for use in docking/MD simulations. |
| Molecular Docking Software (e.g., AutoDock Vina) | For initial, rapid in silico screening of binding affinity between viral proteins and host receptors or antibodies. |
| GISAID Database [23] | A global repository of influenza and coronavirus sequence data, essential for tracking real-world viral evolution and validating models. |
A primary challenge in modern virology and pandemic preparedness is the reactive nature of public health responses. By the time a new, high-risk viral variant is detected, it is often too late to adjust public policy or vaccine strategies effectively [9]. The field of viral evolutionary prediction aims to shift this paradigm from reactive tracking to proactive forecasting, allowing scientists to anticipate viral leaps before they threaten public health [9]. This endeavor is fraught with intrinsic challenges, including the non-linear nature of viral evolution, where the effect of one mutation can depend on the presence of others, a phenomenon known as epistasis [9]. Furthermore, the vast mutational space makes it practically impossible to test every possible variant experimentally [9].
Unified deep learning frameworks are emerging as a transformative solution to these challenges. These platforms are designed to handle multiple viruses and predict diverse phenotypic outcomes, such as transmissibility, immune evasion, and host interactions. They leverage artificial intelligence (AI) to integrate genomic, epidemiologic, immunologic, and fundamental biophysical information, creating models that can forecast the course of viral evolution [27] [28]. The core objective is to look at a viral genetic sequence and predict its evolutionary fate and functional consequences, a capability considered the holy grail of pandemic preparedness [28]. This technical support document outlines the specific issues, solutions, and experimental protocols for researchers employing these sophisticated frameworks.
FAQs: Core Concepts for Researchers
FAQ 1: What does "unified" mean in the context of these frameworks, and how does it differ from traditional models? A unified framework is designed to be broadly applicable across multiple viral species, rather than being built for a single specific virus like SARS-CoV-2. While many initial models were developed using COVID-19 data due to its extensive dataset availability, their architectures are intentionally designed for adaptability across RNA viruses [27]. This is achieved by focusing on fundamental biological and physical principles, such as binding affinity to human receptors and antibody evasion potential, which are common constraints shaping the evolution of many viruses [9].
FAQ 2: What types of multi-phenotype predictions can these frameworks perform? These frameworks move beyond single-trait prediction. They can be trained to jointly forecast multiple clinical and biological endpoints critical for risk assessment. For a respiratory virus, this could include simultaneous predictions for:
- Viral Fitness: Including transmissibility and binding affinity to host receptors [9].
- Immune Evasion: The ability to escape neutralizing antibodies from prior infection or vaccination [9] [27].
- Clinical Severity: Associations with patient outcomes such as overall survival or progression-free survival [29]. This multi-endpoint modeling provides a comprehensive profile of a variant's potential threat.
FAQ 3: My data is heterogeneous, combining genomic sequences, protein structures, and clinical outcomes. How can a unified framework handle this? This is a key strength of multimodal deep learning. These frameworks use specialized fusion techniques to integrate diverse data types. For instance, protein language models—AI models trained on millions of protein sequences—can convert raw viral and human protein sequences into meaningful numerical representations that capture evolutionary constraints [30]. These representations can then be combined with other data layers, such as biophysical properties or immune response data, within a single model to improve prediction accuracy for tasks like identifying human-virus protein-protein interactions [30].
FAQ 4: A major challenge is the "black box" nature of AI. How interpretable are these predictions for guiding experimental validation? Interpretability is a critical focus for newer frameworks. While complex models like neural networks can be opaque, there is a significant push towards developing interpretable AI. For example, some frameworks use decision-tree architectures that are powered by machine learning for optimization but result in a clear, visual model that clinicians and researchers can understand [29]. This allows users to see the specific molecular rules the model used to assign a variant to a high-risk category, thereby building trust and providing actionable insights for lab experiments.
Troubleshooting Common Experimental Issues
Problem: Poor Model Generalization to Novel Viruses
- Symptoms: Your model, trained on SARS-CoV-2, performs poorly when making predictions for an unrelated virus like Influenza.
- Solutions:
- Leverage Transfer Learning: Start with a model pre-trained on a broad dataset (e.g., many RNA viruses or general protein sequences) and fine-tune it on a smaller, target-virus-specific dataset [27] [28].
- Incorporate Biophysical Grounding: Ensure your model incorporates fundamental biophysical features (e.g., binding affinity, structural stability) that are universal constraints on viral evolution, rather than relying solely on virus-specific genomic patterns [9].
- Benchmark Rigorously: Use standardized benchmark datasets, like those proposed in systematic reviews, to evaluate your model's performance across different viral contexts and identify specific weaknesses [31].
Problem: Handling Epistasis (Non-Linear Mutation Interactions)
- Symptoms: The model accurately predicts the effect of single mutations but fails when combinations of mutations arise, as their combined effect is non-linear.
- Solutions:
- Choose Architectures that Capture Interactions: Utilize deep learning models like transformers or recurrent neural networks that are inherently designed to model complex, long-range dependencies within sequence data [9] [28].
- Include Epistasis in Training: Explicitly train your model using data that includes paired or multiple mutations, not just single mutants. The VIRAL framework, for instance, overcame this limitation by factoring in these mutational relationships [9].
- Active Learning Cycles: Implement an active learning loop where the model's most uncertain predictions about mutation combinations are prioritized for experimental testing, creating a virtuous cycle of data improvement and model refinement [9].
Problem: Integrating and Managing Multi-Omics Data
- Symptoms: Model performance degrades or becomes unstable when trying to integrate disparate data types (e.g., genomics, transcriptomics, proteomics).
- Solutions:
- Employ Multimodal Fusion Techniques: Adopt a framework specifically designed for multimodal data. These frameworks process each data type through a dedicated sub-model (encoder) and then fuse the representations in a later stage [30] [32].
- Dimensionality Reduction: Apply techniques like PCA or autoencoders to each high-dimensional omics layer before fusion to reduce noise and computational complexity [32].
- Address Data Distribution Shifts: Be aware that different omics data have different scales and distributions. Normalize and preprocess each data type appropriately to avoid having one domain dominate the model's learning process [32].
Experimental Protocols for Key Methodologies
Protocol: Forecasting Variant Dominance Using Biophysical AI
This protocol is based on the approach detailed by Harvard's Shakhnovich lab for forecasting which viral variants are likely to become dominant in populations [9].
1. Principle: Link quantitative biophysical features of viral proteins to viral fitness and use AI to rapidly screen mutational space.
2. Reagents and Equipment:
- Data: Curated sequences of viral variants (e.g., spike protein sequences for SARS-CoV-2) and associated epidemiological data on variant frequency.
- Software: Computational biology tools for predicting protein binding affinity (e.g., molecular docking software) and immune evasion.
- Compute: High-performance computing (HPC) cluster or cloud computing resources for running AI models.
3. Step-by-Step Procedure:
- Step 1: Feature Calculation. For each variant sequence in your training set, compute key biophysical features. These include:
- Binding Affinity: The calculated binding strength between the viral protein (e.g., spike) and the host receptor (e.g., ACE2).
- Structural Stability: The estimated folding stability of the viral protein.
- Antibody Evasion Score: A metric predicting the variant's ability to escape a panel of known neutralizing antibodies.
- Step 2: Model Training. Train a machine learning model (e.g., a gradient boosting machine or neural network) to predict a variant's likelihood of becoming epidemiologically dominant based on the calculated biophysical features. The training label is typically a measure of variant frequency over time.
- Step 3: Incorporate Epistasis. Ensure the model architecture or training data can account for epistasis, where the effect of one mutation depends on other mutations present in the sequence [9].
- Step 4: In-silico Saturation Mutagenesis. Use the trained model to predict the fitness of all possible single-point mutations (and potentially combinations) in the viral protein of interest.
- Step 5: Active Learning Loop. Identify the mutations or variants for which the model is most uncertain. Prioritize these for in vitro experimental validation (e.g., pseudovirus neutralization assays). Feed the experimental results back into the model to retrain and improve its accuracy [9].
4. Analysis and Interpretation:
- The model outputs a ranked list of high-risk mutations/variants.
- Validation: Correlate predictions with future epidemiological data. A successful model will identify high-risk variants before they appear in the population.
The workflow below visualizes this integrated computational and experimental pipeline.
Protocol: Multi-Omics Integration for Host-Pathogen Interaction Prediction
This protocol outlines how to integrate multiple layers of biological data to predict complex phenotypes like host-virus protein-protein interactions (PPIs) or disease resistance mechanisms [30] [32].
1. Principle: Use multimodal deep learning to fuse information from different biological layers (e.g., genome, proteome) for enhanced predictive power.
2. Reagents and Equipment:
- Data Sources:
- Genomics: Viral and host genome sequences.
- Transcriptomics: Host and viral gene expression data post-infection (RNA-seq).
- Proteomics: Data on protein expression or structural information.
- Software: Protein language models (e.g., ESM, ProtBERT), deep learning frameworks (e.g., PyTorch, TensorFlow).
3. Step-by-Step Procedure:
- Step 1: Data Encoding.
- Genomic/Protein Sequences: Process them through a protein language model to generate numerical feature embeddings that capture evolutionary and structural information [30].
- Transcriptomic/Proteomic Data: Normalize and preprocess into feature vectors.
- Step 2: Multimodal Fusion.
- Pass each data type through its own dedicated neural network encoder.
- Fuse the resulting representations from each modality into a unified feature vector. This can be done via simple concatenation or more sophisticated attention-based mechanisms [30].
- Step 3: Model Training.
- Feed the fused representation into a final prediction layer (a neural network) to predict the target phenotype (e.g., PPI probability, resistance score).
- Train the entire model end-to-end using known positive and negative examples.
- Step 4: Interpretation.
- Use model interpretation techniques (e.g., attention weights, SHAP values) to determine which data modalities and specific features were most important for the prediction.
4. Analysis and Interpretation:
- The model outputs a prediction score (e.g., likelihood of interaction).
- Validation: Compare predictions against a held-out test set of known interactions from databases or new experimental results (e.g., yeast-two-hybrid).
The following diagram illustrates the flow of data through this multimodal architecture.
The Scientist's Toolkit: Key Research Reagent Solutions
The following table details essential reagents and tools referenced in the experimental protocols and literature for developing and applying unified deep learning frameworks.
| Item | Function in Framework | Example Application |
|---|---|---|
| Protein Language Models (e.g., ESM) | Converts raw protein sequences into numerical embeddings that capture structural and evolutionary information. [30] | Feature extraction for viral spike proteins and human receptors in host-pathogen interaction prediction. [30] |
| Lyophilization-Ready Master Mixes | Provides room-temperature stable reagents for qPCR/LAMP assays, simplifying assay development and storage. [33] | Development of multiplex molecular assays for detecting and differentiating emerging respiratory viruses. [33] |
| High-Sensitivity Paired Antibodies | Key components for developing rapid immunoassays (e.g., lateral flow tests) with high specificity and low cross-reactivity. [33] | Creating point-of-care diagnostic tests for specific viral antigens or host response biomarkers. [33] |
| Ambient-Temperature NGS Kits | Simplifies sample preparation for next-generation sequencing by eliminating cold-chain logistics. [33] | Genomic surveillance of circulating viral variants in resource-limited settings for model training data. [33] |
| Gene Synthesis Services | Provides custom, high-quality synthetic DNA sequences for testing specific genetic designs in vitro. [34] | Synthesizing and testing de novo designed viral capsid sequences for gene therapy or vaccine development. [34] |
Quantitative Framework Performance Benchmarks
To select the appropriate tool, researchers must compare the demonstrated performance of different approaches. The table below summarizes key quantitative results from recent studies.
| Framework / Model Name | Primary Task | Key Performance Metric | Result | Context & Notes |
|---|---|---|---|---|
| VIRAL Framework [9] | Identification of high-risk SARS-CoV-2 variants | Acceleration factor vs. conventional screening | >5x faster | Identifies variants ahead of epidemiological signals; requires <1% of experimental screening effort. |
| MuTATE [29] | Molecular subtyping for cancer risk stratification | Reclassification rate in patient risk groups | 13-72% | Reclassified patients across three cancer types (LGG, EC, GA), improving risk stratification. |
| Systematic Benchmark [31] | Virus-host prediction (27 tools) | Generalizability across contexts | Variable | No single tool was universally optimal; performance highly dependent on specific use case and dataset. |
| DeepHVI [30] | Human-Virus Protein-Protein Interaction (PPI) prediction | Accuracy of PPI prediction | Improved (vs. baseline) | Uses multimodal deep learning and protein language models; specific accuracy values not provided in results. |
For researchers and drug development professionals, the relentless evolution of viruses presents a fundamental challenge: how to design effective vaccines against a rapidly moving target. The high mutation rates of viruses, particularly RNA viruses, and the complex epistatic interactions within their genomes create a fitness landscape that is difficult to map and predict [23] [35]. This evolutionary arms race often results in viral variants that can evade both natural and vaccine-induced immunity, rendering existing countermeasures less effective [36]. The core challenge lies in shifting from a reactive posture—responding to variants after they have already emerged and spread—to a proactive one, where we anticipate viral evolutionary paths and design vaccines accordingly. Computational tools are now emerging to make this proactive antigen design a tangible reality, offering a pathway to future-proof vaccines against not-yet-prevalent viral variants.
