Evolutionary Modeling in Cancer Therapy: Overcoming Resistance through Darwinian Dynamics and Computational Approaches
This article provides a comprehensive analysis of evolutionary modeling as a transformative framework for understanding and overcoming cancer therapy resistance.
Evolutionary Modeling in Cancer Therapy: Overcoming Resistance through Darwinian Dynamics and Computational Approaches
Abstract
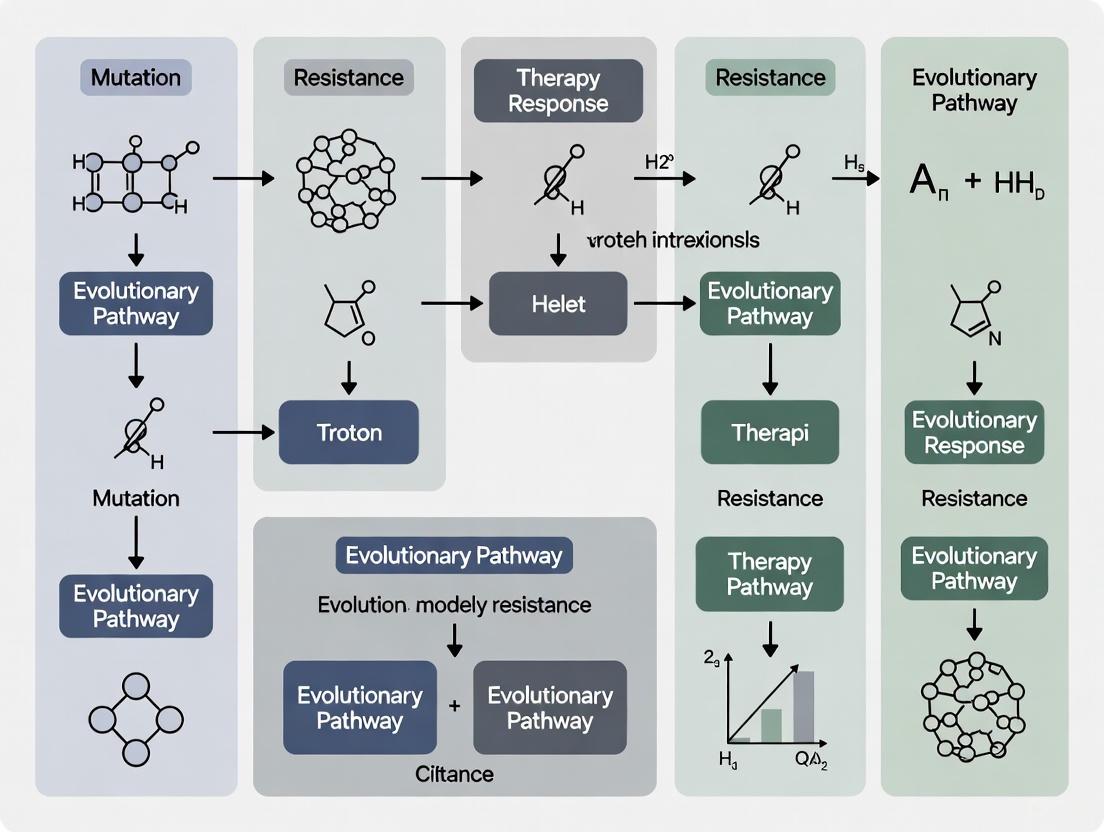
This article provides a comprehensive analysis of evolutionary modeling as a transformative framework for understanding and overcoming cancer therapy resistance. It explores the foundational principles of cancer as an eco-evolutionary process, where resistance develops through Darwinian selection pressures. The content examines cutting-edge methodological approaches, including adaptive therapy, evolutionary steering, and double-bind strategies that exploit fitness trade-offs. It addresses critical implementation challenges in clinical translation and validates these approaches through preclinical models and emerging clinical trial data. Designed for researchers, scientists, and drug development professionals, this synthesis bridges theoretical models with practical therapeutic applications, offering a paradigm shift from maximum cell kill to evolution-informed resistance management.
The Evolutionary Arms Race: Understanding Cancer as a Complex Adaptive System
Despite continuous deployment of new treatment strategies and agents over many decades, most disseminated cancers remain fatal. Cancer cells, through their access to the vast information of the human genome, have a remarkable capacity to deploy adaptive strategies for even the most effective treatments [1]. The clinical manifestation of treatment resistance requires two critical steps: first, the deployment of a resistance mechanism, and second, the proliferation of resistant cells to a population large enough to allow tumor progression [1]. While the emergence of resistance mechanisms is virtually inevitable due to the diversity of adaptive strategies available, the proliferation of resistant phenotypes is not—it depends on complex Darwinian dynamics governed by the costs and benefits of resistance mechanisms in the context of the local environment and competing populations [1].
The dynamic cancer ecosystem is extraordinarily robust to therapeutic perturbations due to cellular diversity, spatial and temporal heterogeneity in the tumor environment, and complex interactions with host cells [1]. Traditional maximum tolerated dose (MTD) strategies, while intuitively appealing, accelerate competitive release—a phenomenon wherein eliminating sensitive cells removes competition for resources, allowing resistant populations to expand rapidly [1]. This review explores the evolutionary principles underlying treatment failure and outlines novel therapeutic strategies that exploit Darwinian dynamics to delay or prevent resistance.
Theoretical Foundations: Evolutionary Dynamics in Cancer
Competitive Release and Its Therapeutic Implications
Competitive release occurs when intense Darwinian selection for resistant clones combined with elimination of all competing populations accelerates proliferation of resistant populations [1]. This evolutionary phenomenon is well-documented in pest management, where high-dose pesticide application promotes rapid emergence of uncontrollable, resistant strains [1]. Similarly, in oncology, MTD therapy imposes intense selection for resistant phenotypes while eliminating potential competitors.
Table 1: Comparison of Traditional MTD vs. Evolution-Informed Strategies
| Parameter | Maximum Tolerated Dose (MTD) | Adaptive Therapy | Extinction Therapy |
|---|---|---|---|
| Selection Pressure | High, continuous | Dynamic, responsive | Sequential, timed |
| Effect on Sensitive Cells | Complete elimination | Maintained at low levels | Initial reduction then strike |
| Effect on Resistant Cells | Competitive release | Suppressed by competition | Targeted at population nadir |
| Tumor Control Strategy | Maximum cell kill | Stable coexistence | Population extinction |
| Clinical Evidence | Standard of care for many cancers | Phase 2 trials in prostate cancer, melanoma [2] | Preclinical and theoretical models [3] [4] |
Evolutionary Rescue in Cancer Populations
Evolutionary rescue occurs when a population being driven toward extinction by environmental change adapts through beneficial alleles that permit recovery [4]. In cancer, the therapy represents the selective force driving extinction, while resistance mutations serve as the beneficial alleles. The hallmark of evolutionary rescue is a U-shaped trajectory of population size: initial rapid decline to a nadir, followed by renewed expansion [4]. The probability of evolutionary rescue depends on population size at treatment onset, therapy kill rate, and mutation rate for resistance alleles [4].
Diagram Title: Evolutionary Rescue vs. Extinction Pathways
Quantitative Models of Evolutionary Dynamics
Mathematical Framework for Evolutionary Rescue
The probability of tumor extinction under therapy can be modeled using evolutionary rescue theory. For a two-strike extinction therapy approach, the extinction probability PE(τ) is the product of probabilities of no evolutionary rescue due to standing genetic variation (PESGV) and de-novo mutations (PEDN) [3]:
PE(τ) = PESGV(τ) × PEDN(τ)
Where PESGV(τ) = exp[-πeR₂(τ)] represents rescue from pre-existing resistant cells, and PEDN(τ) = exp[-πe(∫₀τμ₂R₁(t)dt + ∫₀τμ₁R₂(t)dt) - πeμ₂(∫τ∞S(t)dt + ∫τ∞R₁(t)dt)] represents rescue from de-novo mutations arising during treatment [3].
Table 2: Key Parameters in Evolutionary Rescue Models
| Parameter | Symbol | Default Value | Biological Meaning |
|---|---|---|---|
| Carrying capacity | K | N(0) | Maximum population size supported by environment |
| Birth rate | b | 1.0 | Per capita birth rate of sensitive cells |
| Death rate | d | 0.1 | Per capita death rate of all cell types |
| Cost of resistance | c | 0.5 | Fitness cost of resistance mechanism in untreated environment |
| Mutation rate | μ₁, μ₂ | 2.5 × 10⁻⁶ | Rate of acquiring resistance to treatment 1 or 2 |
| Treatment-induced death | δ₁, δ₂ | 2.0 | Additional death rate due to treatment 1 or 2 [3] |
G-Function Framework for Evolutionary Dynamics
The G-function approach in evolutionary game theory provides a unified framework for modeling population and strategy dynamics simultaneously [5]. The fitness-generating function G(v,u,x)∣ᵥ=ᵤᵢ describes the per capita growth rate of individuals with strategy v=uᵢ, where u represents the strategy vector of all populations and x represents their densities [5]. Darwinian dynamics then follow:
dxᵢ/dt = xᵢ × G(v,u,x)∣ᵥ=ᵤᵢ
duᵢ/dt = σᵢ² × ∂G(v,u,x)/∂v∣ᵥ=ᵤᵢ
Where σᵢ² represents the variance of strategic traits in population i, driving evolutionary change [5].
Application Notes & Experimental Protocols
Protocol: In Silico Evaluation of Extinction Therapy Timing
Purpose: To determine the optimal switching time from first-line to second-line treatment in a two-strike extinction therapy protocol [3] [4].
Background: Evolutionary rescue theory suggests that small populations are vulnerable to stochastic extinction and less capable of adapting to environmental changes. The "second strike" should be delivered when the tumor population is at or near its minimum size, which may occur when the tumor is undetectable by conventional imaging [3].
Diagram Title: Extinction Therapy Simulation Workflow
Procedure:
Model Setup:
- Initialize a population of 10⁶ treatment-sensitive cells (S) with small subpopulations (∼100 cells each) of variants resistant to treatment 1 (R₁) and treatment 2 (R₂) [3].
- Set mutation rates for acquiring resistance (default μ₁ = μ₂ = 2.5×10⁻⁶) [3].
- Define fitness costs of resistance (default c = 0.5) and treatment-induced death rates (default δ₁ = δ₂ = 2.0) [3].
Simulation Execution:
- Apply first treatment (strike 1) and simulate population dynamics using either differential equations or stochastic agent-based models.
- Calculate extinction probability PE(τ) for potential switching times τ using evolutionary rescue theory.
- Identify optimal switching time τ* that maximizes PE(τ).
- Apply second treatment (strike 2) at time τ* and continue simulation until extinction, persistence, or progression occurs.
Outcome Assessment:
- Record time to extinction for successful simulations.
- For failures, record whether rescue occurred through standing genetic variation or de-novo mutation.
- Perform sensitivity analysis on key parameters (mutation rates, fitness costs, carrying capacity).
Validation: Compare model predictions with in vitro experiments using cancer cell lines with engineered resistance markers [6].
Protocol: Adaptive Therapy Dose Modulation Based on Evolutionary Game Theory
Purpose: To maintain stable tumor burden by dynamically adjusting treatment doses to preserve treatment-sensitive cells that suppress growth of resistant populations [1] [2].
Background: Adaptive therapy exploits competitive interactions between drug-sensitive and drug-resistant cancer cells. By maintaining a population of sensitive cells, resistant cells remain suppressed due to competition for resources [1].
Procedure:
Therapeutic Monitoring:
Dose Modulation Algorithm:
- When tumor burden decreases by 50% from baseline, pause treatment [2].
- Monitor tumor burden regularly (frequency depends on cancer type and biomarker kinetics).
- When tumor burden returns to baseline, reinitiate treatment.
- For dose modulation (alternative to on/off cycling), adjust dose to maintain tumor burden within a stable window (e.g., ±25% of target burden).
Long-term Management:
- Continuously monitor for signs of escape (rapid growth despite treatment).
- If escape occurs, consider switching to alternative therapeutic strategy.
Clinical Validation: In a clinical trial of metastatic castrate-resistant prostate cancer, adaptive therapy based on this protocol increased median time to progression from 16.5 to 27 months while reducing cumulative drug dose to 47% of standard dosing [2].
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Evolutionary Therapy Studies
| Reagent/Resource | Function | Example Applications |
|---|---|---|
| Beyondcell [6] | Computational method for identifying tumor cell subpopulations with distinct drug responses in single-cell RNA-seq data | Detecting therapeutic clusters in heterogeneous tumors; predicting drug sensitivity patterns |
| SLiM 4.0 [4] | Agent-based evolutionary simulation platform | Modeling clonal evolution and resistance emergence with minimal mathematical assumptions |
| Drug Perturbation Signature Collection (PSC) [6] | Collection of drug-induced expression signatures from LINCS database | Predicting transcriptional responses to treatments; identifying signature reversals |
| Drug Sensitivity Signature Collection (SSC) [6] | Collection of sensitivity signatures from CCLE, GDSC, CTRP | Predicting innate drug sensitivity based on pre-treatment transcriptional state |
| bollito pipeline [6] | Automated scRNA-seq processing pipeline | Cell filtering, normalization, integration, and differential expression analysis |
| Evolutionary Game Theory G-Function Framework [5] | Mathematical framework for coupled ecological and evolutionary dynamics | Modeling population and strategy dynamics of sensitive and resistant cell populations |
Discussion: Clinical Translation and Future Directions
While evolutionary-based therapy approaches show promise, clinical implementation faces several challenges. These include communication barriers between modelers and clinicians, limited trust in mathematical models, increased requirements for disease monitoring, and cultural resistance to outsider ideas in the medical field [2]. However, ongoing clinical trials in prostate cancer, melanoma, and other solid tumors are generating crucial validation data [2].
Future research directions should focus on:
- Developing better biomarkers for real-time monitoring of tumor evolutionary dynamics
- Creating standardized computational platforms for translating evolutionary models into clinical decision support
- Designing clinical trials that incorporate evolutionary principles into combination therapy sequencing
- Integrating single-cell technologies with evolutionary models to predict and prevent resistance
The Darwinian dynamics of treatment failure—from competitive release to evolutionary rescue—provide both an explanation for past therapeutic failures and a roadmap for designing more evolutionarily informed treatment strategies that delay or prevent resistance by working with, rather than against, evolutionary principles.
This application note addresses a fundamental limitation in cancer therapy resistance research: the traditional focus on molecular mechanisms fails to distinguish between the emergence of resistant clones and their subsequent proliferation. We posit that overcoming this limitation requires integrating evolutionary biology principles with advanced single-cell technologies. The protocols herein provide a framework for tracking resistance dynamics and quantifying evolutionary bottlenecks, enabling researchers to design therapeutic strategies that suppress the expansion of resistant populations, not just target their molecular machinery.
Table 1: Key Concepts in Evolutionary Therapy Resistance
| Concept | Traditional Molecular View | Evolutionary Dynamics View |
|---|---|---|
| Resistance Origin | Primarily acquired through new mutations during treatment [8] | Pre-existing in heterogeneous tumors due to intratumoral diversity [9] [10] |
| Therapeutic Goal | Block specific resistance pathways (e.g., efflux pumps, bypass signaling) [8] | Control the eco-evolutionary dynamics of the entire tumor population to suppress resistant clone proliferation [10] |
| Tumor Model | A homogeneous entity with uniform response | A diverse ecosystem of competing and cooperating subclones [9] [11] |
| Primary Challenge | Bypass molecular redundancy | Anticipate and steer evolutionary trajectories [10] |
Cancer drug resistance is estimated to account for approximately 90% of cancer-related deaths [11]. While molecular biology has successfully identified a vast array of resistance mechanisms—including drug efflux, evasion of apoptosis, and DNA damage repair [8]—clinical strategies designed to directly inhibit these mechanisms have seen limited success. A key reason is that cancer is not a static disease but an evolutionary system. In large, diverse cancer cell populations, the emergence of resistant phenotypes is virtually inevitable [10]. Therefore, the critical clinical event is not the initial appearance of a resistant cell, but its ability to proliferate and dominate the tumor ecosystem.
The advent of single-cell transcriptomics (SCT) has starkly revealed the limitations of bulk analysis, which averages gene expression and obscures rare, therapy-resistant subpopulations such as cancer stem-like cells and drug-tolerant persisters [9]. This note provides practical protocols to leverage SCT and evolutionary modeling, moving beyond cataloging mechanisms to actively managing the dynamics of resistance.
Quantitative Foundations: Mapping the Resistance Landscape
A quantitative understanding of resistance is the first step toward controlling it. The following table synthesizes key resistance data across cancer types and therapies, highlighting the pervasiveness of the challenge.
Table 2: Quantitative Landscape of Therapy Resistance
| Cancer Type / Therapy | Resistance Metric | Key Findings / Mechanisms | Citation |
|---|---|---|---|
| Advanced HCC (Sorafenib) | ~60-70% innate resistance; 30-40% acquire resistance within 6 months | Dysregulated drug transporters, metabolic reprogramming, TME interactions [12] | |
| Lung Cancer (PD-1/PD-L1 Inhibitors) | >60% develop acquired resistance | Tumor microenvironment (TME), autophagy, ferroptosis, T-cell exhaustion [13] | |
| Metastatic Breast Cancer | 30% of early-stage cases progress to metastatic disease | Transcriptional reprogramming, survival of drug-tolerant subpopulations, immune evasion [9] | |
| Pan-Cancer Analysis | Resistance causes ~90% of cancer deaths | Multifactorial: tumor heterogeneity, phenotypic plasticity, apoptotic evasion [8] [11] |
Core Protocol: Tracking Resistant Clone Dynamics with scRNA-seq
This protocol details the use of single-cell RNA sequencing to decouple the emergence of resistant cells from their proliferation over the course of therapy.
Materials and Reagents
Table 3: Research Reagent Solutions for scRNA-seq
| Item | Function | Example Product(s) |
|---|---|---|
| Viability Stain | Distinguish live cells for sequencing | Propidium Iodide, DAPI |
| Single-Cell Suspension Kit | Dissociate tumor tissue into viable single cells | Miltenyi Biotec Tumor Dissociation Kits |
| scRNA-seq Platform | High-throughput single-cell capture and barcoding | 10x Genomics Chromium |
| Cell Hashtag Antibodies | Multiplex samples by tagging cells with sample-specific barcoded antibodies | BioLegend TotalSeq-A |
| RT-PCR Reagents | Amplify cDNA from single cells | SMART-Seq v4 Ultra Low Input RNA Kit |
| Bioinformatics Tools | Data processing, clustering, and trajectory inference | CellRanger, Seurat, Monocle |
Step-by-Step Procedure
Experimental Design & Sample Collection:
- Cohort: Establish a murine model or patient-derived xenograft (PDX) for the cancer type of interest.
- Time Points: Collect tumor biopsies or dissociated tumors at critical time points:
- T0: Baseline, pre-treatment.
- T1: Early on-treatment (e.g., after first cycle).
- T2: At minimal residual disease (MRD).
- T3: Upon clinical/radiographic progression.
- Sample Multiplexing: Label cells from different time points with unique Cell Hashtag Antibodies to pool samples for a single library preparation, reducing batch effects.
Single-Cell Library Preparation & Sequencing:
- Tissue Dissociation: Process tumor samples into high-viability (>90%) single-cell suspensions using a gentle, optimized Single-Cell Suspension Kit.
- Cell Capture & Barcoding: Load the cell suspension onto a 10x Genomics Chromium platform to partition individual cells into nanoliter-scale droplets with barcoded beads.
- Library Construction: Perform reverse transcription, cDNA amplification, and library construction according to the manufacturer's protocol. Sequence libraries on an appropriate Illumina platform to a minimum depth of 50,000 reads per cell.
Bioinformatic Analysis of Resistance Trajectories:
- Primary Processing: Use CellRanger to align reads, generate feature-barcode matrices, and perform initial quality control.
- Dimensionality Reduction & Clustering: In R/Python, use Seurat to normalize data, identify highly variable genes, perform PCA, and cluster cells using a graph-based algorithm (e.g., Louvain). Visualize clusters in 2D using UMAP.
- Differential Expression & Phenotyping: Identify marker genes for each cluster. Annotate cell types (e.g., malignant, T-cell, fibroblast) and, within the malignant cluster, identify subpopulations expressing resistance signatures (e.g., EMT, stemness, oxidative phosphorylation).
- Trajectory Inference: Utilize Monocle 3 or Slingshot to reconstruct the lineage relationships between cell states. This will infer the potential evolutionary paths from treatment-sensitive to resistant states.
Supporting Protocol: Modeling Evolutionary Bottlenecks
Mathematical modeling is required to translate single-cell data into testable evolutionary hypotheses.
Materials and Computational Tools
- Software: R or Python programming environment.
- Key Packages:
ape(R) for phylogenetics,deSolve(R) for solving differential equations, or custom stochastic simulation code. - Input Data: The cellular lineage and abundance data generated from Protocol 1, Section 4.2.
Step-by-Step Procedure
Construct a Clonal Phylogeny:
- Use the trajectory inference results from Monocle 3 as a scaffold. Alternatively, infer a phylogenetic tree from the single-cell genotyping data (if available) using tools like
ape.
- Use the trajectory inference results from Monocle 3 as a scaffold. Alternatively, infer a phylogenetic tree from the single-cell genotyping data (if available) using tools like
Parameterize a Population Dynamics Model:
- Model the tumor as a system of ordinary differential equations where each compartment represents a distinct subclone (e.g., Sensitive, Drug-Tolerant Persister, Fully Resistant).
dS/dt = r_S * S * (1 - (S + D + R)/K) - d_S * S - δ * SdD/dt = r_D * D * (1 - (S + D + R)/K) + δ * S - d_D * D - ε * DdR/dt = r_R * R * (1 - (S + D + R)/K) + ε * D - d_R * R- Where S, D, R are population sizes of Sensitive, Drug-Tolerant Persister, and Resistant clones; r is growth rate; d is death rate (therapy-induced); K is carrying capacity; and δ, ε are transition rates.
Identify and Target the Bottleneck:
- Fit the model parameters to your time-course scRNA-seq data. The goal is to identify the critical bottleneck in the expansion of the resistant population—is it the initial transition to a persister state (δ) or the subsequent acquisition of full resistance (ε)?
- Design a combination therapy where a second agent specifically targets this bottleneck, for example, by increasing the death rate of the persister population (d_D).
Data Interpretation and Integration
The power of this approach lies in synthesizing data from both protocols.
- Correlate Molecular State with Fitness: The scRNA-seq data (Protocol 1) reveals the molecular identity of the resistant persister and fully resistant clones. The evolutionary model (Protocol 2) quantifies their fitness (growth and death rates) under therapeutic pressure.
- Predict and Intervene: Use the parameterized model to simulate the effects of different combination therapy schedules in silico before moving to in vivo validation. The goal is to identify strategies, such as adaptive therapy, which cycles or modulates drug doses to maintain a population of sensitive cells that can outcompete resistant clones [10].
Application Note
This document provides a structured experimental framework for investigating non-genetic cancer therapy resistance. It outlines defined protocols to dissect the contributions of epigenetic plasticity and the tumor microenvironment (TME) in fostering drug-tolerant persister (DTP) states and sanctuary niches, supporting the development of evolutionary-driven therapeutic models.
Acquired therapeutic resistance remains the primary cause of treatment failure in advanced cancers. While genetic evolution provides a foundational mechanism, non-genetic adaptation—driven by dynamic epigenetic reprogramming and protective microenvironmental niches—confers a rapid, adaptive survival advantage [14] [15]. This application note details methodologies to profile and target these landscapes, focusing on the spatial-epigenetic axis where specific TME niches impose selective pressures that reshape the epigenetic state of resident cancer cells, and vice versa [16].
Key Mechanistic Insights and Associated Quantitative Data
The following table summarizes core epigenetic resistance mechanisms operational within distinct tumor niches, as identified in recent preclinical and clinical studies (2019-2024) [16].
Table 1: Niche-Specific Epigenetic Resistance Mechanisms
| Tumor Niche | Key Epigenetic Axis | Functional Outcome | Quantitative Effect on Resistance | Potential Therapeutic Intervention |
|---|---|---|---|---|
| Hypoxic Core | HIF-1α–SIRT1 | Quiescence, reduced apoptosis | 50-70% reduction in pro-apoptotic gene (e.g., p21, BAX) expression; 2.3-fold reduction in apoptosis under hypoxia [16]. | SIRT1 inhibitors (e.g., EX-527); HIF-1α inhibitors (e.g., PX-478) |
| Invasive Edge | EZH2–H3K27me3 | Proneural-to-Mesenchymal Transition (PMT), plasticity & motility | 2.3-fold higher EZH2 expression; 1.9-fold higher H3K27me3 levels at differentiation gene promoters [16]. | EZH2 inhibitors (e.g., GSK126) |
| Perivascular Niche (PVN) | BRD4–Super-Enhancer (SE); HDAC–DNA Repair | Stemness maintenance, pro-survival transcription | Specific quantitative data not provided in search results, but mechanisms are noted as critical for sustaining GIC populations [16]. | BET inhibitors (e.g., JQ1); HDAC inhibitors |
Experimental Protocols for Deconvolving Resistance Mechanisms
Protocol 1: Spatial Profiling of Epigenetic and Transcriptomic States
Objective: To map epigenetic and gene expression heterogeneity across defined tumor microenvironments (hypoxic core, invasive edge, perivascular niche) from patient-derived samples.
Materials:
- Fresh or optimally preserved frozen GBM tissue sections.
- Spatial transcriptomics platform (e.g., 10x Visium).
- Antibodies for immunohistochemistry (IHC) against niche markers (e.g., CA9 for hypoxia, CD93 for PVN).
- Epigenetic analysis kits (e.g., CUT&Tag for H3K27me3, DNA methylation arrays).
Workflow Diagram: Spatial Multi-omics Profiling
Method Steps:
- Tissue Preparation: Section tissue onto slides compatible with IHC, laser capture microdissection (LCM), and spatial transcriptomics.
- Niche Identification: Perform IHC staining for established niche markers (e.g., hypoxia, vasculature) to guide region selection.
- Region-Specific Isolation:
- Use LCM to isolate cells from specific niches (hypoxic core, invasive edge, PVN) identified in step 2.
- Extract DNA and RNA from these isolated populations for bulk analysis.
- Genome-Wide Profiling:
- Subject DNA to genome-wide methylation analysis (e.g., Illumina EPIC array).
- Subject RNA to bulk RNA-seq or single-cell RNA-seq (scRNA-seq) for transcriptomic clustering and trajectory inference [9].
- Spatial Validation: Perform spatial transcriptomics on serial sections to validate and spatially resolve the identified expression patterns.
- Data Integration: Use bioinformatic tools (e.g., CellPhoneDB, NicheNet) to integrate DNA methylation, chromatin accessibility, transcriptomic data, and spatial coordinates to define niche-specific epigenetic signatures [16] [9].
Protocol 2: Functional Validation of Epigenetic Targets Using Patient-Derived Models
Objective: To test the efficacy of niche-specific epigenetic inhibitors as radiosensitizers in patient-derived glioblastoma organoids (GBOs).
Materials:
- Patient-derived glioma-initiating cells (GICs).
- Organoid culture media and matrices.
- Epigenetic inhibitors: EX-527 (SIRT1i), GSK126 (EZH2i), JQ1 (BETi).
- Irradiator.
- Viability assay kits (e.g., CellTiter-Glo).
- Flow cytometry antibodies for apoptosis and cell cycle analysis.
Workflow Diagram: Functional Validation in GBOs
Method Steps:
- GBO Generation: Culture and expand GICs in a 3D extracellular matrix to form GBOs that recapitulate tumor heterogeneity [14] [15].
- Epigenetic Pre-treatment: Treat GBOs with a niche-targeting epigenetic inhibitor (e.g., SIRT1i for hypoxic core) for 24-48 hours. Include vehicle control.
- Therapy Challenge: Subject pre-treated and control GBOs to a clinically relevant dose of radiation (e.g., 2-6 Gy).
- Phenotypic Readout:
- Viability: Quantify cell viability 72-96 hours post-radiation using a luminescent ATP-based assay.
- Apoptosis and Cell Cycle: Dissociate GBOs and analyze by flow cytometry for Annexin V/PI staining and DNA content.
- Stemness and Differentiation: Analyze the expression of key markers (e.g., SOX2, OLIG2, MES markers) via qRT-PCR or immunofluorescence.
- Data Analysis: Compare viability, apoptosis, and marker expression between inhibitor+radiation and radiation-only groups to determine the degree of radiosensitization.
The Scientist's Toolkit: Research Reagent Solutions
Table 2: Essential Reagents for Investigating Epigenetic Plasticity
| Reagent / Tool | Function / Target | Example Product/Code | Application Context |
|---|---|---|---|
| SIRT1 Inhibitor | Pharmacological inhibition of SIRT1 deacetylase activity | EX-527 (Selisistat) | Target quiescence and radioresistance in hypoxic core niches [16]. |
| EZH2 Inhibitor | Pharmacological inhibition of EZH2 methyltransferase activity | GSK126, Tazemetostat | Suppress proneural-to-mesenchymal transition (PMT) at invasive edges [16]. |
| BET Inhibitor | Displacement of BRD4 from super-enhancers | JQ1, I-BET151 | Target stemness and pro-survival programs in perivascular niches [16]. |
| Single-Cell RNA-seq Kit | High-throughput transcriptomic profiling of individual cells | 10x Genomics Chromium Single Cell 3' Kit | Deconvolve tumor heterogeneity, identify rare subpopulations, and infer lineage trajectories [9]. |
| Patient-Derived Organoids | Physiologically relevant 3D ex vivo tumor models | N/A (Established in-house from patient samples) | Functional validation of targets and combination therapy testing in a preserved TME context [14]. |
| Cell-Cell Communication Tools | Bioinformatics inference of ligand-receptor interactions | CellPhoneDB, NicheNet | Analyze signaling between tumor niches and stromal/immune cells from transcriptomic data [9]. |
Visualization of Core Signaling Pathways
The following diagram illustrates the key niche-specific epigenetic axes that drive therapy resistance in glioblastoma, as detailed in Table 1.
Pathway Diagram: Epigenetic Resistance Axes in GBM Niches
The evolution of therapy resistance is the primary cause of treatment failure in advanced cancers, yet the emergence of resistant cells does not automatically lead to clinical progression. Resistance mechanisms impose fitness costs on cancer cells—metabolic burdens and functional compromises that reduce competitiveness in the absence of therapeutic pressure [1]. These inherent trade-offs create critical evolutionary vulnerabilities that can be exploited through novel treatment paradigms. While conventional maximum tolerated dose (MTD) chemotherapy accelerates competitive release of resistant populations by eliminating sensitive competitors, evolutionary-inspired approaches aim to control tumor burden by maintaining a stable population of therapy-sensitive cells that can suppress the expansion of less-fit resistant variants [1] [17].
Understanding these fitness trade-offs requires examining the molecular machinery of resistance, including the synthesis and operation of drug efflux pumps, enhanced DNA repair systems, and alternative signaling pathways. Each mechanism diverts finite cellular resources from proliferation and survival functions, creating quantifiable deficits in growth kinetics and competitive fitness [1]. This application note provides experimental frameworks for quantifying these costs and implementing evolution-informed treatment protocols that transform resistance management in cancer therapy.
Quantitative Profiling of Resistance Costs
Metabolic and Proliferation Costs of Common Resistance Mechanisms
Table 1: Experimentally Measured Fitness Costs of Resistance Mechanisms
| Resistance Mechanism | Experimental Model | Proliferation Rate Reduction | Metabolic Cost | Key Measurable Parameters |
|---|---|---|---|---|
| P-glycoprotein (P-gp) Overexpression | MCF-7 breast cancer cells | 15-25% in drug-free medium [18] | Increased ATP consumption from drug efflux [18] | Growth rate, intracellular ATP levels, glucose uptake |
| Enhanced DNA Repair Capacity | Colorectal cancer models with Dicer upregulation | 10-20% under non-stress conditions [18] | Upregulation of repair enzyme synthesis [18] | NHEJ efficiency, ROS sensitivity, replication speed |
| Androgen-Independent Signaling | Prostate cancer LNCaP cells | 30-40% in androgen-rich environments [17] | Alternative pathway maintenance [17] | PSA production rate, testosterone dependence |
| CYP17A1 Overexpression | mCRPC models | 20-30% in low-androgen conditions [17] | De novo androgen synthesis [17] | Testosterone production, growth in castrate conditions |
The fitness costs quantified in Table 1 demonstrate that resistance mechanisms impose substantial burdens on cancer cells, which can be measured through specific experimental approaches. For P-glycoprotein overexpression, the continuous ATP consumption required for drug efflux reduces the energy available for proliferation and biomass production [18]. Similarly, cells with enhanced DNA repair capacity must allocate resources to the synthesis and maintenance of repair complexes, creating a metabolic drain that becomes particularly evident in nutrient-limited conditions [18]. The costs of alternative signaling pathway activation, such as androgen-independent progression in prostate cancer, manifest as reduced growth rates when the original signaling ligand is abundant [17].
Figure 1: Fitness Cost Dynamics in Resistance. This diagram illustrates the causal pathway through which resistance mechanisms impose metabolic costs that lead to competitive disadvantages, particularly during treatment holidays when therapy-sensitive cells can expand.
Protocol: Measuring Competitive Fitness in Co-culture Models
Objective: Quantify the fitness differences between therapy-sensitive and resistant cell populations in drug-free conditions using fluorescent tracking and growth kinetics.
Materials:
- Fluorescently tagged cell lines: GFP-labeled sensitive cells and RFP-labeled resistant variants
- Flow cytometry system: For precise quantification of population ratios
- Time-lapse imaging: IncuCyte or similar system for kinetic growth monitoring
- Metabolic assay kits: ATP quantification, glucose consumption measurements
Procedure:
- Establish co-cultures at defined ratios (start with 1:1, 1:9, and 9:1 sensitive:resistant mixtures)
- Maintain in drug-free medium for 14 days with regular passaging to prevent confluence
- Sample every 48-72 hours for flow cytometry analysis to determine population proportions
- Measure metabolic parameters at days 0, 7, and 14 (ATP levels, glucose consumption, lactate production)
- Calculate competitive fitness index using the formula: Fitness = ln(Rf/Ri) / ln(Sf/Si) Where Rf and Ri are final and initial resistant populations, Sf and Si are final and initial sensitive populations
Data Interpretation: A fitness index <1 indicates resistant cells are less fit than sensitive counterparts. Significant differences in metabolic parameters help explain the mechanistic basis for observed fitness differences.
Evolutionary Therapy Protocols
Adaptive Therapy Scheduling Based on Tumor Dynamics
Table 2: Adaptive Therapy Protocol Parameters from Clinical Evidence
| Parameter | Standard MTD Approach | Evolutionary Adaptive Therapy | Biological Rationale |
|---|---|---|---|
| Dosing Strategy | Continuous at maximum tolerated dose | Drug holidays/interruptions based on tumor marker thresholds [17] | Maintains population of sensitive cells to suppress resistant expansion |
| Treatment Trigger | Fixed schedule | PSA or other biomarker increase to predetermined level (e.g., 50% above nadir) [17] | Allows controlled tumor growth while preventing resistant takeover |
| Dose Adjustment | Fixed dose based on BSA | Variable dose based on tumor response dynamics [1] | Minimizes selection pressure while maintaining control |
| Cycle Duration | Fixed intervals | Patient-specific based on tumor growth kinetics [17] | Accommodates inter-patient heterogeneity in evolutionary dynamics |
| Cumulative Drug Exposure | 100% of standard dosing | 47% average reduction reported in clinical trial [17] | Reduces toxicity and treatment costs while maintaining efficacy |
The adaptive therapy approach outlined in Table 2 represents a fundamental shift from conventional cancer treatment paradigms. Rather than attempting to eradicate all cancer cells—an approach that inevitably selects for resistant populations—evolutionary therapy aims for stable tumor control by leveraging the fitness costs of resistance [1]. Clinical trials in metastatic castrate-resistant prostate cancer have demonstrated that this approach can extend time to progression from 16.5 months with standard care to at least 27 months while reducing cumulative drug exposure by 53% [17]. Similar principles have shown promise in preclinical models of breast and ovarian cancers [1].
Figure 2: Adaptive Therapy Workflow. This diagram outlines the decision-making process in evolutionary-informed adaptive therapy, showing how treatment cycles are guided by biomarker monitoring to maintain competitive suppression of resistant cells.
Protocol: Implementing Adaptive Therapy in Preclinical Models
Objective: Establish and validate evolutionary therapy protocols in patient-derived xenograft (PDX) models that mimic the clinical adaptive therapy approach.
Materials:
- PDX models: Characterized for therapy sensitivity and resistance markers
- Bioluminescence imaging: For non-invasive tumor burden monitoring
- Drug formulations: Clinical-grade chemotherapeutic or targeted agents
- Statistical software: For modeling tumor growth dynamics and determining treatment thresholds
Procedure:
- Establish baseline growth kinetics: Monitor untreated tumor growth for 14 days to establish doubling time and growth patterns
- Initiate treatment at standard doses until 50% reduction in tumor burden (or biomarker level) is achieved
- Withhold treatment and monitor tumor regrowth, measuring growth rate acceleration
- Reinitiate treatment when tumor burden reaches 75-90% of initial pretreatment volume
- Continue cycles of treatment and holidays, adjusting thresholds based on observed dynamics
- Compare outcomes against continuous MTD treatment in control cohorts
Endpoint Analysis:
- Time to progression: Defined as tumor volume exceeding predetermined threshold despite treatment
- Cumulative drug exposure: Total dose administered across treatment period
- Resistant subpopulation quantification: IHC or flow cytometry for resistance markers at endpoint
- Survival analysis: Progression-free and overall survival compared between strategies
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents for Fitness Cost Investigation
| Reagent/Cell Line | Manufacturer/Model | Research Application | Key Functional Assessment |
|---|---|---|---|
| MDR1-GFP Reporter Cells | ATCC MDR1-MDCK-II | P-gp expression and function quantification | Drug efflux capacity, ATP consumption during transport |
| Isogenic Sensitive/Resistant Pairs | NCI-60 resistant variants | Controlled comparison of fitness costs | Growth kinetics, metabolic profiling in matched genetic backgrounds |
| CSC Marker Antibody Panels | BD Biosciences CSC Detection Kit | Cancer stem cell population tracking | ALDH1, CD44, CD133 expression in resistant vs. sensitive cells |
| Seahorse XF Analyzer Kits | Agilent Technologies | Real-time metabolic phenotyping | Glycolytic stress tests, mitochondrial function assays |
| PSA/LDH ELISA Kits | Roche Diagnostics | Tumor burden and cytotoxicity monitoring | Biomarker tracking for adaptive therapy decision points |
| IncuCyte Live-Cell Analysis | Sartorius IncuCyte S3 | Kinetic growth and competition assays | Long-term co-culture monitoring without manual sampling |
The strategic exploitation of fitness trade-offs represents a paradigm shift in cancer therapy that moves beyond direct cytotoxic approaches to encompass evolutionary control strategies. The experimental protocols and analytical frameworks presented here provide researchers with standardized methods to quantify resistance costs and implement evolutionary therapy approaches across different cancer models. By focusing on the dynamic equilibrium between sensitive and resistant populations rather than maximal cell kill, these approaches transform resistance management from reactive to proactive. Clinical validation in prostate cancer demonstrates that evolutionary therapies can simultaneously improve disease control while reducing treatment exposure [17], establishing a compelling framework for broader application across cancer types. The research tools and experimental protocols outlined provide a foundation for expanding this approach to breast, ovarian, and other malignancies where resistance drives mortality.
Cancer therapy, much like traditional pest management, is fundamentally an evolutionary challenge. The prevailing paradigm in oncology has long been the application of maximum tolerated doses (MTD) of cytotoxic agents to achieve maximal cell kill [1]. However, this approach virtually always fails in metastatic disease due to the inevitable emergence of treatment-resistant populations [1] [19]. This failure mirrors historical experiences in agriculture, where high-dose pesticide applications initially achieved impressive pest reduction but ultimately led to rapid evolution of resistant strains that became uncontrollable [1]. The parallel is not merely metaphorical; the Darwinian dynamics governing pest resistance and cancer treatment resistance share fundamental principles that can be leveraged to develop more sustainable therapeutic approaches.
Integrated Pest Management (IPM) emerged as an ecological solution to this agricultural challenge, shifting focus from eradication to sustainable management through a combination of biological understanding, controlled intervention, and environmental modification [1]. Similarly, eco-oncology applies ecological and evolutionary principles to understand and manage cancer as a complex, adaptive system [20] [21]. Tumors exhibit remarkable spatial and temporal heterogeneity, continually interact with their microenvironment, and evolve through natural selection to increase cellular fitness [20]. Viewing cancers through this ecological lens provides a framework for developing evolutionarily informed treatment strategies that delay or prevent resistance by managing, rather than attempting to eradicate, the cancer ecosystem.
Table 1: Core Parallels Between Agricultural IPM and Cancer Therapy
| Integrated Pest Management Principle | Oncology Analogue | Therapeutic Implication |
|---|---|---|
| Avoid high-dose eradication strategies | Move beyond maximum tolerated dose | Prevent competitive release of resistant subclones |
| Maintain susceptible populations | Preserve treatment-sensitive cells | Utilize adaptive therapy to maintain competition |
| Combine multiple control strategies | Implement combination therapies | Target multiple vulnerabilities simultaneously |
| Modify environment to disfavor pests | Alter tumor microenvironment | Disrupt ecological niches supporting resistance |
| Monitor populations and adapt strategies | Track tumor evolution longitudinally | Employ treatment switching based on resistance detection |
Theoretical Foundation: Ecological Principles Applied to Cancer
The Competitive Release Phenomenon in Cancer Ecosystems
In ecology, competitive release occurs when intense selection pressure eliminates competing populations, allowing a previously suppressed species to expand rapidly [1]. The precise same phenomenon occurs in cancer treatment when MTD chemotherapy eliminates drug-sensitive cells, thereby removing competition and creating ecological space for resistant subclones to proliferate [1]. This dynamic explains why tumors often regrow more aggressively after an initial response to therapy, with resistant populations now dominating the cancer ecosystem.
The clinical manifestation of competitive release is treatment failure due to acquired resistance. Studies tracking the evolution of metastatic breast cancer through serial sampling have demonstrated that as therapy-sensitive cells are eliminated, resistant subclones undergo population bottlenecks followed by expansion to become the dominant populations [22]. This evolutionary trajectory follows a predictable pattern across cancer types, with resistant phenotypes relying on common signaling pathways despite heterogeneous genetic backgrounds [22].
Fitness Costs and Therapeutic Opportunities
A critical insight from ecology is that resistance mechanisms typically incur fitness costs—metabolic burdens or functional trade-offs that reduce competitive ability in the absence of the selective pressure [1]. In cancer, resistance mechanisms such as upregulated drug efflux pumps or enhanced DNA repair capacity consume cellular resources that would otherwise be allocated to proliferation. These fitness costs create therapeutic opportunities to manage, rather than eradicate, cancer populations by maintaining sensitive cells that can outcompete resistant variants in drug-free intervals or under modified selective pressures.