Computational Tools for Proactive Design: FAQs and Troubleshooting
This section addresses specific, technical issues you might encounter when implementing computational approaches for proactive vaccine design.
FAQ 1: How can we computationally identify which viral mutations are most likely to lead to immune escape?
The Problem: The number of possible mutations in a viral genome is astronomically large. Experimentally testing every single-point mutation and combination for immune escape is not feasible.
The Solution: Leverage deep learning models trained on evolutionary sequence data.
- Tool Example: Language Models for Viral Evolution. These models, inspired by natural language processing, are trained on thousands of viral protein sequences. They learn the underlying "grammar" and "syntax" of functional viral proteins, allowing them to distinguish between mutations that are likely to occur and maintain fitness versus those that are not [36].
- Experimental Validation Protocol: To validate predictions from such a model:
- Select Predicted Mutations: Choose a subset of high-scoring escape mutations predicted by the model.
- Generate Pseudoviruses: Create pseudoviruses incorporating the selected mutations into the viral protein of interest (e.g., SARS-CoV-2 Spike protein) using site-directed mutagenesis.
- Perform Neutralization Assays: Incubate the pseudoviruses with sera from vaccinated individuals or convalescent patients.
- Quantify Escape: Use luciferase-based assay systems (e.g., Steady-Glo or Bright-Glo) to measure the reduction in neutralization compared to the wild-type virus. A significant reduction in luminescence signal indicates successful immune escape [37].
Troubleshooting Guide:
- Issue: Model predictions have a high false-positive rate (predicted escape mutations do not function in the lab).
- Potential Cause: The training dataset may be biased or lack sufficient diversity.
- Solution: Fine-tune the model on a more curated dataset specific to the virus family of interest, incorporating known structural and functional constraints.
- Issue: Combined mutations are not functional in pseudovirus assays.
- Potential Cause: The model may not fully account for epistasis (where the effect of one mutation depends on the presence of others).
- Solution: Implement or use models that explicitly factor in epistatic interactions, such as the biophysical model used in the EVE-Vax platform, which integrates binding affinity and antibody accessibility constraints [9] [37].
FAQ 2: Our goal is to design a single vaccine antigen that protects against future variants. What computational strategy should we use?
The Problem: Designing a single antigen that can elicit a broad immune response against both existing and future viral diversity.
The Solution: Use computational frameworks to design "mosaic" or "consensus" antigens that incorporate features from multiple potential variants.
- Tool Example: EVE-Vax Platform. This platform combines three key biological constraints—viral fitness, antibody accessibility, and structural dissimilarity—to computationally design synthetic spike proteins that mimic potential future immune escape variants [37].
- Experimental Validation Protocol: To test a computationally designed mosaic antigen:
- Antigen Construction: Synthesize the gene for the designed antigen and clone it into your preferred vaccine platform (e.g., mRNA, nanoparticle, viral vector).
- Animal Immunization: Immunize animal models (e.g., mice or non-human primates) with the candidate vaccine.
- Sera Collection and Titration: Collect immune sera and measure total antigen-specific IgG titers using ELISA to confirm immunogenicity.
- Broad Neutralization Assessment: Test the sera for its ability to neutralize a panel of pseudoviruses. This panel should include:
- Current circulating variants.
- Historical variants of concern.
- Computationally designed future variants (like those from EVE-Vax).
- Analysis: A successful broad-spectrum vaccine will show high neutralization titers across a wide range of variants in the panel, outperforming vaccines based only on a single, current sequence [37].
Troubleshooting Guide:
- Issue: The mosaic antigen is less immunogenic than the wild-type antigen.
- Potential Cause: The computational design may have over-optimized for breadth at the cost of immunogenicity.
- Solution: Re-run the design algorithm with adjusted weights, placing a higher penalty on mutations that are predicted to significantly disrupt protein folding or T-cell epitopes.
- Issue: The vaccine does not elicit protection against specific, high-risk future variants.
- Potential Cause: The variant panel used for in silico design did not adequately represent certain evolutionary paths.
- Solution: Expand the variant panel by incorporating predictions from multiple computational models, including those based on coordinated substitution networks [38].
FAQ 3: How can we detect the next variant of concern earlier from genomic surveillance data?
The Problem: Traditional phylogenetic methods detect variants of concern only after they have reached a certain prevalence, costing valuable response time.
The Solution: Shift from tracking single mutations to identifying emerging haplotypes (combinations of mutations) using network analysis.
- Tool Example: HELEN (Heralding Emerging Lineages in Epistatic Networks). This framework analyzes "coordinated substitution networks" of the viral genome. Instead of waiting for a specific haplotype to become common, it looks for dense communities within this network—groups of mutations that are statistically linked and appear together more often than expected by chance. The emergence of these dense communities signals a nascent, fit haplotype long before it becomes prevalent [38].
- Experimental Workflow Protocol:
- Data Stream: Establish a pipeline to continuously ingest and pre-process new viral genome sequences from public databases (e.g., GISAID).
- Network Construction: For each time window (e.g., weekly), compute the coordinated substitution network for the gene of interest (e.g., Spike protein).
- Community Detection: Apply graph theory algorithms to identify densely connected communities within the network.
- Variant Inference: Reconstruct the viral haplotypes associated with the densest communities.
- Prioritization & Alert: Flag these inferred haplotypes for immediate experimental characterization (see FAQ 1's validation protocol) and notify relevant public health and research bodies [38].
Troubleshooting Guide:
- Issue: The system generates too many false-positive alerts.
- Potential Cause: The threshold for defining a "dense" community may be too low, or the sequencing data may be noisy.
- Solution: Increase the density threshold and implement more stringent sequence quality control filters. Validate the method retrospectively on historical data to optimize parameters.
- Issue: The computational cost is too high for real-time analysis.
- Potential Cause: Analyzing millions of sequences with traditional phylogenetics is computationally expensive.
- Solution: The HELEN framework's complexity depends on genome length, not the number of sequences, making it more scalable. Ensure you are using this or a similarly optimized method [38].
Key Computational Tools and Their Applications
The following table summarizes the core computational tools and approaches discussed, highlighting their primary function and the challenge they address.
Table 1: Computational Tools for Proactive Antigen Design and Variant Prediction
| Tool / Approach | Primary Function | Key Challenge Addressed |
|---|---|---|
| AI-Driven Epitope Prediction [39] | Uses CNNs, RNNs, and GNNs to predict B-cell and T-cell epitopes with high accuracy from protein sequences or structures. | Rapid identification of conserved, immunogenic targets that are less likely to mutate. |
| Variant Forecasting Models [9] | Combines biophysics and AI to quantitatively link mutations to viral fitness and immune evasion, factoring in epistasis. | Predicting which specific viral variants are most likely to become dominant in the future. |
| EVE-Vax Platform [37] | Computationally designs synthetic viral proteins that mimic not-yet-seen immune escape variants. | Proactive testing of vaccine efficacy against future variants and guiding broad-spectrum antigen design. |
| HELEN Framework [38] | Detects emerging viral haplotypes by analyzing community structures in coordinated substitution networks. | Early detection of potential Variants of Concern (VOCs) from genomic data, before they become prevalent. |
| Language Models [36] | Learns the "grammar" of viral proteins to predict mutations that maintain viral fitness and function. | Filtering the vast universe of possible mutations to identify those that are evolutionarily plausible. |
Essential Research Reagent Solutions for Experimental Validation
Computational predictions are only as good as their experimental validation. Below is a toolkit of key reagents and their functions for testing computationally designed antigens and predicted variants.
Table 2: Key Research Reagents for Validating Proactive Vaccine Designs
| Research Reagent | Function in Validation Experiments |
|---|---|
| Pseudovirus Systems | Safely model viral entry for pathogens requiring high containment (e.g., SARS-CoV-2, HIV). Used in neutralization assays. |
| Luciferase Assay Kits (e.g., Bright-Glo, Steady-Glo) | Provide a highly sensitive, quantitative readout for pseudovirus-based neutralization assays by measuring luminescence [37]. |
| Convalescent Sera / Vaccinated Sera | Contain the polyclonal antibody response from natural infection or vaccination. The gold standard for testing immune escape in vitro. |
| Monoclonal Antibodies (mAbs) | Act as precise tools for mapping the specific antigenic sites targeted by the immune system and for testing escape from therapeutics. |
| Programmable Gene Synthesis | Enables the rapid and accurate construction of genes encoding computationally designed antigen variants for lab testing. |
| Adjuvants (e.g., Alhydrogel, MF59) | Enhance the immune response to vaccine antigens in pre-clinical animal models, crucial for testing the immunogenicity of novel designs [40]. |
Workflow Visualization for Proactive Vaccine Design
The following diagram illustrates a comprehensive, integrated workflow for proactive antigen design, combining computational prediction with experimental validation.
Integrated Workflow for Proactive Vaccine Design
The convergence of advanced computational tools and high-throughput experimental biology is forging a new paradigm in vaccinology. By leveraging AI-driven prediction, structural modeling, and genomic surveillance, researchers can now move beyond reactive strategies. The FAQs, protocols, and resources provided here offer a practical framework for tackling the inherent challenges in evolutionary prediction. The ultimate goal is clear: to design resilient, "future-proof" vaccines that can withstand the pressure of viral evolution and protect global health against emerging threats.
Bridging the Gaps: Data Scarcity, Model Generalization, and Real-World Deployment
Technical Support Center: FAQs & Troubleshooting Guides
This technical support center provides practical solutions for researchers confronting data scarcity in viral evolutionary prediction. The following FAQs and troubleshooting guides address common experimental and computational challenges in this field.
Frequently Asked Questions (FAQs)
1. Our lab is new to genomic surveillance. What are the main bottlenecks in implementing a WGS pipeline for antimicrobial resistance (AMR) surveillance, and how can we overcome them?
Implementing whole genome sequencing (WGS) presents several key bottlenecks, primarily in bioinformatics and data integration [41].
- Data Integration Bottleneck: Sample metadata and antimicrobial sensitivity testing (AST) results often arrive in disparate, non-standardized formats, making integration with genomic data a manual, error-prone process [41].
- Solution: Implement automated data parsing pipelines. Tools like Data-flo allow you to build visual dataflows that transform different file formats (e.g., from VITEK systems) into consistent, usable formats for analysis, which can then be run by staff without command-line expertise [41].
- Sequence Analysis Bottleneck: The computational process of turning raw sequence data into interpretable results requires specialized training, software, and computing infrastructure [41].
- Solution: Use workflow managers like Nextflow combined with containerization technologies (Docker or Singularity). This approach packages software dependencies into reproducible, scalable pipelines that can run on everything from high-spec laptops to computing clusters, standardizing analyses and minimizing hands-on time [41].
2. We are struggling with low viral titers in clinical samples, which leads to poor genome coverage. What approaches can improve sequence data quality from sparse samples?
This is a common challenge in pathogen agnostic sequencing, often described as a "needle in a haystack" problem [42].
- Optimize Sample Preparation: Move beyond strict metagenomic methods. Integrate optimization steps for host depletion or viral pathogen enrichment to increase the relative abundance of target genetic material before sequencing [42].
- Leverage Pan-Viral Methods: In early outbreak responses, before specific assays are available, consider using pan-viral sequencing methods or random-priming approaches. These can be more effective at capturing novel or divergent pathogens than targeted tests that may fail due to mismatched primers [42].
- Utilize Complementary Surveillance: For community-level monitoring, Wastewater-Based Epidemiology (WBE) can be a powerful tool. It provides a pooled sample that can yield vital data on circulating viral pathogens, even when individual clinical samples are sparse [43].
3. How can we better predict which viral variants pose the highest public health risk, especially when experimental validation is resource-intensive?
Predicting high-risk variants is a central challenge. New computational frameworks are being developed to prioritize lab efforts.
- Combine Biophysics with AI: A promising approach is to use models that quantitatively link biophysical features (e.g., spike protein binding affinity, antibody evasion potential) to a variant's likelihood of surging in the population. Incorporating epistasis (where the effect of one mutation depends on others) is critical for accuracy [9].
- Implement Active Learning Frameworks: Frameworks like VIRAL (Viral Identification via Rapid Active Learning) use AI to identify the mutations most likely to enhance transmissibility and immune escape. This focuses experimental screening on the most concerning candidates, dramatically accelerating validation. Simulations show VIRAL can identify high-risk SARS-CoV-2 variants up to five times faster than conventional approaches, using less than 1% of the experimental screening effort [9].
4. What are the common operational challenges when setting up a pathogen agnostic sequencing program, and how can they be mitigated?
Operationalizing pathogen agnostic sequencing within a surveillance system involves several non-technical hurdles [42].
- Challenge: Staffing and Training. Recruiting and retaining highly trained molecular epidemiologists and bioinformaticians is difficult, especially in resource-constrained areas [42].
- Mitigation: Invest in continuous learning and clear career advancement opportunities. Establish consortiums with other labs to share training modules and standardize practices, fostering a collaborative environment that helps retain talent [42].
- Challenge: Lack of Community Standards. Rapidly advancing technologies and a lack of standardized methods can make it hard to reproduce results [42].
- Mitigation: Participate in proficiency testing exercises. These initiatives, like the Pathogen Discovery Project 1.0 run by the DOD's GEIS program, allow labs to benchmark their agnostic sequencing protocols against a blinded panel of pathogens and identify areas for improvement [42].
- Challenge: Data-Sharing Agreements and Policy Gaps. Establishing agreements with partner laboratories and host nations, and developing policies for using sequencing results for public health action, can be a significant barrier [42].
- Mitigation: Proactively engage with legal, ethical, and public health policy experts early in the program planning process to draft and negotiate these agreements.
Troubleshooting Guides for Common Experimental Issues
Issue: Inconsistent bioinformatics results when analyzing WGS data for AMR markers.
- Problem: Different software versions or database builds yield conflicting predictions.
- Solution: Containerize your analysis environment.
- Step 1: Use a workflow manager like Nextflow to define your analysis steps (e.g., quality control, assembly, AMR gene calling) [41].
- Step 2: Package all software dependencies (specific versions of tools like ARIBA, AMRFinderPlus, etc.) into a Docker or Singularity container [41].
- Step 3: Execute the Nextflow workflow, which calls the software from within the container. This ensures the analysis is fully reproducible across different machines and over time, eliminating "works on my machine" problems [41].
Issue: Failure to detect a known pathogen in a complex clinical sample using metagenomic sequencing.
- Problem: The pathogen signal is too low compared to host and other microbial background.
- Solution: Implement a host depletion and/or target enrichment strategy.
- Step 1 (Host Depletion): Use probes to remove abundant host (e.g., human) RNA/DNA during library preparation. This increases the proportion of microbial reads in the sequence library [42].
- Step 2 (Target Enrichment): If a specific pathogen type is suspected (e.g., viruses), use pan-family PCR primers or viral enrichment kits to selectively amplify viral sequences prior to sequencing [42].
- Step 3: Proceed with standard metagenomic sequencing. The pre-processing steps significantly improve the probability of detecting the "needle in the haystack" [42].
Issue: Difficulty in functionally characterizing the large number of potential spike protein mutations.
- Problem: Experimental screening of every possible mutation for immune evasion and ACE2 binding is impractical.
- Solution: Use a computational framework to prioritize mutants for experimental testing.
- Step 1: Leverage a biophysics-informed AI model, like the one described in the VIRAL framework, to analyze potential spike protein mutations [9].
- Step 2: The model will rank mutations based on their predicted likelihood to enhance viral fitness through improved receptor binding or immune escape.
- Step 3: Focus your lab's experimental resources (e.g., pseudovirus neutralization assays) on characterizing the top-ranked, highest-risk candidates, thereby accelerating the validation process [9].
The tables below summarize key quantitative information from recent studies to aid in experimental planning and benchmarking.
Table 1: Key Metrics from the GHRU WGS Implementation Project
| Metric | Value | Context / Significance |
|---|---|---|
| Genomes Processed | 5,979 | Total across GHRU partners in Colombia, India, Nigeria, and the Philippines [41]. |
| Pathogen Priority | WHO Priority AMR species | Focus on species requiring priority research for antimicrobial resistance [41]. |
| Computational Setup | High-spec laptops or workstations | Minimal hardware requirement when using efficient, containerized workflows [41]. |
| Core Technologies | Nextflow, Docker/Singularity, Data-flo | Workflow manager, containerization, and data parsing tools used to overcome bottlenecks [41]. |
Table 2: Performance of Predictive Frameworks for Viral Variants
| Framework / Model | Key Input Features | Reported Performance / Outcome |
|---|---|---|
| Biophysics + Epistasis Model [9] | Spike protein binding affinity, antibody evasion, epistatic interactions | Forecasts emergence of dominant variants ahead of epidemiological signals [9]. |
| VIRAL Framework [9] | AI analysis of potential spike mutations combined with biophysical model | Identifies high-risk SARS-CoV-2 variants 5x faster, using <1% of experimental screening effort [9]. |
| AI "Virtual Lab" [44] | AI agents with expertise in immunology, computational biology, and machine learning | Designed a novel nanobody-based COVID-19 vaccine candidate in a few days; nanobody showed strong binding to variants [44]. |
Experimental Protocols
Protocol 1: Standardized Bioinformatics Pipeline for Bacterial WGS Analysis
This protocol outlines a reproducible method for processing raw bacterial sequencing reads to determine AMR markers and sequence type, based on the GHRU implementation [41].
- Quality Control: Use a tool like
FastQCto assess the quality of the raw sequencing reads. - Genome Assembly: Perform de novo assembly of the reads into contiguous sequences (contigs) using an assembler like
SPAdes. - Species Identification (Optional): Confirm species using
kmerFinderor a similar tool. - Antimicrobial Resistance Gene Detection: Screen the assembly against curated AMR databases (e.g., NCBI's AMRFinderPlus, CARD) to identify known resistance determinants.
- Multi-Locus Sequence Typing (MLST): Determine the sequence type (ST) by comparing assembled sequences to pubMLST.org schemes.
- Phylogenetic Analysis (for multiple samples): Generate a single-nucleotide polymorphism (SNP) phylogeny using a mapping-based approach (e.g., Snippy) to understand transmission patterns.
All steps are executed within a single Nextflow workflow, with each software tool running from a pre-built Docker/Singularity container to ensure version control and reproducibility [41].
Protocol 2: Pathogen Agnostic Sequencing for Clinical Metagenomics
This protocol is derived from lessons learned in the DOD's GEIS program for handling pathogen-negative samples from surveillance activities [42].
- Sample Selection: Prioritize samples from routine surveillance (e.g., acute respiratory or febrile illness) that tested negative using traditional, targeted diagnostics [42].
- Nucleic Acid Extraction: Perform total nucleic acid extraction (DNA and RNA) from the clinical sample.
- Host Depletion: Treat the extract with a commercial host depletion kit to remove human genetic material, thereby enriching for microbial content [42].
- Library Preparation & Sequencing: Prepare a sequencing library using a metagenomic (shotgun) approach. For RNA viruses, a reverse transcription step is included. Sequence on an NGS platform (e.g., Illumina MiSeq) [42].
- Bioinformatic Analysis:
- Quality Control & Host Read Removal: Trim reads for quality and align to a human reference genome to remove any remaining host reads.
- Taxonomic Classification: Use a classifier (e.g., Kraken2, Centrifuge) to assign reads to taxonomic groups.
- Pathogen Identification: A pathogen is suggested if a significant number of reads map to a known pathogen genome, with coverage across multiple genes.
- Confirmation: Crucially, findings from the agnostic method should be confirmed using a targeted assay (e.g., specific PCR) if possible, to rule out false positives [42].
Visualization of Key Processes and Workflows
The following diagrams illustrate critical workflows and relationships described in the technical support guides.
Data Integration Workflow for Genomic Surveillance
AI Virtual Lab Structure for Accelerated Research
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Tools and Resources for Viral Evolutionary Prediction
| Tool / Resource | Type | Primary Function |
|---|---|---|
| Nextflow [41] | Workflow Manager | Orchestrates complex bioinformatics pipelines, allowing for scalability and reproducibility on different computing infrastructures. |
| Docker / Singularity [41] | Containerization Platform | Packages software, dependencies, and environment into a single, portable unit, eliminating installation conflicts and ensuring reproducible results. |
| Data-flo [41] | Data Parsing Tool | Provides a visual interface to build and share dataflows for cleaning, transforming, and integrating disparate metadata and experimental results. |
| GISAID [45] | Database | Critical international database for sharing influenza and SARS-CoV-2 virus sequences, essential for tracking global variant evolution. |
| AlphaFold [44] | AI Protein Structure Tool | Used by AI "virtual scientists" and researchers to predict the 3D structure of viral proteins (e.g., spike) and designed countermeasures (e.g., nanobodies). |
| VIRAL Framework [9] | AI Predictive Model | Combines biophysical modeling with active learning to prioritize high-risk viral variants for experimental validation, optimizing resource use. |
| Wastewater-Based Epidemiology (WBE) [43] | Surveillance Method | Provides community-level, unbiased data on pathogen circulation, acting as an early warning system and overcoming limitations of sparse clinical sampling. |
The evolutionary prediction of future viral variants is a central challenge in modern immunology and drug development. While much effort is focused on antibody escape mutations, this framework neglects a crucial component: T-cell immunity. Antibodies primarily target a limited number of surface proteins, creating strong selective pressure for mutations in these regions. In contrast, T cells recognize a broader array of viral peptides presented by MHC molecules, including highly conserved internal proteins, making this response more resilient to viral evolution [46]. The over-reliance on antibody-centric models has created critical gaps in our ability to predict viral evolution and design durable interventions.
This technical support center addresses the methodological challenges in studying T-cell responses to viral variants. The guidance below provides standardized protocols and troubleshooting for assays that quantify T-cell immunity, enabling researchers to generate comparable data across laboratories and ultimately improve predictive models of viral evolution.
Technical Support Center
Troubleshooting Guides
Guide 1: Low or No Antigen-Specific T-cell Response in ELISpot/Intracellular Cytokine Staining
Problem: Unexpectedly low or absent T-cell response upon antigen stimulation in assays measuring cytokine production (e.g., ELISpot, ICS).
Questions for Diagnosis:
- Has the antigen preparation been validated? (Check concentration, sterility, and endotoxin levels.)
- What is the viability and count of the PBMCs used? (Should be >90% viability.)
- Are the positive controls (e.g., SEB, CEF peptide pool) yielding expected results?
- For viral variants: Is the antigen sequence correctly synthesized and does it contain the expected epitopes for your model system?
Solutions:
- Antigen Preparation: Titrate the antigen concentration. Use a range from 0.1-10 µg/mL for peptides or 0.1-5.0 µg/mL for recombinant proteins. Include a known positive antigen control (e.g., CEF pool) to validate the entire assay system [47].
- PBMC Quality: Ensure cryopreserved PBMCs are thawed rapidly and rested for 4-6 hours in complete media at 37°C before stimulation. Check viability using trypan blue or an automated cell counter.
- Positive Control Failure: If mitogen (e.g., SEB) controls fail, the issue likely lies with cell health or general detection reagents. If the CEF pool fails but SEB works, the issue may be specific to the MHC-peptide presentation or the immunodominance of the response.
- Variant Epitopes: For variant studies, confirm that the variant peptides used for stimulation contain the mutations of interest and are synthesized at >80% purity. Cross-reference with immune epitope databases (IEDB) to ensure targeted epitopes are relevant.
Guide 2: High Background Noise in T-cell Assays
Problem: Excessive background signal in negative controls (e.g., cells alone or unstimulated), making specific response interpretation difficult.
Questions for Diagnosis:
- Are the assay plates/wash steps performed thoroughly?
- Was the cell culture contaminated?
- Are the antibodies titrated and specific?
Solutions:
- Wash Steps: Increase the number and volume of washes. For ELISpot, use PBS with 0.05% Tween-20. For ICS, ensure permeabilization wash buffers are freshly prepared.
- Cell Contamination: Perform sterility checks on media and reagents. Use antibiotics (e.g., Penicillin-Streptomycin) in culture media if contamination is confirmed as the source.
- Antibody Titration: Titrate all detection antibodies. For ICS, use a viability dye to gate out dead cells that non-specifically bind antibodies. Fc receptor blocking reagents can be added before surface staining to reduce non-specific antibody binding.
Guide 3: Poor Cell Recovery or Viability Post-Stimulation
Problem: Low cell numbers or poor viability after the antigen stimulation period, preventing accurate analysis.
Questions for Diagnosis:
- What is the antigen toxicity profile?
- Is the cell culture condition (CO₂, temperature, humidity) optimal?
- Was the stimulation time too long?
Solutions:
- Antigen Toxicity: Test antigen toxicity by culturing PBMCs with a range of antigen concentrations and measuring viability after 12-24 hours. Reduce stimulation time (e.g., from 18h to 6h for early activation markers) or antigen concentration.
- Culture Conditions: Ensure incubators are calibrated to 37°C, 5% CO₂, and >90% humidity. Use culture plates with lids designed for gas exchange.
- Stimulation Duration: For assays measuring cytotoxicity or requiring high viability post-culture, reduce stimulation time and supplement media with low-dose IL-2 (e.g., 10-50 IU/mL) to support T-cell survival.
Frequently Asked Questions (FAQs)
FAQ 1: Why should T-cell immunity be a primary consideration in evolutionary prediction models for viral variants?
Antibodies exert immense selective pressure on viral surface proteins like Spike, readily driving escape mutations. In contrast, T cells target a broader set of viral proteins, including highly conserved internal proteins. This makes T-cell responses more resilient to viral evolution. Studies of SARS-CoV-2 variants have demonstrated that while antibody neutralization can be significantly evaded, T-cell responses, particularly CD8+ T cells, cross-recognize variants due to the conservation of their target epitopes [46]. Incorporating T-cell targeting into models allows for a more complete prediction of viral evolutionary pathways.
FAQ 2: What are the key quantitative differences between CD4+ and CD8+ T-cell responses to viral variants?