The eco-evolutionary perspective suggests that although emergence of resistance mechanisms to every current therapy is inevitable, proliferation of the resistant phenotypes is not inevitable and can be delayed or prevented with sufficient understanding of the underlying eco-evolutionary dynamics [1]. This represents a fundamental shift from the traditional "kill as many cancer cells as possible" approach to a more nuanced strategy of controlling tumor evolution.
IPM-Inspired Therapeutic Protocols
Adaptive Therapy Dosing Protocol
Theoretical Basis: Adaptive therapy applies ecological principles by maintaining a stable population of therapy-sensitive cells that can suppress the growth of resistant subpopulations through competition for resources and space [1]. This approach leverages the fitness cost of resistance by cycling drug pressure to maintain sensitivity within the tumor ecosystem.
Experimental Methodology:
- Baseline Assessment: Obtain tumor biopsy for single-cell RNA sequencing to characterize subclone heterogeneity and identify dominant signaling pathways [22].
- Initial Dose Determination: Begin treatment at 50% of MTD rather than maximum dose to preserve sensitive populations.
- Monitoring Schedule: Assess tumor burden monthly using circulating tumor DNA (ctDNA) and imaging; track subclone dynamics via serial liquid biopsies.
- Dose Adjustment Algorithm:
- If tumor burden decreases >20%: reduce dose by 25% or implement treatment holiday
- If tumor burden stable (±20%): maintain current dose
- If tumor burden increases >20%: increase dose by 25% or switch to alternative agent
- Resistance Monitoring: Perform monthly analysis of ABC transporter expression and resistance mutation tracking via digital PCR.
Implementation Data: Preliminary clinical data from prostate cancer trials demonstrate that adaptive therapy can maintain stable disease for extended periods with significantly reduced cumulative drug exposure compared to continuous MTD regimens.
Table 2: Adaptive Therapy Monitoring Parameters and Technologies
| Parameter | Assessment Method | Frequency | Decision Threshold |
|---|---|---|---|
| Tumor burden | CT/MRI imaging | 8-12 weeks | ±20% from baseline |
| Subclone dynamics | ctDNA sequencing | 4 weeks | Resistant clone >5% |
| ABC transporter expression | RNA-seq from liquid biopsy | 8 weeks | >2-fold increase |
| Resistance mutations | Digital PCR panel | 4 weeks | Variant allele frequency >1% |
| Patient symptoms | Quality of life questionnaires | 4 weeks | Significant deterioration |
Combination Therapy with Ecological Synergy
Theoretical Basis: Ecological systems respond to single perturbations through compensatory mechanisms, but combined strategic interventions can create stable new equilibria. Similarly, cancer ecosystems can be directed toward more treatable states through carefully timed combination therapies that target both cancer cells and their microenvironmental support systems [20] [19].
Experimental Methodology:
- Ecosystem Mapping: Characterize the tumor ecosystem using spatial transcriptomics and multiplex immunohistochemistry to map cancer cell subtypes, immune populations, stromal components, and vascular networks.
- Target Selection: Identify complementary targets including:
- Proliferation pathways in dominant sensitive clones
- Resistance mechanisms in minor resistant subclones
- Microenvironmental support cells (cancer-associated fibroblasts, tumor-associated macrophages)
- Angiogenic and immunomodulatory factors
- Dosing Sequence Optimization: Implement rational scheduling:
- Week 1-2: Microenvironment disruption (e.g., angiogenesis normalization)
- Week 3-6: Primary cytotoxic or targeted therapy
- Week 7-8: Treatment holiday to allow competitive suppression
- Repeat cycle with monitoring
Implementation Considerations: This approach requires sophisticated diagnostics and frequent monitoring but has the potential to transform advanced cancers into chronic, manageable conditions rather than rapidly lethal diseases.
Experimental Models and Assessment Tools
Preclinical Evolutionary Modeling Systems
3D Ecosystem Co-culture Model: This system models competitive interactions between sensitive and resistant subclones in a microenvironment context.
Protocol Details:
- Cell Line Engineering: Label drug-sensitive and drug-resistant cancer cell lines with different fluorescent markers (eGFP vs mCherry).
- Matrix Preparation: Create 3D extracellular matrix environments with varying stiffness and composition to mimic tissue-specific microenvironments.
- Co-culture Establishment: Plate cells in defined ratios (typically 90:10 sensitive:resistant) in the 3D matrix system.
- Treatment Application: Apply therapeutic agents in continuous, intermittent, or adaptive schedules.
- Population Tracking: Monitor population dynamics via fluorescence imaging and flow cytometry over 4-8 weeks.
- Microenvironment Analysis: Assess cytokine profiles, metabolic gradients, and cell-cell interaction changes.
Data Interpretation: This model allows quantification of competitive indices, fitness costs of resistance, and ecosystem-level responses to different treatment strategies before clinical implementation.
Longitudinal Molecular Monitoring Workflow
Liquid Biopsy Ecosystem Analysis: This protocol enables non-invasive tracking of tumor evolution during therapy.
Methodology:
- Sample Collection: Collect blood samples at baseline and every 2-4 weeks during therapy.
- Plasma Separation: Process within 2 hours of collection to prevent nucleic acid degradation.
- ctDNA Isolation: Extract cell-free DNA using silica-membrane technology.
- Library Preparation: Create sequencing libraries with unique molecular identifiers to reduce errors.
- Targeted Sequencing: Use hybrid capture panels covering 500+ cancer-associated genes.
- Clone Deconvolution: Apply computational methods to reconstruct subclonal architecture from variant allele frequencies.
- Phenotype Inference: Use RNA expression signatures from circulating tumor cells to infer pathway activation.
Analytical Outputs: This workflow generates temporal data on subclone dynamics, emerging resistance mechanisms, and ecosystem evolution in response to therapeutic pressure.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Tools for Eco-Evolutionary Cancer Therapy Studies
| Reagent/Category | Specific Examples | Research Application | Key Function |
|---|---|---|---|
| Fluorescent Cell Labels | eGFP, mCherry, CellTracker dyes | Competitive co-culture assays | Visual tracking of sensitive vs resistant populations |
| 3D Culture Matrices | Matrigel, collagen hydrogels, synthetic scaffolds | Tumor ecosystem modeling | Recreation of tumor microenvironment complexity |
| Single-Cell Analysis Platforms | 10X Genomics, Fluidigm C1 | Tumor heterogeneity characterization | Resolution of subclonal architecture and phenotypes |
| ctDNA Isolation Kits | QIAamp Circulating Nucleic Acid Kit, MagMAX Cell-Free DNA | Liquid biopsy processing | Non-invasive tumor monitoring and clone tracking |
| Targeted Sequencing Panels | Illumina TruSight Oncology, ArcherDx | Resistance mutation detection | Comprehensive profiling of evolving resistance mechanisms |
| Pathway Inhibitors | Tyrosine kinase inhibitors, epigenetic modulators | Combination therapy testing | Targeting of phenotype-specific vulnerabilities |
Discussion and Future Directions
The application of Integrated Pest Management principles to cancer therapy represents a paradigm shift from eradication to evolutionary control. This approach acknowledges that cancer is not a static enemy to be defeated but a dynamic, evolving ecosystem that must be managed through sophisticated understanding of ecological and evolutionary principles [20] [1] [21]. The protocols outlined here provide a framework for implementing this ecological perspective in both preclinical models and clinical practice.
Future developments in this field will likely focus on several key areas: improved evolutionary monitoring technologies, sophisticated mathematical modeling of cancer ecosystem dynamics, rational combination therapy design, and personalized adaptive therapy algorithms. As noted by researchers, "If the acquisition of drug resistance that leads to treatment failure and to patient death can be substantially delayed, then cancer could become a chronic condition" [19]. This vision of transforming lethal cancers into manageable chronic diseases represents the ultimate promise of applying ecological principles to oncology.
The eco-evolutionary approach to cancer therapy requires interdisciplinary collaboration between oncologists, ecologists, evolutionary biologists, and computational scientists. By learning from centuries of ecological management experience and applying these principles to cancer ecosystems, we can develop more sustainable and effective strategies for managing advanced cancers, ultimately turning one of humanity's most formidable foes into a controllable chronic condition.
Computational Strategies and Therapeutic Applications: From Models to Clinical Protocols
The persistence and evolution of therapeutic resistance remain the primary causes of treatment failure in oncology. Confronting this challenge requires a paradigm shift from traditional maximum cell-kill approaches to strategies that explicitly account for cancer's evolutionary dynamics [23]. Quantitative modeling provides the essential theoretical framework to understand, predict, and disrupt the evolutionary trajectories of resistant cancer cell populations. By formalizing the complex ecological interactions within tumors, these models enable the design of evolutionarily-informed treatment protocols that can delay or prevent the emergence of resistance [24] [23].
This article details the four dominant quantitative frameworks—Ordinary Differential Equations (ODEs), Partial Differential Equations (PDEs), Agent-Based Models (ABMs), and Game-Theoretic Frameworks—applied to cancer therapy resistance research. We present structured comparisons, experimental protocols, and implementation workflows to equip researchers with practical methodologies for developing and applying these models in preclinical and clinical settings.
Model Frameworks and Comparative Analysis
Ordinary Differential Equation (ODE) Models
ODE models describe the dynamics of cell populations over time using equations that depend only on time as an independent variable. They are particularly effective for modeling the competition between drug-sensitive and drug-resistant cell subpopulations at the whole-tumor level, ignoring spatial heterogeneity.
Core Application: Modeling population dynamics of sensitive and resistant cells under therapeutic pressure. Key Components:
- State variables (e.g., population sizes of sensitive cells ( S(t) ) and resistant cells ( R(t) ))
- Parameters (e.g., growth rates, conversion rates, drug kill rates)
- System of differential equations
A foundational ODE model for induced drug resistance is given by [25]: [ \begin{aligned} \frac{dx1}{dt} &= (1 - (x1 + x2))x1 - (\epsilon + \alpha u(t))x1 - du(t)x1 \ \frac{dx2}{dt} &= pr(1 - (x1 + x2))x2 + (\epsilon + \alpha u(t))x1 \end{aligned} ] where ( x1 ) and ( x2 ) represent sensitive and resistant cell populations, ( \epsilon ) is the spontaneous resistance rate, ( \alpha ) is the drug-induced resistance rate, ( d ) is drug cytotoxicity, ( p_r ) is the relative growth rate of resistant cells, and ( u(t) ) is the time-dependent drug concentration.
Partial Differential Equation (PDE) Models
PDE models extend population dynamics to include spatial dimensions, enabling the study of how spatial heterogeneity and tissue architecture influence the emergence and spread of resistance.
Core Application: Modeling spatiotemporal dynamics of tumor invasion and treatment response. Key Components:
- State variables dependent on both time and space (e.g., ( c(x,t) ))
- Diffusion terms modeling cell migration
- Reaction terms modeling proliferation and death
- Boundary conditions
A proliferation-invasion PDE model takes the form [26] [27]: [ \frac{\partial c(x,t)}{\partial t} = D\nabla^2c(x,t) + \rho c(x,t)(1 - \frac{c(x,t)}{K}) - kd(x,t)c(x,t) ] where ( c(x,t) ) is the cancer cell density at location ( x ) and time ( t ), ( D ) is the diffusion coefficient modeling cell motility, ( \rho ) is the proliferation rate, ( K ) is the carrying capacity, and ( kd(x,t) ) is the therapy-induced death rate.
Agent-Based Models (ABMs)
ABMs simulate the behavior and interactions of individual cells (agents) within a defined environment, generating emergent population-level dynamics from simple individual-level rules.
Core Application: Modeling intratumor heterogeneity and complex cellular interactions driving resistance. Key Components:
- Agents representing individual cells
- Rule sets governing agent behavior
- Environment representing tissue space and resources
- Stochastic elements
ABMs are particularly valuable when analytic solutions are intractable, such as in models with complex interactions and finite population sizes [28]. They can incorporate rules for cell division, death, mutation, movement, and resource consumption based on local microenvironmental conditions.
Evolutionary Game-Theoretic Frameworks
Evolutionary game theory models cancer as an ecosystem where different cell types (strategies) compete according to fitness payoffs, with treatment acting as a modifier of the evolutionary landscape.
Core Application: Designing adaptive therapy protocols that control tumor evolution. Key Components:
- Player types (sensitive cells, resistant cells, immune cells)
- Strategy sets (cooperate/defect phenotypes)
- Payoff matrices representing fitness interactions
- Population dynamics governed by evolutionary stability
In this framework, cancer cells act as "defectors" in a population dynamics game, while healthy cells act as "cooperators," with the immune system serving as a dynamic regulator [29]. Treatment becomes an evolutionary "game" where the objective shifts from maximum cell kill to controlling the competitive balance between sensitive and resistant populations.
Table 1: Comparative Analysis of Quantitative Modeling Approaches
| Model Type | Mathematical Formulation | Spatial Resolution | Key Strengths | Primary Applications in Resistance Research |
|---|---|---|---|---|
| ODE Models | System of differential equations: ( \frac{d\vec{x}}{dt} = f(\vec{x}, t, \vec{p}) ) | No | Mathematical tractability, parameter identifiability, well-suited for optimal control | Modeling population dynamics of sensitive/resistant cells; predicting resistance evolution under different dosing schedules [25] [26] |
| PDE Models | Partial differential equations: ( \frac{\partial c}{\partial t} = D\nabla^2c + R(c) ) | Yes | Captures spatial heterogeneity, invasion fronts, and microenvironmental gradients | Studying geography of resistance emergence; impact of tumor architecture on treatment efficacy [26] [27] |
| Agent-Based Models | Rule-based systems with stochastic elements | Yes (discrete) | Models individual cell variability and complex local interactions; emergent phenomena | Investigating intratumor heterogeneity; role of rare cell subpopulations in resistance [28] [2] |
| Game-Theoretic Frameworks | Payoff matrices + population dynamics: ( \frac{dxi}{dt} = xi[(A\vec{x})_i - \vec{x}^TA\vec{x}] ) | Optional | Explains paradoxical behaviors; designs evolutionarily stable treatments | Adaptive therapy design; exploiting cost of resistance; maintaining treatment-sensitive populations [29] [23] |
Table 2: Dominant Resistance Mechanisms and Corresponding Modeling Approaches
| Resistance Mechanism | Most Suitable Model Types | Key Model Parameters | Expected Dynamics |
|---|---|---|---|
| Pre-existing genetic mutations | ODE, Game Theory | Mutation rate (ε), relative fitness of resistant cells (pr) | Initial decline then relapse due to resistant population expansion [25] |
| Drug-induced resistance | ODE, ABM | Induction rate (α), selection pressure | Accelerated resistance development with continuous therapy [25] |
| Spatial heterogeneity in drug penetration | PDE, ABM | Diffusion coefficient (D), nutrient/oxygen gradients | Resistance emergence in sanctuary sites with subtherapeutic drug levels [26] |
| Metabolic cooperation and competition | Game Theory, ABM | Resource availability, cost of resistance | Stable coexistence of sensitive/resistant cells under resource limitation [29] [23] |
| Epigenetic plasticity | ABM, ODE with phenotype switching | Switching rates between phenotypes | Rapid adaptive resistance without genetic changes [25] |
Experimental Protocols and Workflows
Protocol 1: ODE Model Development and Calibration for Resistance Forecasting
Objective: Develop a predictive ODE model for resistance evolution under specific therapeutic regimens.
Materials and Reagents:
- In vitro or in vivo time-course data on tumor volume/cell count
- Drug concentration-response data
- Genomic or functional data on resistance marker prevalence
Procedure:
- System Specification: Define state variables (e.g., sensitive cells S, resistant cells R) and their interactions
- Parameter Estimation: Use maximum likelihood or Bayesian methods to estimate parameters from pretreatment data
- Model Validation: Compare model predictions with observed treatment response data not used in calibration
- Therapy Optimization: Apply optimal control theory to identify dosing schedules that maximize time to progression [25]
Data Analysis:
- Structural identifiability analysis to determine which parameters can be uniquely estimated
- Sensitivity analysis to identify most influential parameters
- Bayesian calibration to quantify parameter uncertainty and model predictions
Protocol 2: Implementing Adaptive Therapy Based on Evolutionary Games
Objective: Design and execute an evolution-based adaptive therapy protocol in preclinical models.
Materials and Reagents:
- Syngeneic or patient-derived xenograft models
- Biomarkers for tumor burden (e.g., PSA, imaging)
- Drugs with known resistance mechanisms
Procedure:
- Model Initialization: Calibrate game-theoretic model with baseline tumor composition data
- Treatment Strategy: Implement adaptive algorithm:
- Administer therapy until tumor burden decreases by predetermined percentage (e.g., 50%)
- pause treatment until tumor regrows to initial size
- Resume treatment [2]
- Monitoring: Track tumor burden and resistant subpopulation frequently
- Model Refinement: Update model parameters based on observed response
Validation Metrics:
- Time to progression compared to standard continuous therapy
- Cumulative drug dose
- Resistant subpopulation fraction at progression
Figure 1: Adaptive Therapy Decision Workflow
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Resources for Evolutionary Therapy Modeling
| Resource Category | Specific Examples | Function in Resistance Research | Compatible Model Types |
|---|---|---|---|
| Preclinical Models | Patient-derived xenografts (PDX), Genetically engineered mouse models (GEMMs) | Provide in vivo systems for validating model predictions and testing therapeutic strategies | All model types |
| Cell Line Repositories | Cancer Cell Line Encyclopedia (CCLE), NCI-60 panel | Enable high-throughput drug screening and resistance mechanism identification | ODE, Game Theory |
| Omic Technologies | Whole-exome sequencing, RNA-seq, Single-cell sequencing | Characterize molecular evolution of resistance and tumor heterogeneity | ABM, PDE, ODE |
| Mathematical Software | MATLAB, R, Python (SciPy), COPASI | Implement and numerically solve mathematical models | All model types |
| Clinical Data Resources | TCGA, GENIE, Adaptive therapy trial data | Provide real-world data for model calibration and validation | All model types |
Integration and Visualization of Model Dynamics
Figure 2: Multi-Model Integration Workflow for Clinical Translation
The integration of ODE, PDE, agent-based, and game-theoretic modeling approaches provides a powerful multidisciplinary framework to address the critical challenge of therapy resistance in oncology. Each approach offers complementary insights: ODEs for population-level dynamics, PDEs for spatial heterogeneity, ABMs for cellular complexity, and game theory for evolutionary strategies. The future of cancer therapy resistance research lies in combining these quantitative approaches with experimental and clinical data to design evolutionarily-informed treatment strategies that can outmaneuver cancer's adaptive capabilities. As these models become increasingly refined and validated, they hold the promise of transforming cancer from a lethal disease to a controllable chronic condition.
Adaptive Therapy (AT) is an evolution-based approach to cancer treatment that updates treatment decisions in dynamic response to evolving tumor dynamics. This strategy represents a fundamental shift from the traditional maximum tolerated dose (MTD) paradigm. Unlike MTD, which aims to kill the maximum number of tumor cells and often accelerates the proliferation of resistant populations, adaptive therapy maintains tolerably high levels of tumor burden to exploit the competitive suppression of treatment-resistant subpopulations by treatment-sensitive subpopulations [1] [30].
The conceptual foundation of adaptive therapy rests on core evolutionary principles. While the emergence of resistant cancer cells to current therapies is virtually inevitable, the proliferation of these resistant phenotypes is not inevitable and can be delayed or prevented with sufficient understanding of underlying eco-evolutionary dynamics [1]. Adaptive therapy capitalizes on the Darwinian interactions between sensitive and resistant cell populations, leveraging the fitness cost of resistance mechanisms that often impair cellular proliferation in treatment-free environments [30].
Theoretical Framework and Evolutionary Principles
Evolutionary Dynamics of Cancer Therapy
Cancer ecosystems demonstrate remarkable robustness to therapeutic perturbations due to cellular diversity, spatial heterogeneity in genotypic and phenotypic properties, and variations in the tumor microenvironment [1]. Traditional MTD approaches accelerate competitive release—an evolutionary phenomenon where eliminating sensitive cell populations removes natural competitors for resistant cells, allowing their rapid expansion [1]. This explains why MTD often produces initial tumor shrinkage followed by aggressive, treatment-resistant relapse.
Adaptive therapy applies principles derived from successful pest management strategies, where controlled application of pesticides prevents emergence of resistance while maintaining acceptable damage levels [1]. Similarly, AT maintains a stable tumor volume by strategically balancing treatment-sensitive and-resistant populations through dynamic treatment modulation.
Key Requirements for Adaptive Therapy Success
Research indicates that adaptive therapy success depends on three critical characteristics of the cancer ecosystem [30]:
- Cost of Resistance: Resistance mechanisms must impose a fitness cost that reduces proliferative advantage in untreated environments
- Competitive Suppression: Resistant cells must be suppressible through competition with sensitive cells
- Therapy Sensitivity: Treatment must effectively reduce the population of sensitive cells
When these conditions are met, mathematical models demonstrate a trade-off curve between time for resistant cells to emerge and mean cancer burden, which guides protocol optimization [30].