Table: Key Quantitative Differences in T-cell Responses to Viral Variants
| Parameter | CD4+ T Cells | CD8+ T Cells |
|---|---|---|
| Cross-reactivity to Omicron BA.4/BA.5 | Significantly reduced reactivity compared to ancestral strain [47] | Higher degree of cross-reactivity maintained |
| Polyfunctionality Boost | Enhanced by booster vaccination (increased IFN-γ, IL-2, TNF-α) [47] | Less affected by booster vaccination; remains less polyfunctional [47] |
| Response Onset | Detectable ~7 days post-vaccination [47] | Detectable ~7 days post-vaccination [47] |
| Typical Readout | Intracellular cytokine staining (IFN-γ, TNF-α, IL-2) | Intracellular cytokine staining (IFN-γ, TNF), CD107a degranulation assay [46] |
FAQ 3: How do "stem-like" T cells impact long-term immunity against evolving viruses?
Stem-like T cells (TCF1+), recently identified in the CD4+ compartment, are antigen-primed but less differentiated. They act as a long-lived reservoir that can self-renew and continuously replenish short-lived effector cells, sustaining immune responses during chronic infections and upon re-exposure to variants [48]. This population is critical for the durability and adaptability of T-cell immunity, as their persistence ensures a base level of protection that can be rapidly mobilized against new viral variants, even when those variants have evaded antibody responses.
FAQ 4: What is a critical pitfall in interpreting PD-1 expression on virus-specific T cells?
The expression of PD-1 on antigen-specific T cells is often interpreted as a sign of "exhaustion." However, in acute SARS-CoV-2 infection, PD-1 is expressed on virus-specific CD8+ T cells as a marker of recent activation, not exhaustion. These PD-1+ cells during acute infection are highly functional, producing effector molecules like IFN-γ, TNF, and CD107a [46]. Misinterpreting PD-1 in this context could lead to the incorrect conclusion that the T-cell response is dysfunctional when it is, in fact, robustly active.
Experimental Protocols for Key T-cell Assays
Protocol: Intracellular Cytokine Staining (ICS) for Assessing Cross-Reactivity to Viral Variants
Application: This protocol is used to quantify and characterize antigen-specific CD4+ and CD8+ T-cell responses, and to assess the cross-reactivity of these responses to different viral variant peptides.
Principle: PBMCs are stimulated with viral peptides. Secretion of cytokines is blocked, causing them to accumulate intracellularly. Cells are then stained for surface markers, fixed, permeabilized, and stained internally for cytokines, allowing for the identification and phenotyping of antigen-responsive T cells.
Reagents:
- Peptide pools (ancestral strain and variant strains, e.g., Omicron BA.4/BA.5)
- RPMI-1640 complete media
- Protein Transport Inhibitor (e.g., Brefeldin A)
- Anti-CD3, anti-CD4, anti-CD8 antibodies
- Anti-cytokine antibodies (e.g., anti-IFN-γ, anti-TNF-α, anti-IL-2)
- Permeabilization/Wash Buffer
- Flow cytometer
Procedure:
- PBMC Preparation: Thaw cryopreserved PBMCs and rest for 4-6 hours in complete media at 37°C. Count and assess viability (>90% is critical).
- Stimulation: Seed 1-2 x 10^6 PBMCs per well in a 96-well U-bottom plate. Add:
- Test Wells: Peptide pools (e.g., 1-2 µg/mL per peptide).
- Positive Control: Staphylococcal Enterotoxin B (SEB, 1 µg/mL) or PMA/Ionomycin.
- Negative Control: DMSO (peptide solvent) or media alone.
- Inhibit Cytokine Secretion: Add Brefeldin A (1:1000 dilution) to all wells after 1-2 hours of stimulation.
- Incubate: Incubate plates for a total of 18 hours (or 6 hours for early activation markers) at 37°C, 5% CO₂.
- Surface Staining: Transfer cells to FACS tubes, wash with PBS, and stain with surface antibody cocktails (e.g., anti-CD3, CD4, CD8) for 20-30 minutes at 4°C in the dark.
- Fixation and Permeabilization: Wash cells, then resuspend in Fixation/Permeabilization buffer for 20 minutes at 4°C in the dark.
- Intracellular Staining: Wash cells with Permeabilization/Wash Buffer, then stain with intracellular antibody cocktails (e.g., anti-IFN-γ, TNF-α) for 30 minutes at 4°C in the dark.
- Acquisition: Wash cells and resuspend in PBS. Acquire data on a flow cytometer, collecting at least 100,000 events in the lymphocyte gate.
Technical Notes:
- Always include a fluorescence-minus-one (FMO) control for accurate gating.
- The activation profile of SARS-CoV-2-specific CD8+ T cells includes high expression of CD38, CD69, or PD-1 without functional exhaustion [46].
- For variant cross-reactivity studies, ensure the peptide pools for different variants are matched in concentration and composition aside from the defining mutations.
Protocol: Phenotyping Stem-like CD4+ T Cells (TCF1+)
Application: To identify and characterize the population of stem-like CD4+ T cells, which are crucial for long-term immune persistence and are defined by the expression of TCF1.
Principle: This protocol uses multicolor flow cytometry to detect the transcription factor TCF1 (encoded by the TCF7 gene) intracellularly, combined with surface markers to define the stem-like T cell population.
Reagents:
- Anti-CD3, anti-CD4, anti-CD45RA, anti-CCR7, anti-CD95, anti-PD-1 antibodies
- Anti-TCF1/TCF7 antibody
- Foxp3/Transcription Factor Staining Buffer Set
- Permeabilization buffer
Procedure:
- Surface Staining: Isolate and stain PBMCs with surface antibody cocktails for 30 minutes at 4°C in the dark. Include markers like CD45RA and CCR7 to define naive and central memory subsets, and CD95 to exclude naive cells (CD45RA+CCR7+CD95-).
- Fixation and Permeabilization: Use a specialized Foxp3/Transcription Factor buffer set for optimal intracellular staining of nuclear antigens like TCF1. Fix and permeabilize cells according to the kit instructions.
- Intracellular Staining: Stain cells with anti-TCF1 antibody for 30-60 minutes at 4°C in the dark.
- Acquisition and Analysis: Acquire data on a flow cytometer. The stem-like population is often identified as TCF1+ within the CD4+ T cell compartment, typically residing in the CD45RA-CCR7+/- (central/effector memory) and PD-1+ fraction [48].
Technical Notes:
- Transcription factor staining requires rigorous permeabilization. Commercial kits are recommended.
- The identification of stem-like CD4+ T cells is an evolving field. Co-staining with other markers like CXCR5 may be incorporated for further subset definition.
Data Presentation: Quantitative Insights
Table: SARS-CoV-2 Specific CD8+ T-Cell Response Kinetics and Characteristics [46]
| Characteristic | Metric / Observation | Experimental Context |
|---|---|---|
| Response Onset | Peak as early as 1 week post-infection | Acute SARS-CoV-2 infection |
| Population Half-life | ~200 days | Post-acute phase / Memory |
| Immunodominance | Targets median of 17 epitopes per individual; immunodominant toward nucleo- and membrane proteins | Broad specificity analysis |
| Phenotype (Acute) | CD38+ CD69+ PD-1+ (activation, not exhaustion) | Functional profiling during viremia |
| Phenotype (Memory) | Effector Memory (TEM) and TEMRA (CD45RA+, CX3CR1+, KLRG1+, CD57+) | >180 days post-symptom onset |
| Tissue Residence | Higher frequency in respiratory tract vs. blood; detectable in lungs & nasal mucosa for up to 12 months | Site-specific immunity analysis |
Visualization of Concepts and Workflows
Stem-like T Cell Differentiation and Viral Defense
T-cell Cross-reactivity Assay Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table: Essential Reagents for T-cell Immunity and Viral Variant Research
| Reagent / Tool | Function / Application | Example Use Case |
|---|---|---|
| Overlapping Peptide Pools | Synthetic peptides spanning viral proteins, 15-20 amino acids long, overlapping by 10-12 aa. Used to stimulate a broad T-cell response. | Mapping T-cell responses to the full-length spike protein of SARS-CoV-2 and its variants (e.g., Omicron BA.4/BA.5) [47]. |
| Protein Transport Inhibitors (Brefeldin A, Monensin) | Block protein secretion from the Golgi apparatus, causing cytokines to accumulate inside the cell for detection by intracellular staining. | Essential for Intracellular Cytokine Staining (ICS) assays to detect antigen-induced IFN-γ or TNF-α production. |
| MHC Multimers (Tetramers, Pentamers) | Recombinant MHC molecules complexed with a specific peptide and fluorescently labeled. Used to directly identify T cells with a specific T-cell receptor. | Tracking the frequency and phenotype of CD8+ T cells specific for a conserved epitope across different viral variants. |
| Anti-Cytokine Antibodies (e.g., anti-IFN-γ, anti-IL-2) | Conjugated antibodies used to detect cytokines intracellularly (by flow cytometry) or after capture (by ELISpot). | Quantifying polyfunctional T-cell responses (cells producing multiple cytokines) after stimulation with variant peptides [47]. |
| Anti-TCF1/TCF7 Antibody | Antibody for intracellular staining of the TCF1 transcription factor, a key marker for stem-like T cells. | Identifying and isolating the stem-like CD4+ T cell population for functional studies or to investigate their role in long-term immunity [48]. |
| Microscopy Kits (e.g., Duolink PLA) | Proximity Ligation Assay kits that allow for the visualization of protein-protein interactions or post-translational modifications in fixed cells/tissues. | Studying the interaction between T-cell receptors and signaling molecules in response to variant antigen stimulation [49]. |
This technical support center provides troubleshooting guides and FAQs for researchers navigating the integration of computational predictions and experimental testing in viral variant research. The content is designed to address common bottlenecks and streamline the path from in silico forecasts to validated biological findings.
Frequently Asked Questions (FAQs) & Troubleshooting
1. Our computational model identified numerous high-fitness viral variants. How can we prioritize which ones to test experimentally when lab resources are limited?
- Challenge: This is a classic bottleneck where computational throughput exceeds experimental capacity.
- Solution: Implement an Active Learning framework. Instead of testing all predictions at once, use a iterative loop where experimental results on a small, strategically chosen batch of variants are used to retrain and refine the computational model for the next selection round [9].
- Protocol: The VIRAL (Viral Identification via Rapid Active Learning) framework demonstrates this approach [9].
- Initial Screening: Your biophysical or AI model screens the sequence space and outputs an initial list of high-fitness candidates.
- Batch Selection: Select a small, diverse batch (e.g., 5-10 variants) that represents different areas of the predicted fitness landscape, not just the very top scores.
- Experimental Validation: Test this batch using a rapid assay (e.g., pseudovirus neutralization or binding affinity assays).
- Model Retraining: Feed the experimental results back into your computational model to improve its predictions.
- Iterate: Repeat steps 2-4. This method has been shown to identify high-risk variants up to five times faster than conventional approaches, using less than 1% of the experimental screening effort [9].
2. We are experiencing a bottleneck in generating and processing viral genomic data for validation studies. Are there tools to automate this?
- Challenge: Manual management and analysis of large-scale genomic data are slow and prone to inconsistency.
- Solution: Utilize automated computational workflows designed for viral genomic surveillance. These pipelines streamline raw data processing, variant calling, and consensus sequence generation.
- Protocol: ViralFlow v1.0 is a reference-based genome assembler workflow that can be adapted for various viruses [50].
- Input: Provide the workflow with raw sequencing reads (FASTQ files) and a reference genome.
- Automated Processing: The workflow automatically performs:
- Quality Control: Trims reads and removes adapters (using fastp).
- Read Mapping: Aligns reads to the reference genome (using BWA).
- Variant Calling and Annotation: Identifies and characterizes mutations (using Freebayes and SnpEff).
- Consensus Generation: Builds consensus sequences.
- Output: The workflow generates standardized outputs, including mutation reports, lineage assignments, and quality metrics, ready for public health reporting or further analysis [50].
3. How can we validate that a predicted variant actually confers enhanced immune evasion?
- Challenge: Establishing a direct link between a genetic mutation and a functional phenotype like immune evasion.
- Solution: Employ a combination of in vitro binding assays and in vivo/ex vivo neutralization studies.
- Protocol:
- Protein-Level Binding: Express the purified spike protein (or other relevant antigen) of the predicted variant. Use Surface Plasmon Resonance (SPR) or ELISA to quantitatively measure its binding affinity to human receptors (like ACE2 for SARS-CoV-2) and a panel of monoclonal antibodies. This directly tests the biophysical mechanism of evasion [9].
- Virus-Level Neutralization: Generate pseudoviruses or live viruses carrying the variant sequence. Incubate these with convalescent patient sera or vaccinated individual sera in a cell culture assay. Measure the reduction in neutralization potency (i.e., the increase in IC50 values) compared to a reference strain. This validates immune evasion in a more biologically relevant context [9] [27].
4. Our predictions were accurate for known variants but perform poorly when forecasting entirely new lineages. What could be wrong?
- Challenge: Models overfitting to existing data and failing to generalize, often due to ignoring epistasis (where the effect of one mutation depends on other mutations present).
- Solution: Incorporate epistasis directly into your predictive models. Use a biophysical model that quantitatively links mutations to fitness via structural and functional parameters, rather than relying solely on sequence frequency data.