Table 1: Comparison of Cancer Treatment Paradigms
| Parameter | MTD | Intermittent Therapy | Adaptive Therapy |
|---|---|---|---|
| Treatment Goal | Maximum cell kill | Periodic high-dose killing | Stable tumor burden |
| Dosing Schedule | Continuous high dose | Fixed periodic holidays | Dynamic, response-driven |
| Selection Pressure | High for resistance | Intermediate | Low for resistance |
| Competitive Release | Maximized | Moderate | Minimized |
| Cumulative Dose | High | Moderate | Variable, often lower |
Protocol Classifications and Algorithmic Structures
Dose-Skipping Protocols
Dose-skipping approaches administer high-dose treatment until a specific tumor response threshold is achieved, followed by a treatment holiday until a predetermined upper threshold is reached [30]. The first adaptive therapy clinical trial for metastatic castrate-resistant prostate cancer (mCRPC) employed a dose-skipping protocol where abiraterone was withdrawn until prostate-specific antigen (PSA) returned to 50% of baseline levels, then restarted [30]. This 50% rule created patient-specific treatment holidays that varied considerably between individuals, with holidays typically shortening in later treatment cycles as PSA dynamics accelerated.
Dose-Modulation Protocols
Dose-modulation approaches adjust drug dosage at regular intervals based on tumor response metrics rather than implementing complete treatment holidays [30]. While both dose skipping and dose modulation have demonstrated efficacy in experimental models, only dose skipping has been translated to clinical practice thus far [30]. Dose modulation offers potential advantages in maintaining more stable tumor control through finer adjustments to therapeutic pressure.
Quantitative Framework and Mathematical Modeling
Mathematical Foundations
Adaptive therapy protocols are fundamentally guided by mathematical models that simulate tumor dynamics under treatment pressure. The core modeling approach typically incorporates distinct sensitive and resistant cancer cell populations, with extensions including healthy cells, immune cells, resource dynamics (e.g., hormones), Allee effects, and phenotypic plasticity [30]. Simple models often demonstrate robustness across most extensions except for Allee effects and cell plasticity, which require specialized modeling approaches [30].
Table 2: Key Mathematical Models in Adaptive Therapy
| Model Type | Key Components | Clinical Applications | References |
|---|---|---|---|
| Lotka-Volterra Competition | Sensitive-resistant cell competition | Prostate cancer, melanoma | [30] |
| Gompertzian Growth | Carrying capacity, growth decay | Theoretical optimization | [30] |
| Consumer-Resource | Androgen dynamics in prostate cancer | mCRPC with abiraterone | [30] |
| Hybrid Cellular Automaton | Spatial competition, cost of resistance | CDK inhibitor applications | [30] |
Optimal Treatment Timing Framework
Recent research has established a general framework for deriving optimal treatment protocols that account for discrete clinical monitoring intervals [31]. This approach addresses the significant limitation of previous models that ignored practical constraints of clinical appointments where tumor burden is measured and treatment schedules reevaluated. The framework identifies a critical trade-off between monitoring frequency and time to progression, proposing that a subset of patients with qualitatively different dynamics require novel protocols with thresholds that change over the treatment course [31].
The mathematical optimization reveals that tumor dynamics between patients vary significantly, resulting in substantial heterogeneity in outcomes that necessitates personalization of adaptive protocols [31]. This personalized approach moves beyond the one-size-fits-all application of the same threshold rules to all patients.
Clinical Workflow and Experimental Protocol
Clinical Implementation Workflow
Detailed Experimental Protocol for mCRPC
Background: This protocol adapts the approach from the first adaptive therapy clinical trial in metastatic castrate-resistant prostate cancer, which demonstrated prolonged progression-free survival and lower cumulative drug dose compared to standard of care [30].
Inclusion Criteria:
- Histologically confirmed metastatic castrate-resistant prostate cancer
- Minimum 50% drop in PSA level under abiraterone administration
- Adequate organ function and performance status
- Willingness to comply with frequent monitoring schedule
Materials and Reagents:
- Abiraterone acetate (Zytiga)
- Prostate-specific antigen (PSA) assay kits
- Imaging equipment (CT, MRI, or bone scan)
- Data collection forms for symptom tracking
Procedure:
- Baseline Assessment: Obtain baseline PSA level, perform staging imaging, document disease-related symptoms
- Initial Treatment Phase: Administer abiraterone at standard dose (1000mg daily) with prednisone
- Monitoring Schedule: Measure PSA levels at 2-week intervals initially, extend to 4-week intervals once stability established
- Treatment Decision Points:
- Continue abiraterone until PSA declines to 50% of baseline value (treatment response)
- Withdraw abiraterone until PSA returns to baseline level (treatment holiday)
- Reinitiate abiraterone at previous dose level
- Response Evaluation:
- Record PSA doubling time during treatment holidays
- Monitor for symptomatic progression
- Perform imaging every 12 weeks or as clinically indicated
- Protocol Adaptation:
- Shorten treatment holidays if PSA acceleration observed in subsequent cycles
- Consider dose modification for toxicity management
- Document cumulative drug exposure
Quality Control:
- Standardize PSA measurement techniques across all assessments
- Establish threshold for significant PSA progression (typically 50% above nadir)
- Implement centralized review of imaging studies
Research Reagent Solutions and Technical Tools
Table 3: Essential Research Tools for Adaptive Therapy Investigations
| Research Tool | Function | Example Applications |
|---|---|---|
| Mathematical Modeling Software | Simulate tumor dynamics under treatment | Protocol optimization, patient-specific forecasting |
| PSA Assay Kits | Quantify prostate-specific antigen | Monitoring tumor burden in prostate cancer trials |
| Circulating Tumor DNA (ctDNA) Analysis | Detect resistance mutations | Early identification of resistant subclones |
| Patient-Derived Xenograft (PDX) Models | In vivo testing of adaptive protocols | Preclinical validation of dosing strategies |
| Lotka-Volterra Competition Models | Quantify competitive interactions | Predicting sensitive-resistant cell dynamics |
| Hormone Level Assays | Measure resource dynamics | Androgen monitoring in prostate cancer |
Clinical Translation and Trial Design Considerations
Adaptive therapy has been integrated into several ongoing or planned clinical trials, including treatments for metastatic castrate-resistant prostate cancer, ovarian cancer, and BRAF-mutant melanoma [31] [30]. The initial clinical results from the mCRPC trial demonstrated significant extensions in time to progression over standard of care, generating interest in designing new adaptive treatment protocols across multiple cancer types [30].
Critical considerations for clinical translation include:
- Biomarker Selection: Identifying reliable, responsive biomarkers of tumor burden (e.g., PSA in prostate cancer) that can guide treatment decisions
- Monitoring Frequency: Balancing practical constraints with optimal assessment intervals to detect significant changes before progression
- Threshold Determination: Establishing patient-specific versus population-based thresholds for treatment adaptation
- Trial Design: Implementing novel clinical trial structures like Sequential Multiple Assignment Randomized (SMAR) trials that can efficiently compare adaptive strategies [32]
The planned ANZadapt trial (NCT05393791) in metastatic castrate-resistant prostate cancer represents a larger, randomized study that will provide more robust evidence regarding adaptive therapy efficacy [30].
Adaptive therapy protocols represent a paradigm shift in cancer treatment that explicitly incorporates evolutionary principles to control tumor proliferation and delay therapeutic resistance. Both dose-skipping and dose-modulation approaches offer dynamic, patient-specific strategies that maintain therapeutic efficacy while reducing cumulative drug exposure and potentially extending progression-free survival.
Future research directions should address several open questions identified by the Cancer Adaptive Therapy Models workshop [30], including optimal model complexity for clinical utility, incorporating immune cell interactions, understanding spatial heterogeneity effects, and developing efficient model parameterization from limited clinical data. Additionally, expanding adaptive therapy beyond hormonal agents to targeted therapies, chemotherapeutics, and immunotherapy combinations presents both challenges and opportunities for broadening clinical impact.
As mathematical models become increasingly integrated into clinical oncology practice [33], adaptive therapy protocols offer a promising framework for personalizing cancer management based on individual tumor dynamics and evolutionary trajectories.
Evolutionary steering represents a paradigm shift in cancer therapy, moving from maximum cell kill to the strategic control of tumor evolution. This approach leverages Darwinian dynamics to direct the evolutionary trajectory of cancer cell populations into states of vulnerability [34] [35]. The foundational principle recognizes that tumors are dynamically evolving ecosystems where intervention with a therapeutic agent fundamentally alters the fitness landscape, selectively favoring subpopulations with specific resistance mechanisms [34]. The goal of evolutionary steering is not merely to reduce tumor burden temporarily but to constrain future evolutionary paths to avoid treatment-resistant outcomes and prolong disease control.
Collateral sensitivity, a pivotal phenomenon in evolutionary steering, occurs when genetic or epigenetic alterations conferring resistance to one drug simultaneously increase susceptibility to a second, unrelated agent [34] [35]. This creates an "evolutionary double bind" where the adaptation that ensures survival against the first therapeutic threat becomes a liability when encountering the second [35]. This trade-off emerges from fundamental constraints in evolutionary optimization, where excellence in one environment often compromises performance in another. The strategic exploitation of collateral sensitivity requires deep understanding of the fitness landscapes shaped by different therapeutics and the predictable evolutionary trajectories they enforce [34].
Theoretical Framework and Evolutionary Principles
Fitness Landscapes and Evolutionary Trapping
The conceptual framework for evolutionary steering relies on modeling genotype-phenotype relationships within fitness landscapes [34]. In these multidimensional representations, a cell's position corresponds to its genetic and epigenetic state, while elevation reflects relative fitness in a given environment. Drug application dramatically reshapes this landscape, transforming previously neutral or slightly deleterious genotypes into fitness peaks [34]. Cancer cell populations climb these peaks through Darwinian selection, leading to evolutionary adaptation and therapeutic resistance.
Evolutionary steering exploits the fact that different drugs create divergent fitness landscapes [34]. A strategic drug sequence can direct populations toward evolutionary traps—regions of the combined fitness landscape where high fitness for one drug corresponds to exceptionally low fitness for another. This approach contrasts with conventional combination therapy by emphasizing temporal sequencing over simultaneous administration, though both strategies may be integrated [35].
Table 1: Key Evolutionary Concepts in Cancer Therapy
| Concept | Definition | Therapeutic Implication |
|---|---|---|
| Evolutionary Steering | Directing tumor evolution through strategic therapeutic intervention | Control of evolutionary trajectories rather than immediate maximal cell kill |
| Collateral Sensitivity | Resistance to one drug confers hypersensitivity to another | Creates opportunities for sequential therapeutic targeting |
| Evolutionary Double Bind | Adaptive solution to one challenge creates vulnerability to another | Limits evolutionary escape routes |
| Fitness Landscape | Mapping of genotype to reproductive success in specific environment | Predicts evolutionary trajectories under different selective pressures |
| Evolutionary Trap | Therapeutic sequence leading to population extinction or control | Goal of evolutionary steering strategies |
The Double-Bind Strategy in Practice
The evolutionary double bind operationalizes collateral sensitivity through structured treatment sequences [35]. The initial therapeutic agent (Drug A) selects for resistant subclones possessing specific molecular alterations. These alterations, while conferring resistance to Drug A, simultaneously create dependencies or disrupt homeostatic mechanisms that render cells exceptionally vulnerable to a follow-up agent (Drug B). The population, now dominated by Drug A-resistant clones, collapses when exposed to Drug B, potentially driving it below sustainable thresholds or to extinction [34] [35].
This strategy acknowledges that complete eradication of all cancer cells is often biologically implausible, and instead aims to constrain tumor evolution within manageable bounds. Successful implementation requires understanding the molecular mechanisms underlying both resistance and the resulting vulnerabilities, enabling rational design of therapeutic sequences rather than empirical testing [34].
Experimental Models and Methodologies
Recapitulating Tumor Evolution In Vitro
Conventional drug resistance models suffer from critical limitations, including small population sizes that fail to capture intratumoral heterogeneity and serial passaging that introduces artificial bottlenecks [34]. These approaches typically wait for de novo resistance mutations, resulting in highly variable, stochastic evolutionary dynamics poorly representative of clinical scenarios where pre-existing resistant subclones are selected [34].
Advanced models employ large population systems (10^8–10^9 cells) grown without replating to maintain complex clonal architectures and pre-existing resistant subpopulations [34]. The HYPERflask system, with a capacity of 150-200 million cells—approximately tenfold greater than standard T175 flasks—enables maintenance of substantial heterogeneity while exposing populations to high drug concentrations without extinction [34]. This approach more faithfully recapitulates the evolutionary dynamics observed in human malignancies.
Single-cell barcoding technologies provide critical tools for tracking clonal dynamics [34]. By labeling individual cells with unique genetic barcodes prior to expansion and treatment, researchers can determine whether resistant clones emerged from pre-existing populations (same barcodes enriched across replicates) or through de novo mutation (unique barcodes in each replicate) [34]. This lineage tracing enables quantitative analysis of evolutionary trajectories and clone-specific responses to therapeutic interventions.
Experimental Workflow for Evolutionary Steering Studies
Protocol: Establishing Large Population Evolutionary Models
Materials:
- HCC827 non-small cell lung cancer cells (EGFR exon19 del mutant)
- High-complexity lentiviral barcoding library (≥1 million unique barcodes)
- HYPERflask cell culture vessels or equivalent large-scale culture system
- Targeted therapeutic agents (e.g., gefitinib, trametinib)
- Next-generation sequencing platform for barcode quantification
- Computational resources for population dynamics modeling
Procedure:
- Library Barcoding: Transduce one million HCC827 cells at low multiplicity of infection (MOI<0.3) to ensure single barcode integration per cell.
- Population Expansion: Expand barcoded cells to approximately 120 million cells in HYPERflask systems to establish the pre-treatment population (POT).
- Replicate Seeding: Seed multiple HYPERflasks with 15 million cells each from the same POT to establish biological replicates with shared clonal composition.
- Therapeutic Exposure: Culture to 80-90% confluence then expose to therapeutic agents at clinically relevant concentrations. Include DMSO vehicle controls.
- Longitudinal Sampling: Collect cell samples at regular intervals (e.g., days 0, 3, 7, 14, 21) for barcode sequencing while maintaining cultures without disruptive passaging.
- Barcode Quantification: Extract genomic DNA and amplify barcode regions for sequencing. Map sequences to reference barcode library to determine clonal frequencies.
- Dynamic Modeling: Apply mathematical models to quantify evolutionary rates, selection coefficients, and clonal trajectory correlations across replicates.
Validation Metrics:
- Pre-existing resistant clones identified by significantly enriched barcodes (p<0.01, Fisher's exact test) across independent replicates
- Reproducible evolutionary trajectories demonstrated by high correlation (r>0.8) of clonal frequency dynamics between replicates
- Minimum population size of 10^8 cells maintained throughout experiment to preserve heterogeneity
Quantitative Assessment of Collateral Sensitivity
Data Analysis and Interpretation
The systematic quantification of collateral sensitivity requires integration of drug response data with clonal tracking information [34]. Resistance is quantified by calculating fold-change in IC50 values relative to parental controls, while collateral sensitivity is identified by significant decreases in IC50 for secondary agents [36]. The strength of collateral sensitivity interactions can be ranked by sensitivity indices, with values <-2.0 typically considered strong effects warranting therapeutic exploitation [36].
Table 2: Quantitative Framework for Collateral Sensitivity Assessment
| Parameter | Calculation | Interpretation |
|---|---|---|
| Resistance Factor (RF) | IC50(resistant)/IC50(parental) | RF > 5 indicates significant resistance |
| Sensitivity Index (SI) | IC50(parental)/IC50(resistant) - 1 | SI < -0.5 indicates collateral sensitivity |
| Clonal Dominance | Maximum barcode frequency in population | Values >0.3 suggest monoclonal resistance |
| Selection Coefficient | Rate of barcode frequency change per generation | Higher absolute values indicate stronger selection |
| Trajectory Consistency | Correlation of barcode dynamics across replicates | R > 0.7 indicates deterministic evolution |
Molecular validation of collateral sensitivity mechanisms requires integrated genomic and transcriptomic profiling [34] [37]. In glioblastoma models, correlation analysis between mRNA expression of DNA damage response regulators and inherent therapy resistance identified ATR overexpression as a key mediator of radioresistance and potential vulnerability [37]. Similarly, in lung cancer models, genomic profiling of clones demonstrating collateral sensitivity revealed specific resistance mechanisms that created new therapeutic dependencies [34].
Protocol: Evaluating Collateral Sensitivity Profiles
Materials:
- Isolated resistant sublines or enriched resistant clones from barcoding experiments
- Candidate secondary therapeutic agents with divergent mechanisms of action
- High-throughput screening system (96- or 384-well format)
- Cell viability assay (e.g., ATP-based luminescence, resazurin reduction)
- Automated liquid handling system for compound serial dilution
Procedure:
- Cell Plating: Seed resistant and parental cell lines at optimized densities (typically 1-5×10^3 cells/well) in 96-well plates.
- Compound Dilution: Prepare 10-point, 1:3 serial dilutions of secondary therapeutic agents using DMSO as vehicle control.
- Viability Assessment: After 72-96 hours incubation, measure cell viability using standardized ATP-based luminescence assays.
- Dose-Response Modeling: Fit sigmoidal dose-response curves to calculate IC50 values using four-parameter logistic models.
- Cross-Resistance Mapping: Compute resistance factors (RF) for all secondary agents relative to parental cell line sensitivity.
- Collateral Sensitivity Identification: Flag compounds with significant sensitivity indices (SI < -0.5) for further validation.
- Mechanistic Investigation: Subject hits to transcriptomic profiling and genomic analysis to identify vulnerability mechanisms.
Validation Criteria:
- Collateral sensitivity effects reproduced in at least two biologically independent resistant lines
- Minimum 2-fold increased sensitivity (SI ≤ -1.0) compared to parental controls
- Dose-dependent response with R^2 > 0.9 for curve fitting
- Effect maintained in 3D culture systems or patient-derived models where feasible
Computational Modeling and Prediction
Mathematical Framework for Evolutionary Steering
Computational approaches are indispensable for predicting evolutionary trajectories and optimizing steering strategies [38]. Mathematical models span multiple scales, from molecular dynamics simulations of drug-target interactions to ordinary differential equation models of cellular population dynamics [38]. Agent-based models can simulate individual cell behaviors and interactions within spatially structured environments, capturing emergent evolutionary dynamics not apparent from population-level observations [38].
Fitness landscape models provide particularly powerful frameworks for designing evolutionary steering strategies [34]. By mapping genotypic states to reproductive fitness under different selective conditions, these models can identify drug sequences that create evolutionary traps [34]. The core principle involves identifying drug pairs with antagonistic fitness landscapes, where high fitness peaks for one drug correspond to deep valleys for the other.
Evolutionary Steering Creates Therapeutic Vulnerability
Protocol: Computational Prediction of Steering Strategies
Materials:
- Longitudinal barcode sequencing data from evolutionary experiments
- Drug sensitivity profiles for primary and secondary agents
- Computational environment (R, Python, or MATLAB)
- Optimization algorithms for parameter estimation
- Stochastic simulation frameworks
Procedure:
- Parameter Estimation: Fit selection coefficients for individual barcodes under drug selection using maximum likelihood methods applied to frequency trajectories.
- Fitness Landscape Reconstruction: Infer multidimensional fitness landscapes by correlating genotypic features (mutations, expression signatures) with relative growth rates under different drug conditions.
- Stochastic Simulation: Implement stochastic population genetics models to project evolutionary trajectories under candidate therapeutic sequences.
- Steering Strategy Optimization: Identify drug sequences that maximize probability of driving population to evolutionary traps using optimal control theory or reinforcement learning approaches.
- Sensitivity Analysis: Quantify robustness of predictions to parameter uncertainty and model assumptions.
- Experimental Validation: Test top predicted steering strategies in vitro using the large population system.
Validation Metrics:
- Model accurately predicts (>80% concordance) dominant barcodes emerging under new drug sequences
- Successful experimental reproduction of predicted collateral sensitivity effects
- Significant extension of time to progression or population control in validation experiments
Research Reagent Solutions
Table 3: Essential Research Tools for Evolutionary Therapy Studies
| Reagent/Category | Specific Examples | Research Application |
|---|---|---|
| Large-Scale Culture Systems | HYPERflask, cell factories | Maintain large populations (10^8-10^9 cells) without passaging bottlenecks |
| Single-Cell Tracking | High-complexity lentiviral barcodes, CRISPR lineage tracing | Longitudinal monitoring of clonal dynamics and evolutionary trajectories |
| Targeted Therapeutics | Gefitinib (EGFR inhibitor), Trametinib (MEK inhibitor) | Selective pressures to steer evolution and probe collateral sensitivity |
| DDR Inhibitors | AZD-6738 (ATR inhibitor), KU-60019 (ATM inhibitor) | Target vulnerabilities in DNA damage response pathways [37] |
| Computational Tools | Population genetics simulations, fitness landscape modeling | Predict evolutionary trajectories and optimize steering strategies [38] |
| Viability Assays | ATP-based luminescence, resazurin reduction | High-throughput quantification of drug sensitivity and resistance |
Clinical Translation and Challenges
The translation of evolutionary steering from theoretical concept to clinical application faces several significant challenges [35]. Tumors exhibit high contingency in their evolutionary trajectories, with multiple possible resistance mechanisms emerging from similar starting conditions [36]. The speed of evolution varies substantially between cancer types and individual patients, necessitating adaptive monitoring strategies [35]. Current limitations in tracking tumor population states in patients through liquid biopsies or imaging further complicate real-time steering adjustments [35].
Promising clinical applications have emerged in specific contexts. In metastatic castrate-resistant prostate cancer, evolutionary model-informed treatment scheduling significantly prolonged responses to abiraterone compared to standard continuous dosing [35]. Similar approaches are being explored in breast cancer and melanoma models [35]. The integration of single-cell transcriptomics with evolutionary principles offers particular promise for deciphering complex resistance patterns and identifying novel collateral sensitivity relationships [9].