- Troubleshooting Steps:
- Model Audit: Check if your model includes terms for mutational interactions. Models that treat all mutations as independent will fail to predict the emergence of novel combinations.
- Reframe the Problem: Forecast viral fitness based on the spike protein's binding affinity and antibody evasion capacity, as these biophysical properties are the ultimate drivers of evolutionary selection. A model that incorporates epistasis has been shown to successfully forecast dominant variants ahead of epidemiological signals [9].
The Scientist's Toolkit: Research Reagent Solutions
| Item | Function |
|---|---|
| Pseudovirus Systems | Safely study the infectivity and antibody neutralization of high-risk viral variants without requiring high-containment BSL-3 labs. |
| Protein Expression Systems | Produce purified viral antigen proteins (e.g., Spike protein) for structural studies and binding affinity assays. |
| Monoclonal Antibody Panels | A collection of antibodies targeting different viral epitopes to map the specific impact of mutations on immune evasion. |
| Clinical Sera Repository | Collected serum from convalescent and vaccinated individuals to test cross-neutralization against new variants. |
| Automated Workflows (e.g., ViralFlow) | Computational pipelines that automate genome assembly, variant calling, and annotation from raw sequencing data [50]. |
| Active Learning Frameworks (e.g., VIRAL) | AI-driven platforms that intelligently select which variants to test next in the lab, dramatically accelerating validation [9]. |
Experimental Protocol: Validating Immune Evasion of a Predicted Variant
Objective: To experimentally test a computationally predicted viral variant for enhanced antibody evasion.
Materials:
- Predicted variant sequence (e.g., Spike gene).
- Reference strain sequence (e.g., Wuhan-Hu-1).
- HEK-293T cells (or other suitable cell line).
- Plasmids for pseudovirus production.
- A panel of monoclonal antibodies and clinical sera.
- Cell culture plates and required media.
Methodology:
- Pseudovirus Generation:
- Co-transfect HEK-293T cells with a packaging plasmid, a reporter plasmid (e.g., encoding luciferase), and plasmids expressing the reference or predicted variant Spike protein.
- Incubate for 48-72 hours, then harvest the pseudovirus-containing supernatant.
- Titrate the pseudovirus to determine the volume needed for consistent infection.
Neutralization Assay:
- Serially dilute the monoclonal antibodies or clinical sera in a cell culture plate.
- Mix each dilution with an equal volume of the titrated pseudovirus. Incubate for 1 hour at 37°C.
- Add the mixture to cells susceptible to infection (e.g., ACE2-expressing cells).
- After a further incubation period (e.g., 48-72 hours), lyse the cells and measure the reporter signal (e.g., luciferase activity).
Data Analysis:
- Normalize the reporter signal from each sample to the signal from wells with no antibody (virus control).
- Plot the percentage neutralization against the antibody concentration.
- Calculate the half-maximal inhibitory concentration (IC50) for the reference and variant pseudoviruses. A statistically significant increase in the IC50 for the variant indicates enhanced immune evasion.
Quantitative Data on Validation Acceleration
The following table summarizes performance metrics from recent studies that have successfully streamlined the validation pipeline.
| Method / Approach | Key Performance Metric | Experimental Efficiency | Source / Context |
|---|---|---|---|
| VIRAL Active Learning Framework | Identified high-risk SARS-CoV-2 variants 5x faster than conventional approaches [9]. | Required < 1% of experimental screening effort [9]. | Forecasting viral variant evolution [9]. |
| Integrated Computational/Experimental Workflow | Accelerated discovery of functional organic materials by guiding synthesis with computational screening [51]. | Enabled screening of vast chemical spaces in silico before any lab work [51]. | Organic materials discovery (e.g., for optoelectronics, gas uptake) [51]. |
| Ultra-Large Virtual Screening | Screened 8.2 billion compounds computationally to select a clinical candidate [52]. | Only 78 molecules synthesized and tested before candidate selection [52]. | Computer-aided drug discovery [52]. |
Workflow Visualization
Streamlined Path from Prediction to Validation
Active Learning for Efficient Screening
In the field of viral evolutionary prediction, a significant challenge is identifying high-fitness variants with limited experimental resources. This is particularly crucial during the early stages of a pandemic when timely identification of concerning variants can shape public health responses. Active learning, a machine learning approach that strategically selects the most informative data points for experimental testing, has emerged as a powerful solution to this resource allocation problem [53].
The VIRAL framework (Viral Identification via Rapid Active Learning) exemplifies this approach, integrating protein language models with Bayesian optimization to accelerate the identification of high-fitness viral variants by up to fivefold compared to random sampling, while requiring experimental characterization of fewer than 1% of possible variants [53] [9]. This efficiency is achieved by combining multiple computational approaches: protein language models like ESM3 generate structure-aware sequence embeddings; Gaussian Processes predict binding affinities with uncertainty estimates; and biophysical models map these affinities to viral fitness metrics [53].
For researchers and drug development professionals, implementing these approaches requires understanding both the technical methodology and practical workflow integration. The following sections address common implementation challenges through troubleshooting guidance, experimental protocols, and visual workflows.
Frequently Asked Questions
What is the primary advantage of using active learning over high-throughput screening for viral variant identification? Active learning dramatically reduces experimental burden by strategically selecting which variants to test. Where high-throughput screening might require testing thousands of variants, the VIRAL framework identifies high-fitness variants by experimentally characterizing fewer than 1% of possible variants, achieving up to fivefold acceleration in variant identification [53] [9].
Why is incorporating uncertainty quantification important in active learning strategies? Uncertainty quantification, such as through Upper Confidence Bound (UCB) acquisition functions, balances the "exploitation" of known high-fitness regions with "exploration" of uncertain regions. This prevents the model from getting stuck in local fitness maxima and enables identification of evolutionarily distant but potentially dangerous variants that might be missed by greedy strategies [53].
How can we ensure data from different research groups is interoperable for integrated analysis? Implementing a data harmonization framework with Common Data Elements (CDEs) and adhering to FAIR (Findable, Accessible, Interoperable, Reusable) principles ensures interoperability. This includes using shared metadata standards, structured formats, and detailed documentation of experimental conditions [54].
Our team struggles with inconsistent metadata collection across lab members. What practices can help? Establish a two-step metadata practice: (1) systematically record and store raw metadata from all workflow stages, and (2) use tools like the Archivist Python package to select and structure this metadata into unified formats. This approach can be implemented in existing workflows without substantial restructuring [55].
Which visualization colors should be avoided in research presentations and publications? Avoid color combinations indistinguishable to viewers with color vision deficiency (particularly red/green). Use perceptually uniform color gradients (e.g., viridis, cividis) instead of rainbow scales, and test accessibility by converting figures to grayscale to ensure all data remains distinguishable [56].
Troubleshooting Common Experimental Issues
Problem: Active Learning Model Performs Poorly with Limited Initial Data
Issue: When starting with very few known variants (<50 data points), the model fails to identify high-fitness variants effectively.
Solution:
- Utilize Protein Language Model Embeddings: Use models like ESM3 that provide structure-aware sequence embeddings, which serve as informative priors. ESM3 with structural information achieved a Spearman coefficient of 0.53 on combinatorial mutation data when trained on only 20 points (0.06% of dataset) [53].
- Incorporate Biophysical Models: Integrate biophysical models that map binding affinities (ACE2 receptor binding and antibody escape) to fitness, which reduces the functional space that needs to be explored experimentally [53].
- Start with Maximum 2-Mutation Variants: Begin active learning cycles with variants containing no more than 2 mutations, mimicking early pandemic scenarios where highly mutated variants haven't yet emerged [53].
Problem: Inconsistent Experimental Results Across Research Sites
Issue: Teams at different locations generate data that cannot be directly compared or integrated.
Solution:
- Implement Common Data Elements (CDEs): Develop and implement CDEs across all research sites to ensure consistent data collection [54].
- Establish Metadata Standards: Adopt minimal metadata standards specific to your experimental type (e.g., 3D Microscopy Metadata Standards for imaging data) [54].
- Provide Contextual Data: For biospecimens, obtain low-magnification images showing the precise location from which samples were collected, giving data users essential context for interpretation [54].
- Use Standardized Color Maps: Employ scientifically-derived, accessible color maps (e.g., "viridis," "cividis") for all data visualization to ensure accurate representation [56].
Problem: High Performance Computing (HPC) Simulation Workflows Lack Reproducibility
Issue: Inability to replicate simulation results due to inconsistent tracking of software, hardware, and model parameters.
Solution:
- Capture Comprehensive Workflow Metadata: Systematically record metadata at each stage: software environment configuration, simulation engine setup, model parameters, execution details, and storage information [55].
- Implement a Data Model: Develop an abstract representation of data objects and their relationships to maintain organization and integrity of simulation collections over time [55].
- Use Provenance Tracking Tools: Employ workflow management tools like Sumatra, AiiDA, or Snakemake to track data lineage and experimental conditions [55].
Experimental Protocols & Data
VIRAL Framework Implementation Protocol
The following table outlines the core components of the VIRAL active learning framework for viral variant prediction [53]:
| Component | Description | Implementation Example |
|---|---|---|
| Protein Language Model | Generates structure-aware sequence embeddings | ESM3 with RBD structure (PDB 6M0J) as input |
| Surrogate Model | Predicts binding affinity with uncertainty | Gaussian Process with RBF kernel |
| Acquisition Function | Selects most informative variants for testing | Upper Confidence Bound (UCB) balancing exploration & exploitation |
| Biophysical Model | Maps binding affinities to fitness | Computes infectivity from ACE2 binding & antibody escape |
| Experimental Validation | Tests selected variants | Surface Plasmon Resonance or Deep Mutational Scanning |
Key Research Reagents and Solutions
| Reagent/Solution | Function | Application Example |
|---|---|---|
| ESM3 Protein Language Model | Generates structure-aware protein sequence embeddings | Feature generation for SARS-CoV-2 spike protein variants [53] |
| Deep Mutational Scanning (DMS) | High-throughput measurement of mutation effects | Functional characterization of viral variant libraries [53] |
| Surface Plasmon Resonance (SPR) | Measures biomolecular binding interactions & kinetics | Quantifying ACE2 receptor binding affinity [53] |
| Combinatorial Mutagenesis (CM) | Generates & tests multiple mutation combinations | Exploring epistatic effects in viral protein evolution [53] |
| Gaussian Process Regression | Bayesian non-parametric fitting with uncertainty | Predicting variant fitness from limited experimental data [53] |
Quantitative Performance Metrics
The table below shows the performance advantage of active learning compared to baseline approaches in identifying high-fitness variants [53]:
| Method | Enrichment Factor | Experimental Effort | Key Advantage |
|---|---|---|---|
| Random Sampling | 1.0x (baseline) | ~100% screening | Brute-force approach |
| Greedy Acquisition | <1.5x | ~0.4% of dataset | Focuses on predicted high-fitness variants |
| UCB Acquisition | 5.0x | ~0.4% of dataset | Balances exploration & exploitation |
Workflow Visualization
Active Learning Workflow for Viral Variant Identification
Data Harmonization Framework for Team Science
Benchmarks and Real-World Performance: Validating Predictions Against Viral Reality
Frequently Asked Questions
Q1: What is a common reason for large errors in my variant frequency forecasts, and how can I fix it?
Large forecast errors often stem from insufficient genomic sequence data. A downsampling analysis revealed that forecasting accuracy stabilizes and becomes reliable once sequence data exceeds approximately 1,000 sequences per week for a given population. If your forecasts are inaccurate, audit the volume and timeliness of your sequence input data [57].
Q2: My model fails to accurately 'hindcast' past variant dynamics. What does this indicate?
Poor performance in hindcasting (estimating past frequencies) suggests potential issues with model over-fitting or fundamental model misspecification. A model that cannot recreate known past dynamics is unlikely to produce reliable future forecasts. Begin troubleshooting by validating your model against a historical period with well-established truth data [57].
Q3: How do I choose the right model for short-term variant frequency forecasting?
For short-term forecasts (e.g., 30-day outlook), simpler models like Multinomial Logistic Regression (MLR) can perform as well as, or even better than, more complex models. One study found MLR achieved a median absolute error of ~0.6% for 30-day forecasts in countries with robust surveillance. Start simple and upgrade complexity only if it provides a demonstrated accuracy benefit [57].
Q4: Why do my experimental evolution results not match viral evolution observed in nature?
Laboratory systems, particularly those using monolayers of tumoral cells, provide an unnaturally permissive environment that fails to replicate key selective pressures found in a host, such as immune responses. To improve real-world relevance, consider using more advanced systems like organoids or 3D cultures, and always contrast your laboratory findings with field sequence data [23].