Despite these advances, substantial work remains to develop evolutionary steering into a broadly applicable therapeutic paradigm. Future directions must include improved non-invasive monitoring technologies, refined mathematical models incorporating spatial heterogeneity and immune interactions, and clinical trial designs that explicitly test evolutionary hypotheses [34] [35]. The systematic application of these principles holds potential to transform cancer from an acute therapeutic challenge to a chronically manageable disease through continuous evolutionary control.
Despite the continuous development of new anticancer agents, the evolution of therapy resistance remains the primary cause of treatment failure in metastatic cancers [10] [1]. Resistance is not merely a molecular phenomenon but an evolutionary process governed by Darwinian dynamics within tumor ecosystems [1]. Extinction therapy represents a novel treatment paradigm that explicitly incorporates evolutionary principles to eradicate cancerous populations. This approach draws inspiration from Anthropocene extinctions, where human activities cause the extinction of large, diverse, and geographically dispersed species [39]. Similarly, the eradication of metastatic cancer requires driving the malignant population to extinction by exploiting its eco-evolutionary vulnerabilities [39]. This protocol outlines the rationale, experimental models, and methodological framework for implementing extinction therapy through rational drug sequencing.
The conceptual foundation of extinction therapy rests on a two-strike strategy [39]. The first strike applies reductive therapy to diminish tumor population size and genetic diversity, while the second strike introduces novel perturbations that exploit the eco-evolutionary weaknesses of the decimated population [39]. This approach recognizes that while resistant cells are virtually inevitable in large, heterogeneous cancer populations, their proliferation is not predetermined and can be constrained through evolutionary steering [1]. The principles of extinction therapy stand in contrast to conventional maximum tolerated dose (MTD) strategies, which often accelerate competitive release of resistant clones by eliminating competing populations [1].
Theoretical Framework and Evolutionary Principles
Eco-Evolutionary Dynamics of Tumor Extinction
The eradication of metastatic cancer populations follows principles analogous to species extinctions in nature [39]. Both processes involve large, heterogeneous populations facing selective pressures that ultimately drive them below a minimum viable population (MVP) threshold. Beyond this threshold, stochastic demographic fluctuations and Allee effects (where individuals in small populations have reduced fitness) create an absorbing boundary toward extinction [39].
Key eco-evolutionary vulnerabilities exploited by extinction therapy include:
- Demographic stochasticity: Random fluctuations in birth and death rates disproportionately affect small populations
- Reduced genetic diversity: Population bottlenecks decrease adaptive potential
- Fragmented ecology: Isolated subpopulations cannot benefit from rescue effects
- Allee effects: Below a critical density, populations experience reduced fitness
Mathematical modeling of these dynamics employs both deterministic and stochastic frameworks [39]. A basic deterministic model describes tumor population dynamics as:
Where N(t) represents the number of cancer cells and g(t) the per capita growth rate [39]. As populations decline, stochastic individual-based models become essential for predicting extinction probabilities, incorporating demographic stochasticity, heterogeneity, and Allee effects [39].
Rational Drug Sequencing Versus Conventional Approaches
Extinction therapy fundamentally differs from conventional chemotherapy through its explicit incorporation of evolutionary dynamics:
Table: Comparison of Treatment Strategies
| Parameter | Conventional MTD Therapy | Extinction Therapy |
|---|---|---|
| Primary objective | Maximize tumor cell kill | Steer evolutionary trajectory |
| Treatment schedule | Continuous at maximum doses | Sequential, rotating drugs |
| Evolutionary impact | Selective sweep of resistant clones | Constrain resistance emergence |
| Therapeutic focus | Molecular resistance mechanisms | Eco-evolutionary population dynamics |
| Resistance management | Target specific mechanisms | Exploit collateral sensitivity |
Quantitative Evidence for Sequential Therapy
Antibiotic Sequential Therapy as a Model System
Research in bacterial systems provides compelling proof-of-concept for sequential therapy approaches. Surprisingly, fast sequential switching between only β-lactam antibiotics (a homogeneous set) resulted in increased extinction of Pseudomonas aeruginosa populations despite expectations that this would promote cross-resistance [40]. This effect was favored by low rates of spontaneous resistance emergence and low levels of spontaneous cross-resistance among the antibiotics in sequence [40].
In these experiments, bacterial populations were challenged with sequential treatments across different antibiotic sets using a serial dilution protocol with 2% culture transfer after 12 hours across 96 transfers (approximately 500 generations) [40]. Antibiotic concentrations were calibrated to IC75 (inhibitory concentration of 75%), allowing bacterial adaptation under selection pressure [40]. The triple β-lactam sequences (CAR-CEF-DOR and TIC-AZL-CEZ) showed unexpectedly high treatment potency, with extinct fractions of 27.2% and 13.3% respectively, comparable to heterogeneous drug sets (CAR-CIP-GEN, 15% extinct) [40].
Dynamics of Resistance Mutations in Cancer
Cancer therapy resistance follows evolutionary patterns observable at short timescales. During treatment of acute bacterial respiratory infections (as a model system), resistance mutations rapidly expand and contract in response to antibiotic changes, with some mutations increasing nearly 40-fold over 5-12 days following therapy alterations [41]. Conversely, mutations conferring resistance to non-administered antibiotics diminish and can go to extinction [41]. These findings demonstrate the responsiveness of resistance mutations to therapeutic changes and the potential for driving mutations to extinction through strategic drug cycling.
Experimental Models and Protocols
Lineage Tracing and Phenotype Dynamics Measurement
Genetic barcoding technologies enable quantitative measurement of phenotype dynamics during cancer drug resistance evolution [42]. This approach facilitates tracking of clonal dynamics without direct measurement of resistance phenotypes, using mathematical modeling to infer evolutionary behaviors.
Table: Research Reagent Solutions for Lineage Tracing Studies
| Reagent/Technology | Function | Application in Extinction Therapy |
|---|---|---|
| Lentiviral barcoding | Unique genetic labeling of cells | Tracking clonal dynamics and lineage relationships |
| scRNA-seq | Single-cell transcriptomic profiling | Characterizing phenotypic heterogeneity |
| scDNA-seq | Single-cell DNA sequencing | Identifying genetic alterations |
| WST-1/MTT assays | Cell viability quantification | Measuring drug response and resistance |
| Pharmacokinetic modeling | Simulating drug concentration effects | Predicting phenotypic transitions under treatment |
Protocol: Genetic Lineage Tracing for Resistance Evolution
- Cell line preparation: Utilize colorectal cancer cell lines (e.g., SW620, HCT116) or other appropriate models
- Lentiviral barcoding: Infect parental cells with lentivirus containing unique genetic barcodes
- Expansion and replication: Expand barcoded population and split into multiple replicate populations
- Drug treatment regimen: Apply periodic chemotherapy (e.g., 5-FU) with defined sequences and timing
- Population sampling: Collect cells at predetermined time points during treatment
- Barcode sequencing: Extract and sequence barcodes to track lineage abundances
- Mathematical modeling: Apply inference frameworks to determine phenotype dynamics from lineage tracing data [42]
Three mathematical models of increasing complexity can be employed to interpret lineage tracing data:
- Model A (Unidirectional transitions): Sensitive cells transition to resistant state
- Model B (Bidirectional transitions): Includes reversible transitions between states
- Model C (Escape transitions): Incorporates drug-dependent emergence of fit resistant phenotypes [42]
Development of Drug-Resistant Cell Lines
Protocol: Generating Drug-Resistant Cell Lines for Sequential Therapy Testing
- Cell culture initiation: Culture parental cancer cells (e.g., DU-145 prostate cancer cells) in complete medium (RPMI-1640 + 1% pen-strep + 10% FBS) at 37°C, 5% CO₂ until 80% confluent [43]
- IC₅₀ determination:
- Seed cells in 96-well plates at 1.0 × 10⁴ cells/well
- Prepare serial drug dilutions (e.g., paclitaxel at 0, 0.1, 0.5, 1, 2, 4, 10, 20, 40, 80, 160, 320, 620, 1280 nM)
- Incubate for 48 hours, add WST-1 reagent, and measure absorbance at 450nm (reference 650nm)
- Calculate cell viability: [(As-Ab)/(Ac-Ab)] × 100 where As=sample, Ab=blank, Ac=control
- Determine IC₅₀ using nonlinear regression (four-parameter logistic model) [43]
- Stepwise resistance induction:
- Seed parental cells at 2.0 × 10⁶ cells/100mm dish
- Initial exposure: Add drug at IC₁₀-IC₂₀ concentration for 2 days
- Recovery: Replace with drug-free medium until 80% confluent
- Passage cells and cryopreserve aliquots
- Subsequent exposures: Increase drug concentration 1.5-2.0 fold each cycle
- Repeat process until significantly elevated IC₅₀ confirmed in resistant lines [43]
Implementation Framework for Extinction Therapy
Therapeutic Sequencing Strategies
The core principle of extinction therapy involves initial reductive treatment followed by exploitation of the resulting eco-evolutionary vulnerabilities [39]. This approach mirrors successful eradication campaigns against invasive species, such as the Galápagos goats, where initial hunting (first strike) reduced the population by 90%, followed by "Judas goat" tactics (second strike) to eliminate the remaining resistant individuals [39].
Rational Drug Sequencing Protocol:
- First strike - reductive phase: Apply initial therapy to reduce tumor burden and diversity
- Monitoring phase: Assess population decline and emergence of resistance
- Second strike - extinction phase: Implement alternative therapies that exploit specific vulnerabilities of the diminished population
- Consolidation: Apply additional perturbations to prevent population recovery
The following diagram illustrates the conceptual framework of extinction therapy:
Quantitative Framework for Drug Sequencing
The efficacy of sequential therapy depends on multiple parameters that can be optimized through evolutionary modeling:
Table: Parameters for Optimizing Sequential Therapy
| Parameter | Description | Measurement Approach | Therapeutic Implication |
|---|---|---|---|
| Switching rate | Frequency of drug alternation | Experimental evolution with different switching intervals | Fast switching can prevent adaptation to any single drug [40] |
| Spontaneous resistance rate | Probability of resistance emergence to single drug | Fluctuation analysis or lineage tracing | Drugs with lower spontaneous resistance preferred for sequences [40] |
| Cross-resistance level | Degree of resistance overlap between drugs | Resistance profiling of evolved populations | Low cross-resistance pairs maximize sequential therapy efficacy [40] |
| Collateral sensitivity | Resistance to one drug increases sensitivity to another | Pairwise resistance screening | Exploit trade-offs to design effective sequences [40] |
| Fitness cost of resistance | Growth disadvantage of resistant cells in absence of drug | Competitive growth assays | Higher costs enable containment strategies |
Integration with Artificial Intelligence and Evolutionary Modeling
Artificial intelligence (AI) approaches are increasingly valuable for optimizing extinction therapy strategies. AI can analyze large biological datasets to identify key biomarkers and molecular pathways associated with resistance, predict drug-target interactions, and optimize drug combination strategies [44]. Machine learning algorithms can integrate multisource heterogeneous data including omics data, medical images, and electronic medical records to identify resistance features and construct predictive models [44].
AI-Driven Workflow for Extinction Therapy:
- Data collection: Aggregate clinical, genomic, transcriptomic, proteomic, and imaging data
- Preprocessing: Clean, standardize, and perform feature selection on heterogeneous datasets
- Modeling: Apply machine learning algorithms (SVM, random forest, deep learning) to identify resistance patterns
- Validation: Cross-validate models and verify with experimental studies
- Interpretation: Use explainable AI (e.g., SHAP values) to interpret model predictions
- Clinical translation: Continuously optimize models with new clinical data [44]
This AI-facilitated approach can identify novel therapeutic sequences that exploit evolutionary vulnerabilities in cancer populations, potentially predicting collateral sensitivity patterns that inform optimal drug sequencing strategies.
Extinction therapy represents a paradigm shift in cancer treatment, moving beyond the maximum kill approach to strategically steer tumor evolution toward eradication. By integrating evolutionary dynamics, rational drug sequencing, and advanced monitoring technologies, this approach exploits fundamental ecological principles to overcome the challenge of therapy resistance. The protocols outlined here provide a framework for implementing extinction therapy in both experimental and clinical settings, with the potential to significantly improve outcomes for patients with metastatic cancers.
A primary cause of treatment failure in oncology is the evolution of drug resistance within tumor cell populations. The vast information content of the human genome provides cancer cells with a remarkable capacity to deploy adaptive strategies, making the emergence of resistance mechanisms to virtually any single-agent therapy virtually inevitable [1]. However, the clinical manifestation of resistance depends not merely on the emergence of these mechanisms but on the proliferation of resistant phenotypes—a process governed by complex Darwinian dynamics involving trade-offs between the costs and benefits of resistance traits in the context of the local microenvironment and competing cellular populations [1]. This understanding has prompted a paradigm shift from traditional maximum tolerated dose (MTD) strategies, which often accelerate competitive release of resistant clones, toward evolutionary-informed therapies that seek to actively manage and constrain tumor evolution [1] [45].
Synthetic biology offers a revolutionary toolkit to address this challenge by programming tumor evolution itself. Rather than simply targeting cancer cells, synthetic biology enables the engineering of sophisticated genetic circuits that can be introduced into cancer cells to alter their evolutionary trajectory. These approaches exploit the same selective pressures that drive resistance to proactively steer tumor populations toward more therapeutic-sensitive states or to engineer their self-destruction [46]. This Application Note details the core principles, experimental protocols, and key reagents for implementing synthetic biology solutions to redirect tumor evolution, with a specific focus on selection gene drive systems.
Core Concept: Selection Gene Drives for Tumor Stabilization
Selection gene drives represent a novel synthetic biology framework that couples an inducible fitness advantage with a shared fitness cost to redirect evolutionary trajectories in tumor populations. The system is designed to leverage the selective pressure of anticancer drugs to drive the propagation of therapeutic transgenes that fundamentally alter the tumor's response to treatment [46].
Theoretical Foundation and Design Criteria
The conceptual foundation for selection gene drives builds upon evolutionary game theory and ecological models of tumor progression. Mathematical modeling suggests that tumors can be driven toward a stable polymorphic equilibrium comprising both therapy-sensitive and resistant subpopulations, preventing the uncontrolled expansion of fully resistant clones [45]. Stochastic models of evolutionary dynamics have identified key design criteria for effective selection gene drives [46]:
- Tight Coupling: The fitness advantage and cost must be inextricably linked within the same genetic construct.
- Inducible Fitness Advantage: The selective benefit must be activatable by a specific therapeutic agent.
- Therapeutic Coupling: The system must be designed to harness the selective pressure of clinically approved targeted therapies.
- Diverse Lethal Mechanisms: The system should employ distinct therapeutic mechanisms to overcome pre-existing genetic heterogeneity.
Table 1: Quantitative Parameters for Selection Gene Drive Design
| Parameter | Design Consideration | Optimal Range |
|---|---|---|
| Switch Engagement Threshold | Minimum drug concentration required for selective advantage | 10-50% of MTD |
| Fitness Cost | Baseline growth impairment from drive system | <20% reduction |
| Selective Advantage | Fitness benefit during drug exposure | 2-5x relative growth advantage |
| Escape Frequency | Rate of system failure or bypass | <10⁻⁶ in vitro |
Molecular Mechanism of Action
A selection gene drive system typically comprises two genetically encoded "switches" that function in concert:
- The Sensor Switch: Confers a drug-dependent fitness advantage, often through resistance to a targeted therapeutic agent.
- The Effector Switch: Introduces a shared vulnerability or therapeutic susceptibility, such as enzyme-prodrug activation or immune sensitization.
When tumor cells containing the gene drive are exposed to the targeted therapy, cells with functional sensor switches gain a immediate selective advantage. However, this simultaneously promotes the propagation of the linked effector switch, which enables novel therapeutic interventions that can eliminate the entire population regardless of its original resistance profile [46].
Experimental Protocols
Protocol 1: In Vitro Validation of Selection Gene Drive Systems
Objective: To quantitatively assess the dynamics of selection gene drive propagation and its efficacy against pre-existing genetic resistance in controlled cell culture systems.
Materials:
- Cancer cell lines with relevant genetic backgrounds (e.g., EGFR-mutant for osimertinib-based drives)
- Selection gene drive constructs (lentiviral or retroviral vectors)
- Targeted therapeutic agents (e.g., tyrosine kinase inhibitors)
- Effector agents (e.g., prodrugs for activated catalysis)
- Cell culture reagents and equipment
- Flow cytometry system for tracking fluorescent markers
- Incucyte or similar real-time cell analysis system
Procedure:
Cell Line Engineering:
- Transduce target cancer cell lines with selection gene drive constructs at MOI 5-10.
- Include separate populations with effector-only and sensor-only constructs as controls.
- Select stable populations with appropriate antibiotics for 7-14 days.
- FACS-sort populations to >95% purity based on fluorescent markers.
Mixed Population Competition Assays:
- Mix gene drive-engineered cells with unengineered cells at defined ratios (1:9, 1:1, 9:1).
- Plate 1×10⁵ cells per well in 12-well plates in triplicate for each condition.
- Treat cultures with:
- No drug control
- Targeted therapy only (e.g., 100 nM osimertinib)
- Effector agent only (e.g., 5-fluorocytosine for cytosine deaminase systems)
- Combination therapy (sequential or concurrent)
- Passage cells every 3-4 days, maintaining drug treatments.
Time-Series Monitoring:
- Sample cells every 48-72 hours for flow cytometry analysis of fluorescent markers.
- Quantify cell viability using trypan blue exclusion or ATP-based assays.
- Extract genomic DNA at days 0, 7, 14, and 21 for qPCR quantification of construct abundance.
Data Analysis:
- Calculate relative fitness (ω) as the ratio of growth rates between engineered and control populations.
- Determine escape frequency by plating 1×10⁶ cells in selective conditions and counting resistant colonies after 14 days.
- Model population dynamics using modified Lotka-Volterra competition equations.
Troubleshooting:
- Low transduction efficiency: Optimize viral titer or consider alternative transfection methods.
- High escape frequency: Verify construct integrity and consider additional safeguards.
- Incomplete population control: Titrate effector agent concentration and timing.
Protocol 2: In Vivo Evaluation in Mouse Models of Solid Tumors
Objective: To validate selection gene drive efficacy in spatially structured, immunocompetent tumor microenvironments and assess therapeutic impact on pre-existing resistance.
Materials:
- Immunocompromised (NSG) or humanized mouse models
- Patient-derived xenografts (PDXs) or cell line-derived xenografts (CDXs)
- Selection gene drive-engineered cancer cells
- Therapeutic agents: targeted inhibitors and corresponding prodrugs/effectors
- In vivo imaging system (IVIS) for bioluminescent tracking
- Equipment for intracardiac, intravenous, or orthotopic injections
Procedure:
Tumor Initiation:
- Implant 5×10⁵ gene drive-engineered cells mixed with 5×10⁵ wild-type cells (1:1 ratio) subcutaneously or orthotopically into 8-12 week-old mice.
- Include control groups with wild-type cells only and effector-only engineered cells.
- Monitor tumor growth via caliper measurements 3 times weekly.
Therapeutic Intervention:
- When tumors reach 100-200 mm³, randomize mice into treatment groups (n=8-10):
- Vehicle control
- Targeted therapy alone (e.g., osimertinib, 25 mg/kg daily by oral gavage)
- Effector agent alone (e.g., 5-fluorocytosine, 500 mg/kg i.p. daily)
- Sequential therapy (targeted therapy followed by effector agent)
- Concurrent combination therapy
- Continue treatment for 4-6 weeks or until tumor volume exceeds ethical endpoints.
- When tumors reach 100-200 mm³, randomize mice into treatment groups (n=8-10):
Longitudinal Monitoring:
- Measure tumor dimensions 3 times weekly to calculate volume (V = 0.5 × length × width²).
- Perform IVIS imaging weekly for bioluminescent tracking of tumor burden.
- Collect blood samples weekly for circulating tumor DNA (ctDNA) analysis of drive construct prevalence.
Endpoint Analysis:
- Euthanize mice at study endpoint or when tumors reach 1500 mm³.
- Harvest tumors and process for:
- Single-cell suspension for flow cytometry
- Formalin-fixed, paraffin-embedded sections for IHC
- Snap-frozen tissue for DNA/RNA extraction
- Quantify tumor burden in metastatic organs via ex vivo bioluminescence.
Data Analysis:
- Compare tumor growth curves between treatment groups using mixed-effects models.
- Calculate time-to-progression and survival benefit.
- Correlate drive construct prevalence in ctDNA with therapeutic response.
Diagram 1: Experimental Workflow for Selection Gene Drive Development
The Scientist's Toolkit: Key Research Reagents
Table 2: Essential Reagents for Synthetic Biology Approaches to Redirect Tumor Evolution
| Reagent Category | Specific Examples | Function/Application |
|---|---|---|
| Vector Systems | Lentiviral vectors, Retroviral vectors, Transposon systems (Sleeping Beauty, PiggyBac) | Stable delivery and genomic integration of genetic circuits |
| Sensor Switches | Drug-responsive promoters (tetracycline-inducible), Engineered resistance genes (EGFR-T790M), Chimeric antigen receptors | Confer selective advantage in response to specific therapeutics |
| Effector Switches | Suicide genes (HSV-TK, cytosine deaminase), Immune modulators (secreted cytokines, surface engagers), Prodrug-converting enzymes | Introduce novel vulnerabilities or therapeutic susceptibilities |
| Selection Agents | Tyrosine kinase inhibitors (osimertinib, pralsetinib), Antibiotics (puromycin, blasticidin), Prodrugs (ganciclovir, 5-fluorocytosine) | Apply selective pressure to drive system propagation |
| Tracking Systems | Fluorescent proteins (GFP, RFP, mCherry), Luciferase reporters, Cell surface markers (CDy, tNGFR) | Monitor system propagation and population dynamics |
| Analytical Tools | Flow cytometry, Single-cell RNA sequencing, ddPCR for construct quantification, Phylogenetic analysis software | Quantify system performance and evolutionary dynamics |
Pathway Visualization and Logical Framework
Diagram 2: Selection Gene Drive Mechanism of Action
Integration with Evolutionary Modeling
The effective implementation of synthetic biology approaches requires tight integration with evolutionary modeling to predict and optimize therapeutic outcomes. The SDevo (state-dependent evolutionary phylodynamic) framework enables quantification of spatially varying birth rates in tumors, revealing that cells on the tumor periphery can divide 3-6 times faster than those in the interior [47]. This differential growth rate creates characteristic genetic signatures that can be exploited for timing therapeutic interventions.
Evolutionary models further indicate that successful tumor control requires maintaining a stable polymorphic heterogeneity of sensitive and resistant cells rather than complete eradication of sensitive populations [45]. Optimal control theory applied to these models suggests that dose titration protocols, starting with lower doses and gradually increasing, can achieve tumor stabilization across a wide range of initial tumor compositions [45]. This approach stands in direct contrast to traditional MTD strategies and aligns with the programmable control enabled by synthetic gene drive systems.
Synthetic biology approaches represent a paradigm shift in cancer therapy by moving from reactive strategies that target cancer cells as they exist to proactive programming that directs tumor evolution toward therapeutic vulnerability. Selection gene drives exemplify this approach by harnessing the selective pressures that typically drive resistance to instead propagate therapeutic vulnerabilities through tumor populations.
Future developments in this field will likely focus on increasing the sophistication of genetic circuits to include multi-input logic gates that respond to specific tumor microenvironment conditions, integrating fail-safe mechanisms to prevent unintended consequences, and combining synthetic circuits with immunotherapeutic approaches to engage endogenous immune responses. As these technologies mature, they will increasingly be guided by evolutionary modeling that predicts tumor trajectory and optimizes intervention timing, ultimately enabling truly personalized, evolution-informed cancer therapy.
Navigating Implementation Challenges: Technical and Clinical Translation Barriers
Evolutionary cancer therapy (ECT) represents a paradigm shift in oncology, focusing on controlling rather than eradicating cancer by leveraging competition between drug-sensitive and resistant cell populations [2]. This adaptive approach requires continuous, multidimensional monitoring of tumor dynamics to guide treatment decisions. The success of ECT hinges on frequent, precise assessment of tumor burden and clonal evolution, moving beyond static snapshots to a dynamic understanding of tumor behavior [48] [2]. Liquid biopsies and radiomics have emerged as complementary, minimally invasive technologies that provide the real-time data essential for implementing adaptive treatment protocols. By integrating circulating biomarkers with quantitative imaging features, clinicians can monitor therapeutic response, detect emergent resistance, and adjust treatment strategies before clinical progression becomes evident [49] [2]. This application note provides detailed methodologies and frameworks for implementing these monitoring technologies within ECT clinical trials and practice.
Biomarker Classes for Tracking Tumor Evolution
Comparative Analysis of Key Biomarkers in Liquid Biopsy
Table 1: Key Liquid Biopsy Biomarkers for Monitoring Tumor Dynamics
| Biomarker | Biological Source | Clinical Significance | Associated Technologies | Applications in ECT |
|---|---|---|---|---|
| Circulating Tumor Cells (CTCs) | Cells shed from primary/metastatic tumors | Direct insight into tumor heterogeneity, metastatic potential, and therapeutic resistance [48] | Microfluidic enrichment, immunoaffinity capture, single-cell RNA sequencing [48] [9] | Monitoring clonal dynamics, identifying resistant subpopulations, longitudinal phenotypic analysis |
| Circulating Tumor DNA (ctDNA) | DNA fragments from apoptotic/necrotic tumor cells | Detection of tumor-specific mutations, copy number variations, methylation signatures [48] | ddPCR, NGS panels, methylation profiling [48] | Tracking minimal residual disease, early relapse detection, monitoring evolution of resistance mutations |
| Extracellular Vesicles (EVs) | Nano-sized vesicles secreted by tumor cells | Carry proteins, lipids, nucleic acids; mediate intercellular communication [48] | Ultracentrifugation, size-exclusion chromatography, nanoparticle tracking [48] | Assessing tumor microenvironment crosstalk, monitoring drug resistance mechanisms |
| Tumor-Educated Platelets (TEPs) | Platelets altered by tumor interactions | RNA and protein profile changes indicating cancer progression [50] | RNA sequencing, mass spectrometry [50] | Accessible biomarker source for longitudinal monitoring, particularly in central nervous system malignancies |
Integration of Multi-Modal Biomarkers in ECT
The synergistic integration of multiple biomarker classes provides a comprehensive view of tumor evolution that is essential for ECT. While CTCs offer direct cellular information including phenotypic plasticity and metastatic potential, ctDNA provides a broader representation of tumor heterogeneity through its short half-life and distribution throughout the bloodstream [48]. EVs and TEPs contribute additional layers of molecular information about tumor-stroma interactions and systemic effects [50]. In ECT protocols, combining these biomarkers enables more accurate assessment of tumor burden dynamics and competitive interactions between sensitive and resistant cell populations, allowing for optimized treatment scheduling and dosing decisions [2].
Experimental Protocols for Liquid Biopsy Analysis
CTC Isolation and Characterization Protocol
Principle: CTCs are extremely rare (approximately 1-10 cells/mL of blood) compared to hematopoietic cells, requiring sophisticated enrichment and detection strategies [48]. Their molecular characterization provides direct insights into tumor heterogeneity and treatment resistance mechanisms.
Materials:
- EDTA or CellSave blood collection tubes
- Density gradient medium (e.g., Ficoll-Paque)
- Microfluidic enrichment device (e.g., CTC-iChip, IsoFlux)
- EpCAM or other epithelial marker antibodies for immunoaffinity capture
- Cell fixation and permeabilization reagents
- Immunofluorescence staining antibodies (CK, CD45, DAPI)
- Single-cell whole transcriptome amplification kit
- Next-generation sequencing library preparation kit
Procedure:
Blood Collection and Processing:
- Collect 10mL peripheral blood into EDTA or CellSave tubes.
- Process within 4-96 hours of collection (optimize based on preservation system).
- Separate mononuclear cells using density gradient centrifugation (400 × g, 30 minutes).
CTC Enrichment:
- Option A - Microfluidic Enrichment: Load blood sample onto microfluidic device (e.g., CTC-iChip). Use deterministic lateral displacement and inertial focusing for size-based separation, followed by magnetophoretic sorting of immunolabeled cells [48].
- Option B - Immunoaffinity Capture: Incubate blood sample with antibody-coated magnetic beads (e.g., anti-EpCAM). Separate labeled cells using magnetic separation columns. Wash thoroughly to remove unbound cells.
CTC Identification and Enumeration:
- Fix enriched cells with 4% paraformaldehyde for 15 minutes.
- Permeabilize with 0.1% Triton X-100 for 5 minutes.
- Perform immunofluorescence staining: Cytokeratin (CK-FITC, epithelial marker), CD45 (PE, leukocyte marker), and DAPI (nuclear stain).
- Image using fluorescence microscopy or automated scanning system.
- Identify CTCs as CK+/CD45-/DAPI+ cells. Calculate CTCs per mL of blood.
Molecular Characterization:
- For single-cell analysis, individually pick CTCs using micromanipulation or microfluidics.
- Perform whole transcriptome amplification using commercial kit.
- Prepare sequencing libraries and sequence using NGS platform (e.g., Illumina).
- Analyze data for expression profiles, mutations, and copy number variations.
Quality Control:
- Include spike-in controls of known cancer cells for recovery assessment.
- Process healthy donor blood as negative control.
- Perform replicate analyses to assess technical variability.
Applications in ECT: This protocol enables monitoring of clonal dynamics during therapy, identification of resistant subpopulations, and assessment of phenotypic plasticity through longitudinal analysis [48] [2].
ctDNA Analysis Protocol for Mutation Tracking
Principle: ctDNA comprises short DNA fragments (∼170 bp) released into circulation from apoptotic and necrotic tumor cells. Detection of tumor-specific alterations in ctDNA allows non-invasive monitoring of tumor burden and genomic evolution [48].
Materials:
- Cell-free DNA blood collection tubes (e.g., Streck)
- Plasma preparation tubes
- DNA extraction kit (silica membrane or magnetic bead-based)
- Qubit fluorometer and dsDNA HS assay kit
- Digital PCR system or NGS library preparation kit
- Target enrichment reagents (e.g., hybrid capture baits)
- Bioanalyzer or TapeStation system
Procedure:
Blood Collection and Plasma Separation:
- Collect 10mL blood into cell-free DNA preservation tubes.
- Invert gently 8-10 times for proper mixing.
- Centrifuge at 1600 × g for 20 minutes at room temperature to separate plasma.
- Transfer plasma to fresh tube without disturbing buffy coat.
- Perform second centrifugation at 16,000 × g for 10 minutes to remove residual cells.
- Aliquot plasma and store at -80°C if not processing immediately.
Cell-Free DNA Extraction:
- Thaw plasma samples on ice if frozen.
- Extract DNA using commercial kit following manufacturer's protocol.
- Elute DNA in low-EDTA TE buffer or nuclease-free water.
- Quantify DNA using fluorometric method (e.g., Qubit).
- Assess fragment size distribution using Bioanalyzer.
Mutation Detection:
- Option A - Digital PCR: Design and validate assays for specific mutations of interest. Prepare reaction mix with DNA, primers, probes, and digital PCR supermix. Partition samples into thousands of nanoliter-sized droplets or wells. Amplify using thermal cycler. Analyze using droplet reader to count mutant and wild-type molecules. Calculate mutant allele frequency.
- Option B - Next-Generation Sequencing: Prepare sequencing libraries from 10-50ng ctDNA. Use unique molecular identifiers to correct for amplification bias and enable absolute quantification. Perform hybrid capture-based target enrichment using panels covering relevant cancer genes. Sequence on NGS platform with minimum 10,000x raw coverage.
Data Analysis:
- For dPCR data, calculate variant allele frequency (VAF) as mutant/(mutant + wild-type) molecules.
- For NGS data, align sequences to reference genome, call variants using validated pipelines, and calculate VAF.
- Monitor VAF changes longitudinally to track clonal dynamics.
Quality Control:
- Include negative controls (water) and positive controls (synthetic reference standards).
- Monitor extraction efficiency using spike-in synthetic DNA fragments.
- Establish limit of detection for each assay using dilution series.
Applications in ECT: This protocol enables detection of minimal residual disease, monitoring of tumor burden dynamics, and identification of emerging resistance mutations to guide adaptive therapy decisions [48] [2].
Figure 1: Liquid Biopsy Workflow for Evolutionary Cancer Therapy Monitoring
Radiomics Protocols for Quantitative Imaging Biomarkers
Radiomics Feature Extraction and Analysis Protocol
Principle: Radiomics involves extracting high-dimensional quantitative features from medical images that reflect tumor heterogeneity, phenotype, and microenvironment [51]. These imaging biomarkers provide complementary information to liquid biopsies, capturing spatial heterogeneity and enabling whole-tumor assessment.
Materials:
- DICOM images from CT, MRI, or PET/CT scanners
- Image preprocessing software (e.g., 3D Slicer, Python packages)
- Tumor segmentation tools (semi-automated or manual)
- Radiomics feature extraction platform (e.g., PyRadiomics)
- Statistical analysis software (R, Python with scikit-learn)
- High-performance computing resources for deep learning models
Procedure:
Image Acquisition and Standardization:
- Acquire images using standardized protocols with consistent parameters (slice thickness, reconstruction kernel, contrast timing).
- For multi-center studies, implement phantom-based calibration to harmonize imaging data.
- Convert all images to standardized orientation and voxel spacing.
Tumor Segmentation:
- Manual Segmentation: Experienced radiologists delineate tumor boundaries slice-by-slice using appropriate software.
- Semi-Automated Segmentation: Use region-growing or graph-cut algorithms with manual correction.
- Deep Learning Segmentation: Implement pre-trained neural networks (e.g., U-Net) for automated segmentation with quality control.
- Generate 3D volume-of-interest (VOI) masks in DICOM-RT format.
Image Preprocessing:
- Resample all images to isotropic voxel spacing (e.g., 1×1×1 mm³).
- Apply intensity discretization with fixed bin width (recommended: 25 HU for CT).
- Perform intensity normalization (e.g., z-score) to reduce scanner-specific effects.
- For MRI, apply bias field correction and intensity standardization.
Feature Extraction:
- Use standardized radiomics software (e.g., PyRadiomics) to extract features.
- Extract first-order statistics (intensity-based features: mean, entropy, kurtosis).
- Extract shape-based features (3D characteristics: volume, sphericity, surface area).
- Extract texture features using:
- Gray Level Co-occurrence Matrix (GLCM)
- Gray Level Run Length Matrix (GLRLM)
- Gray Level Size Zone Matrix (GLSZM)
- Neighborhood Gray Tone Difference Matrix (NGTDM)
- Apply wavelet and Laplacian of Gaussian filters for transformed image features.
Feature Selection and Model Building:
- Perform intraclass correlation coefficient (ICC) analysis to identify reproducible features (ICC > 0.8).
- Apply variance thresholding to remove non-informative features.
- Use correlation analysis and recursive feature elimination to reduce dimensionality.
- Develop predictive models using machine learning algorithms (random forest, support vector machines, neural networks).
- Validate models using cross-validation and independent test sets.
Quality Assurance:
- Assess inter-observer variability in segmentation through dice similarity coefficient.
- Implement feature stability analysis using test-retest imaging.
- Use phantom studies to quantify technical variability.
Applications in ECT: Radiomics features can predict tumor behavior, assess spatial heterogeneity, and monitor response to therapy, providing critical information for adapting treatment strategies in ECT protocols [2] [51].
Figure 2: Radiomics Workflow for Tumor Dynamics Assessment
Integrated Monitoring Framework for Adaptive Therapy
Temporal Monitoring Protocol for ECT
Principle: ECT requires frequent assessment of tumor dynamics to guide treatment adjustments [2]. This protocol integrates liquid biopsy and radiomics data to inform decisions about treatment dosing, scheduling, and drug sequencing.
Materials:
- Blood collection supplies for liquid biopsy
- Imaging equipment for radiomics
- Data integration platform
- Mathematical modeling software
- Clinical decision support system
Procedure:
Baseline Assessment:
- Perform comprehensive tumor staging with CT, MRI, or PET/CT.
- Collect baseline blood samples for CTC enumeration and ctDNA analysis.
- Establish mutational profile and identify targetable alterations.
- Calculate initial tumor burden using quantitative imaging.
Treatment Initiation:
- Begin therapy according to ECT protocol (continuous, metronomic, or pulsed dosing).
- Establish monitoring schedule based on expected dynamics (typically 2-4 week intervals).
Longitudinal Monitoring:
- Liquid Biopsy Sampling: Collect blood every 2-4 weeks for:
- CTC enumeration and characterization
- ctDNA mutation tracking
- EV analysis for resistance markers
- Radiomic Assessment: Perform imaging every 8-12 weeks:
- Quantitative tumor volume measurement
- Radiomic feature extraction
- Heterogeneity assessment
- Clinical Assessment: Monitor symptoms, performance status, and conventional biomarkers.
- Liquid Biopsy Sampling: Collect blood every 2-4 weeks for:
Data Integration and Decision Points:
- Integrate multi-parametric data using dedicated software platform.
- Apply mathematical models to predict tumor dynamics [2].
- Trigger treatment modifications based on predefined thresholds:
- Treatment holiday when tumor burden decreases by ≥50%
- Treatment resumption when tumor burden returns to baseline
- Dose modulation based on rate of regrowth
- Drug switching upon emergence of specific resistance mutations
Resistance Management:
- Monitor for emergence of resistant subclones through ctDNA mutation analysis.
- Characterize phenotypic changes in CTCs (EMT, stem-like markers).
- Adapt therapy to suppress resistant populations (extinction therapy, double-bind approaches) [2].
Implementation Considerations:
- Establish clear thresholds for treatment modification based on tumor type and therapeutic agents.
- Develop standardized response criteria for integrated biomarkers.
- Implement quality control measures across multiple sampling timepoints.
- Use secure data management systems for longitudinal data tracking.
The Scientist's Toolkit: Essential Research Reagents and Materials
Table 2: Essential Research Reagents for Tumor Dynamics Monitoring
| Category | Specific Reagents/Systems | Application | Key Considerations |
|---|---|---|---|
| Blood Collection & Preservation | CellSave tubes, Streck cfDNA tubes, EDTA tubes | Sample integrity maintenance | Choice affects stability: CellSave preserves cells, Streck preserves cfDNA |
| Nucleic Acid Extraction | QIAamp Circulating Nucleic Acid Kit, Maxwell RSC ccfDNA Plasma Kit | Isolation of ctDNA, EV-RNA | Recovery efficiency, fragment size bias, inhibitor removal |
| CTC Enrichment | CTC-iChip (BioCEPT), IsoFlux System, CellSearch System | Rare cell isolation | Purity, viability, platform-specific biases (epithelial vs. unbiased) |
| Single-Cell Analysis | SMART-Seq v4 Ultra Low Input Kit, 10x Genomics Chromium | Transcriptomic profiling | Sensitivity, coverage, molecular completeness |
| Sequencing | Illumina TSO500, AVENIO ctDNA Analysis Kits, TruSight Oncology | Mutation detection | Coverage uniformity, limit of detection, turnaround time |
| Image Analysis | 3D Slicer, PyRadiomics, ITK-SNAP | Radiomic feature extraction | Reproducibility, standardization, computational requirements |
| Data Integration | R, Python with scikit-learn, TensorFlow | Predictive modeling | Model interpretability, validation requirements, clinical implementation |
The integration of liquid biopsy biomarkers and radiomics provides a powerful framework for monitoring tumor dynamics in evolutionary cancer therapy. The protocols outlined in this document enable researchers and clinicians to implement comprehensive monitoring strategies that capture both temporal and spatial heterogeneity of tumors. By combining molecular data from circulating biomarkers with quantitative imaging features, ECT protocols can be optimized through adaptive decision-making based on real-time assessment of tumor evolution and therapeutic response. As these technologies continue to mature, their systematic implementation in clinical trials and practice will be essential for realizing the full potential of evolutionary approaches to cancer control.
Adaptive Therapy (AT) represents a paradigm shift in oncology, moving from the traditional goal of maximum tumor cell kill towards long-term disease control by exploiting evolutionary principles. This approach aims to suppress resistant tumor phenotypes by maintaining a stable population of therapy-sensitive cells that can competitively suppress the growth of resistant populations through dynamic dose modulation. Treatment is cycled on and off based on tumor burden measurements, allowing sensitive cells to rebound during treatment breaks and suppress resistant clones that often bear fitness costs in drug-free environments [52].
However, the success of this strategy faces a significant challenge: non-genetic resistance mechanisms. Unlike genetic resistance caused by permanent mutations, non-genetic resistance encompasses dynamic, reversible adaptations including epigenetic reprogramming, cell state transitions, and microenvironment-mediated protection. These mechanisms can rapidly increase the resistant population at the expense of the sensitive one, fundamentally undermining the competitive dynamics that adaptive therapy seeks to exploit [52] [53] [54]. This article explores these mechanisms and provides practical experimental approaches for their investigation within evolutionary modeling frameworks.
Key Non-Genetic Resistance Mechanisms
Epithelial-to-Mesenchymal Transition (EMT) and Cellular Plasticity
EMT represents a fundamental cellular plasticity program that enables cancer cells to transition from epithelial states to mesenchymal phenotypes, enhancing invasiveness, metastatic potential, and therapeutic resistance. This transition involves profound transcriptional reprogramming that reduces drug sensitivity through multiple pathways.
- Molecular Drivers: Key transcription factors including SNAIL, SLUG, ZEB1, and TWIST orchestrate EMT, repressing epithelial markers like E-cadherin while inducing mesenchymal markers such as vimentin and N-cadherin [9].
- Impact on Adaptive Therapy: Cells undergoing EMT often enter a slow-cycling, drug-tolerant state that allows survival during treatment cycles. When therapy is withdrawn, these persistent cells can serve as reservoirs for tumor regrowth, potentially accelerating rather than suppressing resistance development [53] [55].
Tumor Microenvironment (TME)-Mediated Protection
The tumor microenvironment creates physical and biochemical sanctuaries that shield cancer cells from therapeutic effects, independently of genetic mutations.
- Mechanisms of Protection:
- Physical Barrier: The extracellular matrix (ECM) and abnormal vasculature restrict drug penetration to tumor regions [52] [56].
- Stromal Signaling: Cancer-associated fibroblasts (CAFs) secrete growth factors and cytokines that promote cancer cell survival under therapeutic pressure [52].
- Metabolic Adaptation: Hypoxic regions within tumors induce metabolic shifts that reduce dependence on pathways targeted by therapies [57].
Drug Efflux Pump Overexpression
The overexpression of ATP-binding cassette (ABC) transporters represents a rapid adaptation mechanism that directly expels therapeutic agents from cancer cells.
- Key Players: P-glycoprotein (P-gp/ABCB1), multidrug resistance-associated proteins (MRPs/ABCC family), and breast cancer resistance protein (BCRP/ABCG2) are frequently implicated in chemotherapeutic resistance [52] [54].
- Regulation: These efflux pumps can be transcriptionally upregulated in response to therapeutic stress through both genetic and non-genetic mechanisms, with studies identifying PKCϵ as a regulator of P-gp expression in Acute Myeloid Leukemia [54].
Heat Shock Protein-Mediated Stress Adaptation
Heat shock proteins (HSPs) constitute an evolutionarily conserved cellular defense system that promotes cancer cell survival under various TME stressors.