Troubleshooting Guides
Issue: Inaccurate Nowcasts (Estimates of Current Variant Frequency)
Problem: Your model's estimate of variant frequencies for the most recent time points consistently deviates from later, more complete data.
| Potential Cause | Diagnostic Steps | Solution |
|---|---|---|
| Data Backfill Delay | Analyze the lag between sample collection date and sequence submission date in your data source. | Implement a data correction procedure that explicitly models the backfill process to adjust for the expected delay [57]. |
| Low Sequencing Volume | Calculate the number of sequences available per week. Is it below 1,000? | Source additional sequence data from supplementary repositories or collaborate with surveillance programs to increase throughput [57]. |
| Inadequate Model for Extrapolation | Compare the performance of a simple 7-day moving average against your model for the most recent time points. | Switch to or incorporate a model like MLR that is better at extrapolating from incomplete recent data [57]. |
Issue: Poor Forecast Performance Across Multiple Time Horizons
Problem: Your model's forecasts are inaccurate for both short-term (e.g., 2-week) and longer-term (e.g., 6-week) projections.
| Potential Cause | Diagnostic Steps | Solution |
|---|---|---|
| Incorrect Fitness Assumptions | Check if the model assumes a fixed growth advantage for variants when in reality fitness may be changing. | Use a model that allows for variant fitness to change over time, such as the Growth Advantage Random Walk (GARW) [57]. |
| Poor State/Parameter Estimation | Review the data assimilation method (filter) used to fit the model to data. | Test different filtering methods; for compartmental models, Ensemble Kalman Filters (EnKF) often provide robust state estimation [58]. |
| Ignored Key Drivers | Audit model inputs. Are external drivers like population immunity or non-pharmaceutical interventions included? | Enrich the model structure to include key known drivers of transmission dynamics, such as vaccination rates and contact patterns [59]. |
Quantitative Data from Retrospective Studies
The table below summarizes the performance of different forecasting models as evaluated in a 2022 retrospective study of SARS-CoV-2 variant dynamics [57].
Table 1: Model Forecasting Error (Median Absolute Error) for Variant Frequencies
| Model | Forecast Lag: -30 days (Hindcast) | Forecast Lag: 0 days (Nowcast) | Forecast Lag: +30 days (Forecast) |
|---|---|---|---|
| Multinomial Logistic Regression (MLR) | 0.1% - 1.4% | 0.3% - 2.0% | 0.5% - 1.9% |
| Fixed Growth Advantage (FGA) | 0.2% - 1.5% | 0.3% - 2.3% | 0.6% - 2.1% |
| Growth Advantage Random Walk (GARW) | 0.2% - 0.8% | 0.3% - 1.6% | 0.5% - 1.9% |
| Piantham Model | 0.2% - 1.5% | 0.3% - 2.1% | 0.6% - 2.0% |
| Naive Model (7-day moving average) | 0.4% - 12.5% | 2.1% - 20.0% | 5.8% - 25.0% |
Table 2: Impact of Genomic Surveillance Quality on Forecast Accuracy
| Surveillance Characteristic | Impact on Forecast Error | Minimum Recommended Threshold |
|---|---|---|
| Sequencing Volume | Mean Absolute Error (MAE) decreases significantly as volume increases, plateauing at high volume. | 1,000 sequences per week for a population [57] |
| Data Timeliness (Backfill) | Significant delays between sample collection and submission increase nowcast error. | Minimize submission lag; model and correct for expected backfill [57] |
| Variant Granularity | Forecasting using overly specific lineages (e.g., Pango) can be noisier than using clades. | Use an appropriate level of granularity, such as Nextstrain clades, for dynamics modeling [57] |
Experimental Protocols
Protocol: Conducting a Retrospective Forecast Evaluation
This methodology is used to benchmark the accuracy of a forecasting model using historical data [57].
- Define Analysis Dates: Select regular intervals (e.g., 1st and 15th of each month) for the period of interest to serve as your forecast origins.
- Reconstruct Historical Data Sets: For each analysis date, use the sequence submission date to filter to only the data that was actually available to analysts at that past moment in time. This faithfully recreates the informational constraints of the past.
- Run Models: Execute your forecasting model for each analysis date, producing estimates of variant frequency from 90 days prior (hindcast) to 30 days post (forecast) the analysis date.
- Establish Ground Truth: Calculate a 7-day smoothed variant frequency using the entire, complete dataset available retrospectively. This serves as the "truth" for evaluation.
- Calculate Error Metrics: Compare the model predictions from step 3 against the ground truth from step 4 for every time point. Standard metrics include:
- Absolute Error (AE): ( | \text{Predicted Frequency} - \text{Truth Frequency} | )
- Mean Absolute Error (MAE): Average of AE across all variants and time points.
- Median Absolute Error: Median of AE across all variants and time points.
Protocol: Evaluating the Impact of Sequencing Effort via Downsampling
This procedure determines the minimum sequencing volume required for reliable forecasts [57].
- Obtain a Complete Dataset: Start with a high-quality, high-volume genomic dataset for a region and time period.
- Define Downsampling Levels: Choose a range of target sequence counts per week (e.g., 50, 100, 500, 1000, 5000).
- Generate Subsampled Data: For each week, randomly sample the specified number of sequences without replacement from the full dataset. Repeat this process multiple times (e.g., 10-100 iterations) to account for stochasticity.
- Run Forecasts: Execute your forecasting model on each of the downsampled datasets.
- Analyze Error vs. Volume: Plot the forecasting error (e.g., MAE) against the sequencing volume. The point where the error curve plateaus indicates the volume beyond which additional sequencing provides diminishing returns.
Research Reagent Solutions
Table 3: Essential Materials and Resources for Retrospective Forecasting Research
| Item | Function / Application | Example / Source |
|---|---|---|
| Genomic Sequence Data | The primary input data for estimating variant frequencies and fitting models. | GISAID EpiCoV database [57] |
| Multinomial Logistic Regression (MLR) Model | A simple, effective model for forecasting variant frequency growth; treats variant growth advantage as fixed. | Implemented in various phylogenetic software; analogous to a haploid population genetics model [57] |
| Variant Rt Models (FGA, GARW) | More complex models that estimate variant-specific effective reproduction numbers (Rt) using both sequence counts and case data. | Fixed Growth Advantage (FGA) and Growth Advantage Random Walk (GARW) parameterizations [57] |
| Data Assimilation Filters | Algorithms used to recursively estimate model state variables and parameters as new data arrives. | Ensemble Kalman Filter (EnKF), Particle Filter (PF) [58] |
| Stochastic Compartmental Models | Multi-strain transmission models used to project case numbers and assess the impact of variants, incorporating real-world data like contact patterns and vaccination rates [59]. | SIRS-type models, often coded in R, Python, or specialized modeling frameworks |
Workflow and Model Diagrams
Retrospective Forecast Validation Workflow
Model Comparison Logic
The evolutionary prediction of viral variants aims to forecast strains with enhanced transmissibility or immune escape. However, a significant challenge in this field lies in the wet-lab validation of these computational predictions. Pseudovirus-based neutralization assays (PBNAs) have emerged as a critical, scalable tool for bridging this gap, allowing researchers to quantitatively measure the immune escape of forecasted variants in a biosafe environment [9] [60]. Establishing a robust correlation between in silico forecasts and in vitro assay results is fundamental to transforming predictive models into actionable public health insights, such as guiding vaccine updates [61] [9].
Core Experimental Protocol: From Prediction to Validation
This section outlines a standardized workflow for using pseudovirus neutralization assays to validate computational predictions of immune escape.
The following diagram illustrates the end-to-end process, from viral sequence to validated prediction.
Detailed Protocol: Pseudovirus Neutralization Assay
Objective: To measure the neutralizing antibody activity in serum samples against a predicted viral variant and calculate the fold-change reduction compared to a reference strain (e.g., Wuhan) [61] [60].
Materials & Reagents:
- Pseudovirus: Replication-incompetent viral particles (e.g., based on VSV or lentivirus backbone) pseudotyped with the spike protein of the predicted variant and a reporter gene (Luciferase or GFP) [60] [62].
- Cell Line: ACE2/TMPRSS2-expressing cells, such as HEK293T-ACE2 or Vero E6-ACE2-TMPRSS2 [60].
- Sera: Panel of serum samples from vaccinated individuals or convalescent patients [61] [63].
- Controls: Positive control (reference sera), negative control (pre-immune or naive sera), and cell-only control.
- Equipment: Cell culture incubator (37°C, 5% CO2), luminometer (for luciferase) or flow cytometer (for GFP), biological safety cabinet (BSL-2) [60].
Step-by-Step Procedure:
Serum Serial Dilution: Prepare a series of 2-fold or 3-fold serial dilutions of the heat-inactivated (56°C for 30 minutes) serum samples in cell culture medium in a 96-well plate [63].
Virus-Serum Incubation: Add a standardized amount of pseudovirus (e.g., 1000 TCID50/well) to each serum dilution. Include virus control wells (virus + medium) and cell control wells (medium only). Incube the plate for 1-2 hours at 37°C [63] [62].
Cell Infection: Seed the target cells (e.g., HEK293T-ACE2) into the plate. Incubate the plate for 24-48 hours to allow for infection and reporter gene expression [60].
Signal Detection:
- For Luciferase-based reporters: Lyse cells and add luciferase substrate. Measure the Relative Luminescence Units (RLU) using a microplate luminometer [60].
- For GFP-based reporters: Quantify fluorescence intensity or the percentage of GFP-positive cells using a flow cytometer or fluorescence plate reader.
Data Calculation:
- Calculate the percentage of neutralization for each serum dilution using the formula:
% Neutralization = [1 - (RLU of test sample / RLU of virus control)] × 100. - Determine the neutralization titer (NT50), defined as the reciprocal serum dilution that inhibits 50% of the pseudovirus infection, using a non-linear regression model (e.g., four-parameter logistic curve) [63] [60].
- Calculate the Geometric Mean Titer (GMT) for each sample group.
- The key metric for immune escape is the fold-change (FC) in NT50 or GMT from the reference virus to the variant:
Fold Change (FC) = GMT (Reference) / GMT (Variant)[61].
- Calculate the percentage of neutralization for each serum dilution using the formula:
The table below catalogs the core components required for establishing and running a pseudovirus neutralization assay.
Table 1: Key Research Reagent Solutions for Pseudovirus Assays
| Item | Function | Examples & Notes |
|---|---|---|
| Pseudovirus System | Core reagent for safe simulation of viral entry under BSL-2 conditions. | VSV-ΔG (e.g., G*VSV-ΔG-LUC) or Lentiviral backbone; available from commercial vendors (e.g., Integral Molecular) or as in-house systems [60] [64]. |
| Cell Line with Receptor | Host cell for pseudovirus infection; provides the viral entry point (e.g., ACE2 for SARS-CoV-2). | HEK293T-hACE2, Vero E6-ACE2-TMPRSS2. TMPRSS2 expression can enhance infection efficiency [60]. |
| Reference Sera | Critical for assay standardization, normalization, and quality control across experiments and labs. | WHO International Standard or other well-characterized pooled convalescent/vaccinated sera [60]. |
| Reporter Detection Kit | For quantifying neutralization based on signal reduction (e.g., luminescence). | Luciferase assay systems; ensure compatibility with the reporter gene in your pseudovirus [60]. |
| DNA Synthesis & Cloning | For rapid construction of plasmids expressing variant spike proteins. | High-fidelity DNA synthesis and cloning services (e.g., Twist Bioscience) to accurately translate AI-designed sequences into testable reagents [65]. |
Troubleshooting Guides and FAQs
Frequently Asked Questions (FAQs)
Q1: How well do pseudovirus neutralization assay (PBNA) results correlate with the gold-standard live virus assays? A1: When properly validated, PBNAs show a strong correlation with live virus neutralization tests. A 2025 study analyzing over 500 samples found Pearson correlation coefficients of 0.907 to 0.961 across variants (Alpha, Beta, Delta), with sensitivity and specificity rates exceeding 90% [63]. This supports PBNA as a reliable surrogate for immune escape assessment.
Q2: Can PBNAs keep pace with the rapid emergence of new variants predicted by models? A2: Yes, the modular nature of PBNAs is one of their greatest strengths. The spike protein plasmid can be rapidly swapped to represent a newly predicted variant, allowing for timely immune profiling. This enables the aggregation of data from multiple public sources to quickly gauge a new variant's immune escape, as demonstrated during the Omicron BA.1 wave [61] [60].
Q3: Our AI model predicts a novel combination of mutations. What is the best way to validate this? A3: This requires a closed "wet-lab feedback loop." The predicted spike protein sequence should be synthesized de novo (e.g., using multiplex gene fragments), packaged into a pseudovirus, and tested in neutralization assays. The resulting experimental data is then fed back into the AI model to refine future predictions, creating an iterative cycle of improvement [9] [65].
Troubleshooting Common Experimental Issues
Problem: Poor Correlation Between Replicates or with Published Data
- Potential Cause: Inconsistent pseudovirus production or titer.
- Solution:
- Standardize the pseudovirus production protocol (transfection time, amount of DNA, harvest time) [62] [64].
- Always titrate each new batch of pseudovirus to ensure a consistent infectious dose (e.g., 1000 TCID50) is used across experiments.
- Include a standardized reference serum in every assay run to monitor inter-assay variability [60].
Problem: High Background Signal (Low Signal-to-Noise Ratio)
- Potential Cause: Suboptimal cell density or excessive pseudovirus input.
- Solution:
- Optimize the cell seeding density and the multiplicity of infection (MOI) of the pseudovirus. A 2025 measles PBNA study highlighted that varying cell density and virus input significantly impacts assay performance and must be predetermined [62].
- Validate the linear range of your assay by testing different virus inputs against a standard serum.
Problem: Weak or No Neutralization Signal
- Potential Cause: Serum toxicity, low antibody titer, or pseudovirus not infecting target cells efficiently.
- Solution:
- Include a cell control (cells only) and a serum toxicity control (serum + cells, no virus) to rule out cytotoxic effects.
- Confirm the functionality of your pseudovirus by ensuring it robustly infects the receptor-expressing cell line compared to the parental cell line.
- Verify the correct expression and incorporation of the variant spike protein into the pseudovirus particles via Western blot or flow cytometry [64].
Data Presentation and Interpretation
Accurate data presentation is crucial for interpreting immune escape. The table below summarizes a framework for data aggregation, as demonstrated in a large-scale study of the Omicron BA.1 variant.
Table 2: Quantitative Framework for Assessing Immune Escape from Aggregated Neutralization Data [61]
| Serum Cohort | Key Metric | Interpretation & Application |
|---|---|---|
| 2x Vaccinated (Wu-1) | Fold-Change (FC) in GMT from WT to variant. | A stable, significant FC (e.g., ~8-fold drop for BA.1) provides an early, reliable indicator of substantial immune escape in this population [61]. |
| 3x Vaccinated (Wu-1) | Fold-Change (FC) in GMT and its stability over time. | Early estimates may be unstable; data from multiple sources must accumulate for the mean FC to converge on a reliable value, highlighting the need for aggregated data [61]. |
| Convalescent (WT) | Fold-Change (FC) in GMT from infecting strain to variant. | Like the 2x Vax group, this FC can stabilize quickly, providing a rapid assessment of escape from natural immunity [61]. |
The relationships between different assay types and their role in a predictive research framework are shown below.
Technical Support Center: Troubleshooting Guides and FAQs
Frequently Asked Questions
Q1: Why does my model show good discriminative ability but poor calibration when predicting viral variant fitness? This discrepancy often occurs when using metrics like C-statistics without assessing calibration. The C-for-benefit measures discriminative ability but doesn't evaluate how well predicted probabilities match observed outcomes. To address this, implement calibration-specific metrics like Eavg-for-benefit, E50-for-benefit, and E90-for-benefit, which measure the average, median, and 90th quantile of absolute differences between predicted and observed treatment effects. Additionally, use the Brier-for-benefit score to assess overall performance [66].
Q2: How can I better link experimental evolution data with real-world viral evolution? Current experimental systems often use monolayers of tumoral cells, which offer unnaturally permissive environments. To improve real-world relevance, transition to more complex systems including non-tumoral cells, 3D cultures, organoids, and explants. These better reflect selective pressures found in vivo, though they may achieve lower viral yields. Additionally, contrast laboratory findings with field data through genomic surveillance pipelines like those used for SARS-CoV-2 tracking [23] [67].
Q3: What metrics should I prioritize when evaluating models for predicting viral variant emergence? Focus on a comprehensive set of metrics covering different performance aspects:
- Discrimination: C-for-benefit for treatment effect prediction
- Calibration: Eavg-for-benefit, E50-for-benefit, E90-for-benefit
- Overall performance: Brier-for-benefit and cross-entropy-for-benefit No single metric provides a complete picture, so use this combination to evaluate different aspects of model performance [66].
Q4: How can I account for different evolutionary timescales in my predictive models? Acknowledge that viral evolution rates inferred from phylogenetic analyses strongly depend on measurement timescales. Rates from recent isolates are systematically higher than those from longer periods. Address this by developing models that explicitly incorporate temporal scale and link evolutionary processes across intra-host, inter-host, and community levels through common evolutionary events identified at different spatiotemporal scales [23].
Q5: What are the key challenges in defining and measuring viral fitness in predictive models? Viral fitness is context-dependent and varies across organizational levels. Factors that determine fitness include:
- Rate of cellular infection (receptor binding, replication efficiency)
- Immune evasion capabilities as infection progresses
- Shedding ability and environmental stability during transmission Develop multi-scale fitness measures that link mechanistic aspects of viral infection (polymerase efficiency, receptor affinity) to population-level metrics like basic reproductive rate (R0) [23].
Troubleshooting Guides
Issue: Model Performance Degradation with New Viral Variants
| Step | Procedure | Expected Outcome |
|---|---|---|
| 1 | Re-evaluate fitness landscape assumptions | Identification of changed selection pressures |
| 2 | Assess genomic robustness and neutral networks | Understanding of mutation tolerance |
| 3 | Implement updated virus characterization | Improved variant impact assessment |
| 4 | Integrate new surveillance data | Enhanced model relevance to circulating strains |
Root Cause: Viral evolution alters fitness landscapes, making previous assumptions obsolete. RNA viruses exhibit high mutation rates and can evolve robust genomes that localize within broad neutral networks [35].
Resolution Protocol:
- Recalibrate Selection Pressures: Isolate emerging viruses from positive specimens and evaluate their characteristics relative to current variants [67].
- Update Training Data: Incorporate new genomic surveillance data from public repositories to ensure models reflect currently circulating strains [67].
- Adjust Fitness Parameters: Account for the fact that overall fitness requires performance across multiple tasks (entry, replication, dissemination, transmission), not just replication speed [35].
Issue: Discrepancy Between Laboratory Predictions and Natural Viral Evolution
| Step | Procedure | Expected Outcome |
|---|---|---|
| 1 | Compare cell culture systems | Identification of unrealistic selective pressures |
| 2 | Implement organoid/3D culture models | Better reflection of in vivo conditions |
| 3 | Analyze population bottleneck effects | Understanding of stochastic influences |
| 4 | Validate with phylogenetic data | Improved correlation with natural evolution |
Root Cause: Simplified laboratory systems (e.g., tumoral cell monolayers) create unnaturally permissive environments that don't reflect the complex selective pressures viruses encounter in natural hosts [23].
Resolution Protocol:
- Enhance Experimental Systems: Transition to non-tumoral cells, 3D cultures, and organoids that better mimic in vivo conditions [23].
- Account for Population Dynamics: Model how fluctuating population sizes and bottlenecks through transmission events influence viral evolution and variant selection [35].
- Incorporate Host Complexity: Design experiments that reflect how fitness values shift across different tissues and host environments, as high fitness in one tissue may represent lower fitness in another [35].
Performance Metrics for Predictive Models
| Metric Category | Specific Metric | Optimal Value | Interpretation | Use Case |
|---|---|---|---|---|
| Calibration | Eavg-for-benefit | 0.002 | Average absolute error in predicted vs. observed effects | Treatment effect prediction [66] |
| E50-for-benefit | 0.001 | Median absolute error | Robust to outliers in treatment effect [66] | |
| E90-for-benefit | 0.004 | 90th quantile of absolute error | Worst-case calibration assessment [66] | |
| Overall Performance | Brier-for-benefit | 0.218 | Mean squared error for treatment effect | Overall model accuracy [66] |
| Cross-entropy-for-benefit | 0.750 | Logarithmic loss for treatment effect | Probabilistic prediction assessment [66] | |
| Discrimination | C-for-benefit | >0.7 | Ability to distinguish benefit groups | Treatment effect heterogeneity [66] |
Viral Evolution Rate Inconsistencies Across Timescales
| Timescale | Evolutionary Rate Pattern | Implications for Predictive Modeling |
|---|---|---|
| Short-term (seasonal outbreaks) | Systematically higher rates | Models may overestimate evolutionary potential |
| Long-term (archival samples) | Systematically lower rates | Models may underestimate adaptation capacity |
| Integrated approaches | Rate reconciliation needed | Multi-scale models required for accuracy |
Data from [23] indicates that viral evolution rates inferred from phylogenetic analyses are strongly timescale-dependent, creating challenges for predictive models.
Experimental Protocols
Genomic Surveillance and Variant Characterization Protocol
Purpose: To track emerging SARS-CoV-2 variants and other viruses of concern to inform public health response and predictive model updates [67].
Methodology:
- Specimen Receipt and Processing:
- Clinical specimens (nasal swabs) are received and entered into laboratory information systems
- De-identified specimens are shipped to centralized sequencing facilities
Specimen Preparation and Sequencing:
- SARS-CoV-2 RNA is extracted and converted to complimentary DNA
- Libraries are prepared for sequencing and loaded into next-generation sequencing equipment
- Quality control tests are performed at multiple stages to verify accuracy
Sequence Data Generation:
- Specimens are sequenced and data is collected from sequencers
- Raw data is processed and transformed into sequence data
- Sequences not initially accepted by public repositories are analyzed and potentially re-sequenced
Data Submission and Analysis:
- Sequence data is submitted to public repositories (e.g., NCBI databases)
- Scientists conduct detailed analyses to identify variants and monitor prevalence
- Representative viruses are selected for further characterization
Timeline: Approximately 10+ days from specimen receipt to assembled sequence readiness [67].
Performance Metric Validation Protocol for Treatment Effect Models
Purpose: To comprehensively evaluate models predicting individualized treatment effect in randomized clinical trials, addressing the challenge of unobservable counterfactual outcomes [66].
Methodology:
- Data Preparation:
- Collect outcomes from RCT with different treatment assignments
- Prepare matched pairs of patients with different treatment assignments based on Mahalanobis distance between characteristics
Metric Calculation:
- Compute observed pairwise treatment effect as difference between outcomes in matched pairs
- Calculate predicted pairwise treatment effects from model outputs
- Apply local-regression smoothing to observed pairwise treatment effects
Performance Assessment:
- Calibration: Compute Eavg-for-benefit, E50-for-benefit, and E90-for-benefit as average, median, and 90th quantile of absolute distance between predicted and smoothed observed effects
- Overall Performance: Calculate Brier-for-benefit as average squared distance between predicted and observed effects
- Discrimination: Compute C-for-benefit using previously established methods
Model Comparison:
- Compare metric values across different modeling approaches (risk modeling with splines, effect modeling with penalized interactions, causal forests)
- Select optimal model based on comprehensive metric profile
Implementation: Available in R package "HTEPredictionMetrics" [66].
Workflow Visualization
Viral Variant Surveillance and Modeling Workflow
Performance Metric Validation Workflow
Research Reagent Solutions
| Reagent/Resource | Function | Application in Viral Variant Research |
|---|---|---|
| BEI Resources | Virus isolate sharing | Provides characterized viral variants for experimental validation [67] |
| Public Sequence Databases (NCBI) | Genomic data repository | Enables access to global surveillance data for model training [67] |
| HTEPredictionMetrics R Package | Performance metric calculation | Implements comprehensive metrics for treatment effect models [66] |
| Advanced Molecular Detection Tools | Genomic sequencing capacity | Supports implementation of genomic surveillance at public health labs [67] |
| Organoid/3D Culture Systems | Physiologically relevant hosts | Provides more natural environments for experimental evolution studies [23] |
| Deep Mutational Scanning | High-throughput variant characterization | Enables systematic assessment of mutation fitness effects [23] |
FAQs: Core Concepts and Data Challenges
What is the primary goal of pre-emptive vaccine strain selection? The goal is to select vaccine strains that will provide the best protection against future circulating viral variants, thereby optimizing vaccine effectiveness (VE). This requires predicting which viral strains will dominate in an upcoming season and how well candidate vaccines will antigenically match them [68].
What are the key data sources used for these predictions? Two primary types of data are crucial:
- Viral Genomic Data: Sequencing data from global surveillance databases (e.g., GISAID) provides the distribution of viral genotypes and is used to compute a strain's future dominance [68].
- Antigenicity Data: Measurements from in vitro assays like hemagglutination inhibition (HI) tests quantify how well antibodies induced by a vaccine candidate can inhibit a circulating virus [68].
What is a "coverage score" and why is it important? The coverage score is a quantitative measure of a vaccine's antigenic match. It is calculated as the average of its antigenicity across circulating viral strains, weighted by each strain's dominance. This score is a key predictor of vaccine effectiveness [68].
What is the main limitation of current vaccine selection methods? The traditional process relies on expert analysis of available data and can be reactive. The time between strain selection and vaccine availability (6-9 months) means the viral landscape can shift, leading to a suboptimal antigenic match. For instance, influenza vaccine effectiveness in the U.S. averaged below 40% between 2012 and 2021 [68].
FAQs: Technical Hurdles and AI Integration
How do AI models address the challenge of viral evolution? AI models can learn the complex relationship between a virus's protein sequences and its fitness. For example, dominance predictors use protein language models and ordinary differential equations to forecast how a virus's prevalence will change over time, moving beyond static fitness landscapes to model dynamic shifts [68].
How can we predict antigenicity without exhaustive lab testing? Antigenicity predictors are AI models that take the hemagglutinin (HA) protein sequences of a vaccine and a virus as input and predict the outcome of an HI test. This allows for in-silico screening of countless vaccine-virus pairs, which is prohibitively expensive in the lab [68].
What is epistasis and why does it complicate predictions? Epistasis occurs when the effect of one mutation depends on the presence of other mutations. This non-linear interaction is a key driver of viral evolution. Models that factor in epistasis can more accurately forecast the emergence of dominant variants by capturing these complex relationships [9].