- Functional Roles: HSPs function as molecular chaperones that stabilize oncoproteins, inhibit apoptosis, and maintain proteostasis under nutrient deprivation, hypoxia, and genotoxic stress [57].
- Therapeutic Implications: HSP synthesis is significantly upregulated in cancer cells, facilitating adaptation to therapeutic insults and contributing to multidrug resistance phenotypes that challenge adaptive cycling approaches [57].
Table 1: Major Non-Genetic Resistance Mechanisms and Their Impact on Adaptive Therapy
| Mechanism | Key Molecular Players | Effect on Tumor Dynamics | Impact on Adaptive Therapy |
|---|---|---|---|
| EMT & Cellular Plasticity | SNAIL, SLUG, ZEB1, TWIST, Vimentin | Increased invasiveness, drug-tolerant persister states | Rapid phenotypic switching bypasses competitive suppression |
| TME-Mediated Protection | CAFs, ECM, abnormal vasculature, hypoxia | Physical drug barriers, survival signaling | Creates sanctuary sites resistant to therapy cycling |
| Drug Efflux Pumps | P-gp, MRPs, BCRP | Reduced intracellular drug concentration | Diminishes efficacy of each treatment cycle |
| Heat Shock Proteins | HSP90, HSP70, HSP27 | Enhanced stress tolerance, protein stability | Promotes survival during treatment phases |
| Epigenetic Reprogramming | DNA methylation, histone modifications | Transcriptional adaptation without DNA mutation | Enables rapid, reversible resistance states |
Quantitative Assessment of Non-Genetic Resistance
The following table summarizes key quantitative findings from clinical and preclinical studies investigating non-genetic resistance and adaptive therapy outcomes:
Table 2: Quantitative Clinical and Preclinical Evidence of Non-Genetic Resistance
| Study Type | Key Findings | Quantitative Measures | Reference |
|---|---|---|---|
| Clinical Trial (mCRPC) | Adaptive therapy with abiraterone | Median TTP: ≥27 months (vs. 16.5 months SOC); 47% reduction in cumulative drug dose | [17] |
| Genomic Analysis | Tumor heterogeneity | Up to 63% of somatic mutations heterogeneous within individual tumors | [56] |
| DNA Repair Studies | Therapy-driven adaptation | 35-40% of PARPi-resistant breast/ovarian cancers show increased HRR activity; RAD51 expression 2.5x higher in platinum-resistant ovarian cancer | [56] |
| Metastatic Breast Cancer | Single-cell transcriptomics | Identification of rare drug-tolerant subpopulations (0.1-1% of tumor mass) | [9] |
| Glioblastoma Model | Temozolomide resistance | Dynamical persistence induced by treatment; not clonal selection | [54] |
Monitoring Technologies for Dynamic Resistance Assessment
Effective implementation of adaptive therapy requires sophisticated monitoring approaches to track evolving tumor composition and detect emerging resistance in real time.
Liquid Biopsy and Circulating Biomarkers
Liquid biopsies enable non-invasive, serial monitoring of tumor dynamics through blood-based biomarkers, providing critical data for adaptive therapy decision-making.
- Circulating Tumor DNA (ctDNA): Quantitative changes in ctDNA levels accurately reflect real-time tumor burden dynamics, while specific mutation patterns can identify emerging resistant subclones [52] [55].
- Protein Biomarkers: Serum markers including PSA (prostate cancer) and CA125 (ovarian cancer) provide established, cost-effective tools for tracking tumor burden changes [52].
- Circulating Tumor Cells (CTCs): Single-cell analysis of CTCs enables characterization of phenotypic plasticity and transcriptional states driving resistance [9].
Single-Cell Transcriptomics and Multi-Omics Approaches
Single-cell technologies resolve the cellular heterogeneity that underlies non-genetic resistance, capturing rare subpopulations that bulk analyses miss.
- Experimental Platforms: Droplet-based systems (10x Genomics Chromium) enable high-throughput profiling, while plate-based methods (Smart-seq2) provide superior transcript coverage [9].
- Analytical Pipelines: Dimensionality reduction (UMAP, t-SNE), clustering (Leiden), and trajectory inference (Monocle, Slingshot) reconstruct phenotypic evolution and lineage relationships during treatment [9].
- Multi-Modal Integration: Combining transcriptomic with epigenetic (ATAC-seq) and spatial data provides comprehensive views of resistance evolution [53] [9].
Experimental Protocols for Investigating Non-Genetic Resistance
Protocol: Longitudinal Single-Cell Analysis of Adaptive Therapy Response
Objective: To characterize transcriptional heterogeneity and non-genetic resistance dynamics throughout adaptive therapy cycles.
Materials:
- Patient-derived xenograft (PDX) models or 3D organoid cultures
- 10x Genomics Chromium Single Cell 3' Reagent Kit
- Validated anticancer therapeutics for adaptive cycling
- Bioanalyzer/TapeStation for quality control
- CellRanger, Seurat, and Monocle software packages
Procedure:
- Model Establishment: Implant PDX models or establish matched organoid cultures from treatment-naive tumor tissue.
- Adaptive Therapy Cycling: Administer therapeutic agents using predefined cycling rules (e.g., treat until 50% reduction in tumor volume/organoid viability, then pause until regrowth to initial size).
- Longitudinal Sampling: Collect tumor samples/organoids at critical timepoints: (T1) pretreatment baseline, (T2) initial response nadir, (T3) during regrowth phase, (T4) upon retreatment response.
- Single-Cell Preparation: Dissociate tissues to single-cell suspensions, ensuring viability >85% and minimizing stress-induced transcriptional artifacts.
- Library Preparation & Sequencing: Process 10,000 cells/sample using 10x Genomics platform, targeting 50,000 reads/cell.
- Bioinformatic Analysis:
- Process raw data with CellRanger, followed by quality control and normalization in Seurat.
- Identify cell subpopulations through shared nearest neighbor clustering.
- Reconstruct phenotypic trajectories using RNA velocity and pseudotemporal ordering with Monocle3.
- Identify differentially expressed genes and regulatory networks associated with resistance.
Expected Outcomes: Resolution of phenotypic plasticity patterns, identification of drug-tolerant persister states, and characterization of transcriptional programs driving resistance recurrence [9] [55].
Protocol: Functional Assessment of Tumor Microenvironment-Mediated Protection
Objective: To quantify the contribution of stromal components to non-genetic resistance in adaptive therapy contexts.
Materials:
- Primary cancer-associated fibroblasts (CAFs) and tumor cells
- Transwell co-culture systems
- Conditioned media collection apparatus
- Fluorescently-labeled chemotherapeutic agents
- Multiplex cytokine/chemokine arrays
Procedure:
- Stromal-Tumor Co-culture: Establish three experimental conditions: (1) tumor cells alone, (2) tumor cells + CAFs in direct contact, (3) tumor cells + CAFs in Transwell separation.
- Therapeutic Challenge: Expose all conditions to therapeutic agents using concentration gradients reflecting pharmacokinetic profiles.
- Viability Assessment: Quantify tumor cell viability through ATP-based assays at 24, 48, and 72 hours.
- Drug Penetration Measurement: Using fluorescently tagged therapeutics, measure intracellular accumulation via flow cytometry.
- Secretome Analysis: Profile CAF-derived factors in conditioned media using multiplex arrays.
- Mechanistic Validation: Employ neutralizing antibodies or small molecule inhibitors against identified protective factors to confirm functional roles.
Expected Outcomes: Quantification of stromal-mediated protection, identification of key resistance-promoting factors, and assessment of microenvironment-dependent fitness trade-offs [52] [56].
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Investigating Non-Genetic Resistance
| Reagent/Category | Specific Examples | Research Application | Key Considerations |
|---|---|---|---|
| Single-Cell Platforms | 10x Genomics Chromium, Smart-seq2 | Transcriptional heterogeneity mapping | Trade-offs between cell throughput and gene detection sensitivity |
| Lineage Tracing | Cellular barcoding, CRISPR scar-based tracing | Clonal dynamics and plasticity tracking | Enables discrimination between selection vs. induction of resistance |
| Epigenetic Profiling | ATAC-seq, ChIP-seq, methylation arrays | Mapping regulatory landscape changes | Identifies chromatin accessibility alterations underlying plasticity |
| Metabolic Probes | Seahorse XF Analyzer reagents, stable isotope tracers | Metabolic plasticity assessment | Measures real-time adaptations in energy pathways |
| TME Modeling | Organoid-stroma co-cultures, CAF-primary cells | Microenvironment-mediated resistance | Preserves native cell-cell interactions and signaling |
| Efflux Pump Assays | Fluorescent substrate accumulation (e.g., Calcein-AM) | Functional transporter activity | Quantitative measurement of multidrug resistance phenotypes |
Evolutionary Modeling and Therapeutic Strategies
Incorporating Non-Genetic Dynamics into Evolutionary Models
Mathematical models of adaptive therapy must account for non-genetic plasticity to accurately predict treatment outcomes and optimize cycling strategies.
- Extended Lotka-Volterra Frameworks: Incorporate phenotypic switching rates between drug-sensitive and tolerant states alongside competitive interactions [17].
- Game-Theoretic Approaches: Model the fitness trade-offs of resistance mechanisms, where resistance traits confer advantages during treatment but impose costs in drug-free conditions [52] [17].
- Parameter Estimation: Use longitudinal single-cell data to quantify switching rates and fitness parameters for different phenotypic states.
Therapeutic Approaches to Counter Non-Genetic Resistance
- Plasticity-Targeting Combinations: Administer agents that limit phenotypic plasticity (e.g., EMT inhibitors, epigenetic modulators) alongside primary therapeutics to stabilize tumor composition [54] [58].
- Microenvironment Modulation: Co-target stromal components (e.g., FAK inhibitors, TGF-β blockade) to disrupt protective niches and sensitize resistant populations [52] [56].
- Adaptive Dual-Drug Scheduling: Implement two-drug cycling strategies that anticipate and counteract common plasticity pathways based on evolutionary model predictions [17] [55].
Non-genetic resistance mechanisms constitute a critical vulnerability in adaptive therapy by enabling rapid, dynamic adaptation that bypasses the competitive suppression principles underlying this approach. Addressing this challenge requires integrated experimental and computational strategies that capture tumor plasticity in real time, quantify its impact on evolutionary dynamics, and develop intervention strategies that specifically target the reversibility and adaptability of these resistance programs. Through sophisticated monitoring technologies, mechanistic studies in appropriate model systems, and enhanced evolutionary models that incorporate phenotypic plasticity, the promise of adaptive therapy can be extended to malignancies where non-genetic adaptation currently drives therapeutic failure.
The fields of mathematical oncology and clinical cancer practice have historically evolved along parallel but distinct paths. Mathematical oncology uses quantitative models to understand cancer dynamics, while clinical practice focuses on direct patient care. Bridging this divide is particularly critical in the context of evolutionary modeling for cancer therapy resistance research, where the eco-evolutionary dynamics of treatment-resistant cancer populations present a fundamental barrier to lasting cure [10]. The evolution of resistance in metastatic cancers is virtually inevitable due to large, diverse cell populations, and its progression is governed by Darwinian processes that mathematical models are uniquely positioned to anticipate and steer [10].
Despite this potential, significant interdisciplinary hurdles persist. Effective collaboration requires individual specialized skills and highlights the importance of teamwork and interdisciplinary collaboration between specialists in oncology, haematology, radiotherapy, and quantitative fields [59]. This document outlines specific protocols and application notes to overcome these barriers, with particular focus on translating evolutionary dynamics research into clinically actionable strategies.
Quantitative Assessment of the Field
Bibliometric analysis reveals mathematical oncology has undergone significant evolution since the 1960s, marked by increased interdisciplinary interactions, geographical expansion, larger research teams, and greater diversity in studied topics [60]. The field is highly dynamic, with researchers incentivized to quickly adapt to both technical and medical research advances.
Table 1: Bibliometric Evolution of Mathematical Oncology
| Decade | Primary Focus Areas | Collaboration Patterns | Clinical Integration Level |
|---|---|---|---|
| 1960s-1980s | Basic growth models, population dynamics | Primarily mathematical collaborations | Limited clinical translation |
| 1990s-2000s | Angiogenesis modeling, early evolutionary models | Emerging interdisciplinary teams | Preclinical validation beginnings |
| 2010s-Present | Evolutionary dynamics, immunotherapy modeling, resistance mechanisms | Large, diverse teams including clinicians | Early clinical trials of evolution-informed therapies |
The cancer burden continues to grow, with 2,041,910 new cancer cases and 618,120 cancer deaths projected to occur in the United States in 2025 [61]. Despite overall mortality declines, the persistent challenge of therapy resistance underscores the urgent need for the interdisciplinary approaches described in these protocols.
Core Experimental Protocols
Protocol for Evolutionary Dynamics Analysis in Clinical Samples
This protocol provides a methodology for integrating mathematical modeling with clinical data to map evolutionary dynamics in cancer therapy resistance.
Materials and Reagents
- Fresh or frozen tumor tissue samples (primary and metastatic where possible)
- Single-cell RNA sequencing reagents (10x Genomics Chromium platform recommended) [9]
- Circulating tumor cell isolation materials
- DNA/RNA extraction and purification kits
- Bioinformatics pipelines for phylogenetic reconstruction
Procedure
- Sample Collection and Processing: Obtain paired tumor biopsies pre-treatment and at progression. Process samples for single-cell analysis within 24 hours of collection [9].
- Single-Cell Sequencing: Utilize droplet-based single-cell RNA sequencing (10x Genomics) to capture tumor heterogeneity. Target 5,000-10,000 cells per sample.
- Computational Analysis:
- Perform quality control using CellRanger or equivalent
- Apply dimensionality reduction (UMAP/t-SNE) and clustering (Louvain/Leiden)
- Conduct phylogenetic reconstruction using tools like Monocle3 or Slingshot
- Calculate evolutionary metrics (diversity indices, selection strength)
- Model Integration: Parameterize mathematical models of resistance evolution using quantified diversity measures and phylogenetic relationships.
- Clinical Correlation: Associate evolutionary dynamics with clinical outcomes including progression-free survival and specific resistance patterns.
Troubleshooting
- For low-quality samples: Implement whole transcriptome amplification protocols
- For computational bottlenecks: Utilize cloud-based analysis platforms
- For sparse clinical data: Implement Bayesian frameworks to handle uncertainty
Protocol for Adaptive Therapy Clinical Implementation
Adaptive therapy cycles treatment application to synchronize with patient-specific intratumoural evolutionary dynamics, suppressing proliferation of resistant cells [10].
Materials
- Standard-of-care therapeutic agents
- Frequent monitoring capabilities (imaging, liquid biopsy)
- Mathematical modeling infrastructure
- Clinical decision support system
Procedure
- Baseline Assessment: Quantify tumor burden and characterize heterogeneity through imaging and biopsy.
- Model Initialization: Parameterize evolutionary game theory models or population dynamics models with clinical data.
- Therapy Modulation:
- Administer initial therapy at standard doses until tumor response plateaus
- Reduce dose or temporarily withdraw treatment to permit sensitive cell regeneration
- Monitor frequently via PSA (prostate cancer), imaging, or liquid biopsies
- Re-escalate treatment upon significant tumor growth
- Dynamic Calibration: Continuously update model parameters based on patient response data.
- Long-term Management: Maintain tumor at stable burden through cyclical treatment modulation.
Validation Metrics
- Time to progression compared to historical controls
- Quality of life measures
- Overall survival
- Cost-effectiveness analysis
Visualizing Interdisciplinary Workflows
Mathematical-Clinical Collaboration Framework
Diagram 1: Collaboration Framework for Mathematical and Clinical Oncology Integration
Evolutionary Therapy Decision Pathway
Diagram 2: Evolutionary Therapy Clinical Decision Pathway
Research Reagent Solutions
Table 2: Essential Research Reagents for Evolutionary Therapy Resistance Studies
| Reagent/Category | Specific Examples | Research Application | Clinical Translation Utility |
|---|---|---|---|
| Single-Cell RNA Sequencing Platforms | 10x Genomics Chromium, Smart-seq2 [9] | Mapping tumor heterogeneity, identifying rare resistant subpopulations | Biomarker discovery, therapy selection guidance |
| Circulating Tumor Cell Isolation | Microfluidic devices, immunomagnetic separation | Monitoring evolutionary dynamics non-invasively | Treatment response monitoring, early resistance detection |
| Spatial Transcriptomics | 10x Visium, Slide-seq [9] | Characterizing tumor microenvironment spatial structure | Understanding niche-specific resistance mechanisms |
| Evolutionary Barcoding | CRISPR-based lineage tracing | Quantifying clonal dynamics in experimental models | Validating evolutionary model predictions |
| Mathematical Modeling Software | Python with SciPy, R with deSolve packages | Implementing evolutionary dynamics simulations | Personalized therapy forecasting |
| Immune Profiling Tools | Multiplex immunofluorescence, mass cytometry | Characterizing tumor-immune interactions | Immunotherapy resistance assessment |
Implementation Hurdles and Solutions
Communication and Conceptual Barriers
The fundamental challenge in bridging mathematical oncology and clinical practice lies in conceptual translation between quantitative and medical frameworks. Where mathematicians express concepts through equations and statistical projections, clinicians require actionable, patient-specific recommendations.
Solution Strategies:
- Establish cross-disciplinary glossaries with explicit definitions
- Create visual abstraction frameworks that represent mathematical concepts in clinically intuitive formats
- Develop joint training opportunities including clinical rotations for mathematical oncologists and quantitative training for clinicians
- Implement regular case conferences where models are presented alongside patient cases
Data Integration Challenges
Clinical data often exists in fragmented systems with varying quality, while mathematical models require structured, high-quality input data. Single-cell transcriptomics has emerged as a transformative approach, enabling high-resolution analysis of individual cells to reveal tumor composition, lineage dynamics, and transcriptional plasticity [9]. However, technical challenges include low RNA capture efficiency and tumor dissociation biases.
Solution Strategies:
- Develop standardized data pipelines for clinical-to-model data transformation
- Create FAIR (Findable, Accessible, Interoperable, Reusable) data principles for interdisciplinary cancer research
- Implement middleware solutions that can interface with electronic health record systems
- Establish biobanking protocols that preserve material for single-cell analysis
Validation and Evidence Generation
Mathematical models require rigorous validation, but traditional clinical trial designs may be inadequate for evaluating dynamic, adaptive treatment strategies informed by evolutionary principles.
Solution Strategies:
- Develop hybrid trial designs incorporating model validation endpoints
- Create digital twin frameworks for in silico testing of therapeutic strategies
- Establish multi-site validation consortia to ensure model generalizability
- Implement iterative co-validation processes between model predictions and clinical outcomes
The integration of mathematical oncology and clinical practice represents a paradigm shift in cancer therapy resistance research. Emerging areas include:
- Artificial Intelligence Integration: Combining evolutionary models with deep learning for improved prediction of resistance pathways.
- Spatio-temporal Modeling: Incorporating single-cell transcriptomics with spatial resolution to map metastatic evolution [9].
- Immuno-evolutionary Dynamics: Modeling the co-evolution of tumors and immune responses under therapeutic pressure.
- Precision Adaptive Therapy: Developing patient-specific evolutionary models to guide dynamic treatment modulation.
As the field evolves, interdisciplinary collaboration remains the cornerstone of progress. The protocols and frameworks outlined here provide a roadmap for bridging mathematical oncology and clinical practice to address the fundamental challenge of therapy resistance. Through continued investment in collaborative infrastructure, training, and research, we can realize the potential of evolutionary modeling to transform cancer care and outcomes.
Success will require sustained commitment to overcoming interdisciplinary hurdles, but the potential payoff—transforming cancer from a lethal to a manageable chronic disease—justifies the substantial effort required.
The emergence of therapy resistance represents the primary cause of treatment failure in advanced cancers. Traditional maximum tolerated dose (MTD) strategies, while achieving initial tumor reduction, inadvertently accelerate the evolution and proliferation of resistant cell populations through competitive release. This application note synthesizes current evolutionary modeling approaches and provides detailed protocols for implementing evolution-informed treatment strategies that control tumor burden by constraining, rather than unleashing, evolutionary speed. We focus on quantitative frameworks, experimental methodologies, and computational tools that enable researchers to design therapies that explicitly manage the tempo of cancer evolution to prolong disease control.
Cancer ecosystems exhibit remarkable adaptability to therapeutic perturbations. The conventional paradigm of maximizing cell kill through MTD approaches suffers from a critical evolutionary flaw: by eliminating treatment-sensitive populations, it removes competition for resistant phenotypes, thereby accelerating their expansion—a phenomenon known as competitive release [62] [1]. This dynamic is particularly problematic in metastatic settings where complete eradication is unlikely, and tumor recurrence is virtually inevitable.
The cost of resistance creates a critical therapeutic leverage point. Resistant cells typically divert energy resources to maintain molecular defense mechanisms (e.g., drug efflux pumps, enhanced DNA repair), reducing their proliferative capacity in drug-free environments [63] [62]. Evolutionary-based therapies exploit this trade-off by maintaining stable populations of treatment-sensitive cells that can outcompete resistant variants in the absence of continuous drug pressure. The subsequent sections provide implementable frameworks for quantifying these dynamics and translating them into controlled therapeutic protocols.