How can we validate a predictive model before a season occurs? The gold standard is retrospective validation. Researchers train models on historical data and evaluate their performance against what actually happened. For example, the VaxSeer model was validated over 10 years of past influenza seasons and was shown to consistently select strains with better empirical antigenic matches than the annual recommendations [68].
Troubleshooting Guide: Experimental Pitfalls
| Problem | Potential Cause | Solution |
|---|---|---|
| Poor correlation between predicted and empirical VE | Model is overfitted to historical antigenic relationships and fails to generalize to novel variants. | Incorporate biophysical features (e.g., spike protein binding affinity) and epistatic interactions into the model to improve generalization to new variants [9]. |
| Inaccurate dominance forecasts | Model treats mutations as independent and additive, failing to capture higher-level protein properties. | Use a dominance predictor that leverages protein language models and ODEs to automatically capture complex interactions across the protein sequence [68]. |
| Inability to test all candidate-virus pairs | High-throughput experimental antigenicity testing (e.g., HI) is resource-intensive and low-throughput. | Use an antigenicity prediction model to perform initial in-silico screening, prioritizing the most promising candidate vaccines for subsequent lab validation [68]. |
| Slow identification of high-risk variants | Conventional approaches require testing a vast number of mutations when a new threat emerges. | Implement an active learning framework (e.g., VIRAL) that combines AI with biophysical models to focus experimental efforts on the most concerning mutations, dramatically accelerating identification [9]. |
Experimental Protocols
Protocol 1: In-Silico Prediction of Antigenic Match (Coverage Score)
Purpose: To prospectively rank candidate vaccine strains based on their predicted antigenic match against a future season's circulating viruses.
Methodology:
- Input Data: Gather a set of candidate vaccine HA protein sequences and a pool of recently circulating viral HA sequences [68].
- Dominance Prediction: For each viral sequence in the pool, use a trained dominance predictor (e.g., based on protein language models and ODEs) to estimate its expected dominance in the target season [68].
- Antigenicity Prediction: For each candidate vaccine and each circulating virus pair, use a trained antigenicity predictor to estimate the HI titer. This model typically uses a neural network architecture that takes a pairwise sequence alignment as input [68].
- Score Calculation: For each candidate vaccine, compute the predicted coverage score using the formula: Coverage Score = Σ (Predicted Dominance of Virus_i × Predicted Antigenicity to Virus_i) The candidate with the highest score is predicted to have the broadest protection [68].
Protocol 2: Forecasting High-Risk Viral Variants
Purpose: To proactively identify viral mutations that are likely to enhance transmissibility and immune escape before they become widespread.
Methodology:
- Biophysical Modeling: Develop a model that quantitatively links biophysical features of a viral protein (e.g., binding affinity to human receptors and antibody evasion capability) to a variant's likelihood of surging in the population. This model must incorporate epistatic interactions [9].
- AI-Powered Screening: Integrate this biophysical model with an active learning AI framework (e.g., VIRAL). The AI analyzes potential mutations and iteratively prioritizes the most concerning candidates for experimental screening [9].
- Experimental Validation: Conduct focused lab experiments (e.g., binding assays, neutralization tests) only on the high-priority variants identified by the AI, validating their fitness and immune evasion properties [9].
Workflow Visualization
AI-Driven Vaccine Strain Selection Workflow
Research Reagent Solutions
| Reagent / Resource | Function in Research | Key Consideration |
|---|---|---|
| Viral Sequence Databases (GISAID) | Provides the genomic data for surveillance, dominance calculation, and model training. | Data timeliness and global representation are critical for accurate forecasts [68]. |
| Hemagglutination Inhibition (HI) Assay | Generates gold-standard quantitative data on antigenic relationships for model training and validation. | Throughput is limited; best used to validate AI predictions rather than for primary screening [68]. |
| Post-Infection Ferret Antisera | Used in HI assays to measure antigenic relationships in a standardized, naive host model. | May not fully recapitulate the complex immunity of human populations [68]. |
| Protein Language Models | AI models that learn evolutionary constraints and relationships from protein sequences, used to build dominance predictors. | Must be adapted to model dynamic fitness landscapes, not just static properties [68]. |
| Biophysical Assays (Binding/Affinity) | Measures the functional impact of mutations (e.g., on receptor binding), providing data for forecasting models. | Essential for grounding AI predictions in real-world biological mechanisms [9]. |
Conclusion
The endeavor to predict viral evolution is steadily progressing from a reactive to a proactive science, driven by interdisciplinary approaches that fuse biophysics, AI, and virology. While foundational challenges like epistasis and stochasticity remain, advanced language models and unified deep learning frameworks demonstrate a remarkable capacity to anticipate high-risk variants, as validated by both retrospective analysis and experimental studies. The critical next steps involve overcoming data limitations, expanding models to encompass broader immune responses, and establishing robust, standardized validation pipelines. For biomedical and clinical research, the successful implementation of these predictive technologies promises a paradigm shift in pandemic preparedness, enabling the development of pre-emptive, broadly effective vaccines and therapeutics that can outmaneuver the viral arms race.
References
- 1. How mutational epistasis impairs predictability in protein ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4918425/]
- 2. Applications of Deep Mutational Scanning in Virology - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC8227372/]
- 3. Enriching productive mutational paths accelerates enzyme ... [https://www.nature.com/articles/s41589-024-01712-3]
- 4. The mutational landscape of SARS-CoV-2 provides new ... [https://www.nature.com/articles/s41467-025-61555-x]
- 5. Viral Evolution Core | Frederick National Laboratory [https://frederick.cancer.gov/node/528]
- 6. VIRUS-MVP: Frequently Asked Questions (FAQs) – virusmvp [https://virusmvp.org/faqs/]
- 7. Profiling of a Functional Protein... | PLOS Genetics Constraint Viral [https://journals.plos.org/plosgenetics/article?id=10.1371/journal.pgen.1005310]
- 8. in Innovation : viruses valley crossing, neutral landscapes, or... fitness [https://pmc.ncbi.nlm.nih.gov/articles/PMC11463231/]
- 9. New research: Forecasting the next variant [https://www.chemistry.harvard.edu/news/2025/07/new-research-forecasting-next-variant]
- 10. Biology Needs Evolutionary Software Tools: Let's Build ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC5967460/]
- 11. Epistasis and evolution: recent advances and an outlook for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10206586/]
- 12. The Evolution of Epistasis and Its Links With Genetic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC2674823/]
- 13. Towards evolutionary predictions: Current promises and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC9850016/]
- 14. Prediction of novel high-risk variants through co ... [https://www.sciencedirect.com/science/article/pii/S2405844025019498]
- 15. Environmental modulation of global epistasis in a drug ... [https://www.nature.com/articles/s41467-023-43806-x]
- 16. Researchers reveal a groundbreaking new theory ... [https://www.thebrighterside.news/post/researchers-reveal-a-groundbreaking-new-theory-of-evolution/]
- 17. Harnessing genotype-phenotype nonlinearity to accelerate ... [https://research.arcadiascience.com/pub/result-nonlinear-phenotypes]
- 18. A hybrid stochastic-deterministic approach to explore multiple ... [https://journals.plos.org/ploscompbiol/article?id=10.1371/journal.pcbi.1009713]
- 19. A hybrid stochastic-deterministic approach to explore ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8730440/]
- 20. Evidence for Recombination as an Evolutionary ... [https://www.frontiersin.org/journals/public-health/articles/10.3389/fpubh.2022.859900/full]
- 21. Recombination in viruses: Mechanisms, methods of study, and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC7106159/]
- 22. Stochastic Interplay between Mutation and Recombination ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC1262575/]
- 23. Five Challenges in the Field of Viral Diversity and Evolution [https://www.frontiersin.org/journals/virology/articles/10.3389/fviro.2021.684949/full]
- 24. Neoantigen Fitness Model Predicts Lower Immune ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6896054/]
- 25. Article Computationally designed proteins mimic antibody ... [https://www.sciencedirect.com/science/article/pii/S1074761325001785]
- 26. Balance of Evolutionary and Dynamic Adaptability in Shaping ... [https://pubmed.ncbi.nlm.nih.gov/40573332/]
- 27. Predicting pathogen evolution and immune evasion in the ... [https://www.sciencedirect.com/science/article/pii/S2001037025001138]
- 28. What will viruses do next? AI is helping scientists predict ... [https://www.nature.com/articles/d41586-024-04195-3]
- 29. MuTATE: an interpretable multi-endpoint machine learning ... [https://www.nature.com/articles/s44401-025-00025-4]
- 30. DeepHVI: A multimodal deep learning framework for ... [https://www.sciencedirect.com/science/article/pii/S2590053625000989]
- 31. Computational approaches for virus host prediction [https://arxiv.org/abs/2509.00349]
- 32. Integrating multi-omics and machine learning for disease ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12204941/]
- 33. 2025 Outlook: Emerging Viruses & Next-Gen Respiratory DX [https://meridianbioscience.com/lifescience-blog/emerging-viruses-next-generation-of-respiratory-diagnostics-2025-outlook/]
- 34. GenScript Life Science Research Grant Program 2025 [https://www.genscript.com/grantprogram-2025.html]
- 35. Closing the gap: the challenges in converging theoretical ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC4096944/]
- 36. A proposed workflow for proactive virus surveillance and ... [https://journals.plos.org/ploscompbiol/article?id=10.1371/journal.pcbi.1009624]
- 37. How Computational Design Can Predict the Next Viral ... [https://www.promegaconnections.com/computational-design-predict-viral-variant/]
- 38. Early detection of emerging viral variants through analysis ... [https://www.nature.com/articles/s41467-024-47304-6]
- 39. AI-driven epitope prediction: a systematic review ... - Nature [https://www.nature.com/articles/s41541-025-01258-y]
- 40. Computational tools for modern vaccine development - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7227725/]
- 41. Overcoming Data Bottlenecks in Genomic Pathogen ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC8634317/]
- 42. Challenges and Opportunities in Pathogen Agnostic ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10902267/]
- 43. Wastewater surveillance for viral pathogens: A tool ... [https://www.sciencedirect.com/science/article/pii/S2405844024099043]
- 44. Researchers create 'virtual scientists' to solve complex ... [https://med.stanford.edu/news/all-news/2025/07/virtual-scientist.html]
- 45. Exploring the emerging technologies and trends of infectious ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12187677/]
- 46. Role of antiviral CD8+ T cell immunity to SARS-CoV-2 ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11998524/]
- 47. T-cell responses induced by SARS-CoV-2 index-virus ... [https://www.nature.com/articles/s43856-025-00941-4]
- 48. Beyond T-cell subsets: stemness and adaptation redefining ... [https://www.nature.com/articles/s41423-025-01321-7]
- 49. Duolink® PLA故障排除指南 [https://www.sigmaaldrich.com/HK/zh/technical-documents/technical-article/protein-biology/protein-and-nucleic-acid-interactions/duolink-troubleshooting-guide?srsltid=AfmBOop31p6GfJ_YPIWhhnl8yw1C-OTjTLjqDxPzpulQDsBPm8y4Q-4V]
- 50. ViralFlow v1.0—a computational workflow for streamlining ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11127631/]
- 51. Integrating Computational and Experimental Workflows for ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC11468036/]
- 52. Computational approaches streamlining drug discovery [https://www.nature.com/articles/s41586-023-05905-z]
- 53. Predicting high-fitness viral protein variants with Bayesian ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12184641/]
- 54. A Guide to Developing Harmonized Research Workflows in ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12233188/]
- 55. Metadata practices for simulation workflows | Scientific Data [https://www.nature.com/articles/s41597-025-05126-1]
- 56. Navigating color integrity in data visualization - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11117063/]
- 57. Fitness models provide accurate short-term forecasts of SARS ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC10705624/]
- 58. Comparison of Filtering Methods for the Modeling and ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC3998879/]
- 59. Real-time estimates of the emergence and dynamics ... [https://www.sciencedirect.com/science/article/pii/S1755436524000665]
- 60. Pseudovirus-Based Neutralization Assays as ... [https://www.mdpi.com/2076-0817/14/11/1129]
- 61. Combining antigenic data from public sources gives an early indication... [https://www.nature.com/articles/s41598-025-19578-3?error=cookies_not_supported&code=df551826-a5db-4e07-9ee9-760a7522d3b6]
- 62. Evaluation of Measles Vaccine Immunogenicity and Durability Using... [https://weekly.chinacdc.cn/en/article/doi/10.46234/ccdcw2025.224]
- 63. Frontiers | Comparative analysis of neutralization assays performed... [https://www.frontiersin.org/journals/immunology/articles/10.3389/fimmu.2025.1650083/full]
- 64. Establishment of a pseudovirus neutralization assay for TGEV [https://pmc.ncbi.nlm.nih.gov/articles/PMC12018367/]
- 65. AI's Future Hinges On The Wet Lab [https://www.twistbioscience.com/blog/perspectives/AI-wetlab-validation]
- 66. Performance metrics for models designed to predict ... [https://pubmed.ncbi.nlm.nih.gov/37422647/]
- 67. CDC's Role in Tracking Variants | COVID-19 [https://www.cdc.gov/covid/php/variants/index.html]
- 68. Influenza vaccine strain selection with an AI-based ... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12618262/]