Quantitative Foundations: Modeling Evolutionary Dynamics
Key Parameters for Evolutionary Tracking
Table 1: Core Quantitative Parameters for Monitoring Evolutionary Dynamics
| Parameter | Biological Significance | Measurement Method | Typical Range |
|---|---|---|---|
| Net proliferative rate (λ) | Growth rate of cell population under specific conditions | Linear regression of log-transformed cell counts over time [64] | -0.5 to 0.9 day⁻¹ |
| Resistance cost (C) | Fitness reduction of resistant phenotype in drug-free environment | Competitive co-culture assays [63] | 0.05-0.5 (relative to sensitive) |
| Initial resistant fraction (f₀) | Pre-existing resistant cells prior to therapy | Deep sequencing or drug challenge assays [64] | 10⁻⁶ to 10⁻³ |
| Drug concentration threshold (β) | Minimum concentration for efficacy | Dose-response curves [65] | Variable by agent |
| Cumulative drug toxicity (x₃) | Total drug exposure burden | Pharmacokinetic integration [65] | Patient-specific |
Mathematical Framework for Population Dynamics
The evolutionary dynamics of sensitive (S) and resistant (R) cell populations under drug exposure can be modeled using a binary nonhomogeneous birth-death process [64]:
Mean population dynamics after m therapy cycles with cycle time (t₁ + t₂):
Where λ(c) and μ(c) represent net proliferation rates under different drug concentrations, and s₀ and r₀ are initial population sizes [64].
The fitness cost of resistance can be quantified through proliferative potential measurements, where sensitive populations may exhibit proliferative potential of 1.0 (replicating each generation) while resistant variants may demonstrate reduced potential of 0.05 (replicating once every 20 generations) in absence of therapeutic selection pressure [63].
Experimental Protocols: Quantifying Evolutionary Parameters
Protocol 1: Measuring Net Proliferative Rates Under Drug Exposure
Purpose: Quantify population growth dynamics of sensitive and resistant cells across a range of drug concentrations to parameterize evolutionary models.
Materials:
- Isogenic cell lines with differential drug sensitivity (e.g., HCC827 [sensitive] and H1975 [resistant] for EGFR-TKI studies) [64]
- Therapeutic agents of interest (e.g., erlotinib, paclitaxel)
- Automated cell counting system or microscopy platform
- 96-well or 6-well tissue culture plates
Procedure:
- Seed triplicate wells at 5,000 cells/well in appropriate growth medium
- After 24-hour attachment, apply drug concentrations across a 6-log range (0.1 nM to 100 μM)
- Perform cell counts every 24 hours for 5-7 days using automated counting or live-cell imaging
- Log-transform cell count data and perform linear regression against time
- Calculate net proliferative rate (λ) as the slope of the regression line
- Fit concentration-response curves using nonlinear least-squares regression
- Validate model fit by comparing predicted vs. observed population sizes
Data Analysis: Net proliferative rates should be calculated for each drug concentration using the formula: λ = ln(N₂/N₁)/(t₂-t₁), where N represents cell count at time t [64].
Protocol 2: Competitive Co-culture to Quantify Resistance Costs
Purpose: Measure the fitness disadvantage of resistant phenotypes in drug-free environments when competing with sensitive cells.
Materials:
- Fluorescently tagged sensitive and resistant cell lines (e.g., GFP/RFP labels)
- Flow cytometry system
- Drug-free culture medium
Procedure:
- Mix sensitive and resistant cells at defined ratios (e.g., 1:1, 1:10, 10:1)
- Culture in drug-free medium for 14-21 days, passaging when near confluence
- Sample populations every 3-4 days and analyze by flow cytometry to determine ratios
- Calculate relative fitness using the formula: w = ln(R₂/R₁)/ln(S₂/S₁) where R and S represent resistant and sensitive population sizes
- Repeat under varying nutrient conditions to assess environmental modulation of resistance costs
Data Analysis: The resistance cost (C) is calculated as C = 1 - w, where w is the relative fitness of resistant compared to sensitive cells [63] [62].
Computational Implementation: Evolutionary Treatment Optimization
Adaptive Therapy Protocol Design
Objective: Maintain tumor burden at stable levels using minimum necessary drug pressure to preserve sensitive cells that suppress resistant expansion.
Algorithm:
- Establish baseline tumor size (e.g., circulating tumor DNA, imaging metrics)
- Initiate therapy at standard doses until tumor reduction ≥50%
- Monitor tumor burden at regular intervals (2-4 weeks)
- Apply therapeutic pulses only when tumor growth exceeds a predetermined threshold (e.g., 20-50% increase from nadir)
- Adjust dose and timing to maintain stable tumor volume
- Incorporate drug-free holidays to allow sensitive cell recovery
Implementation Considerations: Treatment response should be monitored through multiple modalities including radiographic assessment, circulating tumor DNA (ctDNA) analysis, and traditional tumor markers [62] [66].
Double-Bind Therapy Scheduling
Rationale: Simultaneously target vulnerable phenotypes in both tumor core and periphery through strategically sequenced agents.
Protocol:
- Phase 1 (Glucose competitor): Administer glycolytic inhibitor (e.g., 2-deoxyglucose) to target hypoxic, chemoresistant core populations
- Phase 2 (Cytotoxic agent): Apply chemotherapy in separate pulses to target proliferative rim populations
- Optimal scheduling: Separate glucose competitor and chemotherapy administration rather than concurrent delivery [63]
Quantitative Framework: In avascular tumor models (2mm diameter), sensitive populations typically exhibit proliferative potential of 1.0 with IC₅₀ of 10 nM·h, while resistant populations show proliferative potential of 0.05 with IC₅₀ of 1 μM·h [63].
Table 2: Evolutionary-Informed Treatment Strategies and Their Applications
| Strategy | Mechanism | Key Parameters | Tumor Context |
|---|---|---|---|
| Adaptive Therapy [62] | Maintains sensitive competitors | Treatment threshold: 20-50% growth from nadir; Dose: Minimum to stabilize | Hormone-sensitive cancers, Metastatic melanoma |
| Double-Bind Therapy [63] | Targets complementary vulnerabilities | Sequencing: Glucose competitor → Chemotherapy; Dose separation: 24-48h | Glycolytic tumors, Hypoxic microenvironments |
| Sequential Pulsing [64] | Prevents adaptation to single agent | Cycle: 7-21 days per drug; Rotation: Non-cross-resistant agents | NSCLC with T790M resistance |
| Metronomic Dosing [1] | Continuous low-pressure inhibition | Frequency: Daily-low dose; Duration: Continuous until progression | Angiogenic tumors, Pediatric malignancies |
Visualization: Evolutionary Therapy Workflows
Evolutionary Therapy Decision Pathway: Contrasting traditional MTD approaches with evolution-informed adaptive strategies that maintain stable tumor burden through dynamic treatment modulation.
Double-Bind Therapeutic Strategy: Sequential targeting of spatially distinct tumor subpopulations through metabolic and cytotoxic agents to impose conflicting selection pressures.
The Scientist's Toolkit: Essential Research Reagents
Table 3: Key Research Reagents for Evolutionary Therapy Investigations
| Reagent/Cell Line | Application | Key Features | Experimental Use |
|---|---|---|---|
| HCC827 cells [64] | EGFR-TKI sensitivity studies | EGFR exon 19 deletion (E746-A750) | Sensitive population model for erlotinib studies |
| H1975 cells [64] | TKI resistance modeling | L858R + T790M mutations | Resistant population model with gatekeeper mutation |
| 2-Deoxyglucose [63] | Glycolytic inhibition | Glucose analog, competitive inhibitor | Targeting hypoxic tumor core populations |
| Erlotinib [64] | EGFR pathway inhibition | Tyrosine kinase inhibitor, reversible | Selective pressure modulation in NSCLC models |
| Paclitaxel [64] | Microtubule stabilization | Cytotoxic antimitotic agent | Combination therapy with targeted agents |
| Fluorescent cell tags (GFP/RFP) [63] | Competitive co-culture | Stable expression, non-interfering | Tracking population dynamics in mixed cultures |
Evolutionary principles provide a powerful framework for reimagining cancer therapy beyond maximum cell kill. The protocols and models presented here enable researchers to design treatment strategies that explicitly manage evolutionary speed by maintaining sensitive cell populations that suppress resistant variants through competition. By shifting the therapeutic goal from eradication to stable control, these approaches exploit inherent evolutionary trade-offs—particularly the fitness costs of resistance mechanisms—to prolong treatment efficacy. Implementation requires sophisticated monitoring, dynamic dosing, and combinatorial strategies that create evolutionary double binds where any adaptive path carries substantial fitness disadvantages. As cancer research increasingly recognizes evolution as the proximate cause of treatment failure, these evolution-informed protocols offer a promising path toward transforming advanced cancers into chronically managed conditions.
Evolutionary Cancer Therapy (ECT) represents a paradigm shift in the treatment of metastatic cancers, moving from a "treat to eradicate" approach to a "treat to contain" or "treat to delay progression" strategy [67] [68]. By applying principles from evolutionary biology and game theory, ECT aims to control tumor burden by exploiting the evolutionary dynamics between drug-sensitive and drug-resistant cancer cell populations [67] [1]. Despite promising clinical results—including a trial for metastatic castrate-resistant prostate cancer (mCRPC) that extended median time to progression from approximately 14.3 to 33.5 months compared to standard of care—the clinical implementation of ECT faces significant practical challenges [67] [24]. These barriers include the need for multidisciplinary collaboration, complex mathematical modeling, frequent disease monitoring, and adaptive treatment protocols that depart from conventional clinical workflows [67]. This application note addresses these implementation challenges by providing a structured framework for integrating ECT into clinical practice, with specific protocols for resource allocation, workflow design, and therapeutic decision-making.
Core Principles and Quantitative Evidence Base
Evolutionary therapy strategies are founded on the observation that resistant cancer cells often bear a fitness cost in the absence of therapy [1] [62]. Conventional Maximum Tolerable Dose (MTD) chemotherapy eliminates drug-sensitive cells, removing competition for resources and allowing resistant populations to expand freely—a phenomenon known as "competitive release" [1] [62]. In contrast, ECT maintains a stable population of sensitive cells that can suppress the growth of resistant clones through competition for space and resources [67] [45].
Clinical trials have demonstrated the feasibility of this approach across multiple cancer types. The foundational trial for mCRPC (NCT02415621) established a protocol where treatment was paused once prostate-specific antigen (PSA) levels decreased by 50% and resumed only when PSA returned to baseline levels [67] [68]. This adaptive cycling approach reduced cumulative drug dose to 47% of standard dosing while significantly extending time to progression [67]. Building on this success, ongoing clinical trials are investigating ECT protocols for ovarian cancer (NCT05080556), BRAF-mutant melanoma (NCT03543969), and other malignancies [67].
Table 1: Clinical Trial Evidence for Evolutionary Therapy Approaches
| Cancer Type | Trial Identifier | Therapeutic Protocol | Reported Outcomes |
|---|---|---|---|
| Metastatic Castrate-Resistant Prostate Cancer | NCT02415621 | Abiraterone dose cycling based on PSA levels (treatment paused at 50% PSA reduction, resumed at baseline) | Median time to progression: 33.5 months (vs. 14.3 months with standard care); 47% cumulative drug reduction [67] |
| Ovarian Cancer | NCT05080556 | Dose titration based on tumor response (dose gradually decreased when tumor burden is decreasing) | Ongoing trial; results expected forthcoming [67] [68] |
| Various Advanced Cancers | NCT04343365 | Evolutionary Tumor Board feasibility study for incurable patients | Ongoing trial; multidisciplinary team suggests evolutionary treatment strategies [67] |
The theoretical underpinnings of ECT are formalized through mathematical frameworks, particularly evolutionary game theory and Stackelberg evolutionary games [67] [68]. In these models, the physician acts as a "leader" who chooses treatment doses to maximize patient quality of life, while cancer cells act as "followers" that evolve resistance traits in response to treatment pressures [68]. This conceptual framework enables the development of treatment strategies that anticipate and steer the eco-evolutionary dynamics of tumor populations.
Table 2: Mathematical Modeling Approaches in Evolutionary Therapy
| Model Type | Key Features | Clinical Applications |
|---|---|---|
| Stackelberg Evolutionary Game | Physician as "leader" and cancer cells as "followers"; treatment optimized to maximize patient quality of life while anticipating evolutionary response [68] | Identifies optimal constant treatment doses for tumor stabilization; predicts superior outcomes compared to MTD [68] |
| Evolutionary Game Theory with Frequency-Dependent Selection | Models competitive interactions between sensitive and resistant cell populations; accounts for fitness costs of resistance [69] [45] | Informs adaptive therapy protocols that maintain sensitive cells to suppress resistant growth; basis for mCRPC clinical trial design [45] |
| Optimal Control Theory | Mathematical framework for identifying dose titration protocols that stabilize tumor volume [45] | Suggests increasing dose titration may achieve tumor stabilization across diverse initial tumor compositions [45] |
Integrated Clinical Workflow Implementation
Successful ECT implementation requires reengineering conventional oncology workflows to incorporate dynamic monitoring, mathematical modeling, and adaptive decision-making. The following workflow provides a structured approach for clinical integration.
Diagram 1: ECT Clinical Workflow
Resource Requirements and Allocation
Implementing ECT requires specific expertise and infrastructure that may not be present in conventional oncology practices:
Multidisciplinary Team: Successful ECT implementation requires a dedicated team including oncologists, mathematical modelers, computational biologists, and data scientists [67]. The Moffitt Cancer Center model, with its Integrated Mathematical Oncology department, serves as a prototype for this collaborative structure [67].
Monitoring Resources: ECT demands more frequent biomarker assessment than standard care. For prostate cancer, this involves PSA testing every 3-4 weeks instead of the conventional 3-month intervals [67]. For other cancers, this may require advanced imaging or liquid biopsy protocols that necessitate coordination with radiology and pathology departments.
Computational Infrastructure: ECT relies on mathematical models for treatment decision support. Clinical centers need access to computational resources for model calibration, simulation, and prediction. Cloud-based solutions can make this accessible without extensive local infrastructure [67].
Protocol for Adaptive Therapy in mCRPC
The following protocol provides a detailed template for implementing ECT in metastatic castrate-resistant prostate cancer, based on the validated approach from NCT02415621:
Objective: To prolong time to progression and maintain quality of life through adaptive administration of abiraterone in mCRPC patients.
Inclusion Criteria:
- Histologically confirmed metastatic prostate cancer
- Castrate-resistant disease (testosterone < 50 ng/dL)
- Rising PSA despite androgen deprivation therapy
- No prior abiraterone treatment
- ECOG performance status 0-2
Treatment Protocol:
- Initial Phase: Begin abiraterone at 1000 mg daily with prednisone 5 mg twice daily
- Monitoring: Assess PSA levels every 3-4 weeks
- Treatment Decision Algorithm:
- CONTINUE treatment if PSA is below 50% of baseline
- PAUSE treatment if PSA reaches ≤50% of baseline value
- RESTART treatment when PSA returns to baseline level
- Dose Modification: For PSA progression during treatment phases, consider dose escalation if tolerated; for toxicities, follow standard dose reduction guidelines
Assessment Schedule:
- Clinical evaluation every 4-6 weeks
- Comprehensive metabolic panel every 4 weeks
- CT imaging every 12 weeks
- Quality of life assessment every 8 weeks
Endpoint Evaluation:
- Primary endpoint: Time to progression (PSA progression, radiographic progression, or clinical deterioration)
- Secondary endpoints: Cumulative drug dose, quality of life metrics, overall survival
Therapeutic Decision-Making Framework
ECT requires a dynamic decision-making process that responds to tumor dynamics. The following diagram illustrates the treatment adaptation logic for maintaining tumor control while minimizing resistance.
Diagram 2: ECT Decision Logic
Essential Research Reagents and Computational Tools
Implementing ECT in both research and clinical settings requires specific reagents, assays, and computational resources. The following table details essential components of the "evolutionary therapy toolkit."
Table 3: Research Reagent Solutions for Evolutionary Therapy Development
| Reagent/Tool Category | Specific Examples | Research Application |
|---|---|---|
| Biomarker Assays | PSA tests, ctDNA detection panels, circulating tumor cell isolation | Frequent monitoring of tumor burden and composition; essential for treatment adaptation decisions [67] |
| Mathematical Modeling Platforms | Ordinary Differential Equation (ODE) models, Partial Differential Equation (PDE) models, Agent-Based Models (ABMs) | Prediction of tumor dynamics under different treatment scenarios; treatment protocol optimization [67] [68] |
| Game Theory Frameworks | Stackelberg evolutionary game models, Frequency-dependent selection models | Formalization of physician-cancer interactions; identification of evolutionarily robust treatment strategies [67] [68] |
| Cell Line Models | Sensitive and resistant isogenic cell pairs, 3D co-culture systems | Experimental validation of competitive interactions between cell populations; assessment of resistance costs [69] |
Implementation Protocol for Dose Titration Therapy
For cancer types where cycling therapy may not be optimal, dose titration provides an alternative ECT approach. The following protocol is adapted from the NCT05080556 ovarian cancer trial:
Objective: To achieve stable tumor control through gradual dose adjustments based on tumor response dynamics.
Treatment Algorithm:
- Initial Phase: Begin treatment at standard MTD until tumor burden decreases by ≥30%
- Titration Phase: Reduce dose by 25% for each subsequent cycle while tumor burden continues to decrease
- Maintenance Phase: Once minimal effective dose is identified, continue with regular monitoring
- Adaptation Phase:
- For tumor burden increase <20% above nadir: maintain current dose with increased monitoring frequency
- For tumor burden increase ≥20% above nadir: increase dose by 25-50% until control is reestablished
Monitoring Requirements:
- Tumor burden assessment every 4-6 weeks via appropriate modality (imaging, biomarkers)
- Toxicity assessment every treatment cycle
- Quality of life metrics every 8 weeks
The clinical integration of Evolutionary Cancer Therapy requires significant workflow modifications and specialized resources but offers a promising approach for extending progression-free survival in metastatic cancers. By adopting the structured frameworks, protocols, and decision algorithms presented in this application note, cancer centers can systematically implement ECT strategies that leverage evolutionary dynamics to improve patient outcomes. The ongoing clinical trials across multiple cancer types will provide further evidence to refine these protocols and expand the application of evolutionary principles in clinical oncology.
Evidence and Efficacy: Preclinical Validation and Clinical Trial Outcomes
The emergence of therapy resistance represents the primary cause of treatment failure in advanced cancers, a process fundamentally governed by evolutionary dynamics within large cell populations [1] [70]. Overcoming this challenge requires model systems that accurately recapitulate the complex, multi-scale interactions between genetic heterogeneity, phenotypic plasticity, and microenvironmental selection pressures [71] [72]. This Application Note provides detailed protocols for implementing key in vivo and in vitro models that capture these evolutionary dynamics, enabling researchers to dissect resistance mechanisms and design evolution-informed therapeutic strategies. We focus particularly on integrating quantitative measurements of clonal dynamics with microenvironmental manipulation, providing a bridge between traditional oncology models and emerging evolutionary paradigms.
Key In Vitro Model Systems
3D Tumor Organoids for Evolutionary Studies
Application Note: Tumor organoids preserve the genetic heterogeneity and phenotypic plasticity of parental tumors while enabling controlled experimental manipulation, making them ideal for studying evolutionary dynamics in large populations [73].
Detailed Protocol: Establishing Patient-Derived Tumor Organoids
Sampling and Tissue Processing:
- Obtain tumor tissue via surgical resection or biopsy (1-3 mm³ pieces). Non-surgical sources include malignant effusions, ascites, or circulating tumor cells from blood [73].
- Using sterile technique, remove non-epithelial tissue (muscle, fat) with tweezers and surgical scissors.
- Digest tissue pieces with collagenase/hyaluronidase and TrypLE Express enzymes with continuous agitation (2 hours at 37°C or overnight on shaker). For overnight digestion, add 10 µM ROCK inhibitor (Y-27632) to enhance viability.
- Monitor digestion progress; completion is indicated when visible clusters of 2-10 cells appear. Terminate digestion when gentle pipetting yields predominantly single cells and small clusters.
Cell Preparation and Plating:
- Filter cell suspension through 70-100 µm strainers based on tumor type to remove undigested fragments.
- Centrifuge filtered cells (300-500 × g for 5 minutes) and resuspend in appropriate organoid medium.
- Mix cell suspension with extracellular matrix (ECM) hydrogel (Matrigel, BME, or Geltrex) at a ratio determined by cell density and experimental requirements.
- Plate 10-20 µL drops of cell-ECM suspension into pre-warmed multi-well plates. Invert plates and incubate at 37°C, 5% CO₂ for 15-30 minutes to allow ECM polymerization.
- After solidification, carefully add pre-warmed organoid culture medium to each well.
Passaging and Expansion:
- For passaging, remove medium and dissociate organoids using mechanical disruption (pipetting) and enzymatic digestion.
- Replate cells in fresh ECM at appropriate splitting ratios (typically 1:3 to 1:8 depending on growth rate).
- Cryopreserve organoids in freezing medium containing 10% DMSO and specific organoid medium for long-term storage.
Table 1: Comparative Analysis of Model Systems for Evolutionary Studies
| Model System | Key Applications in Evolutionary Dynamics | Tumor Heterogeneity Preservation | Throughput | Technical Complexity | Timeline for Experiments |
|---|---|---|---|---|---|
| 3D Tumor Organoids | Clonal competition, microenvironmental selection, therapy resistance evolution [73] | High (maintains parental tumor diversity) | Medium | High | 2-8 weeks |
| Genetic Barcoding | Quantifying phenotype dynamics, lineage tracing, resistance emergence timing [74] | Can be introduced into any cell model | Medium-High | High | 4-20 weeks |
| Syngeneic Mouse Models | Tumor-immune coevolution, immunotherapeutic resistance [72] [75] | Medium (defined cell line) | Medium | Medium | 4-12 weeks |
| Patient-Derived Xenografts | Human-specific evolutionary dynamics, personalized therapy testing [73] | High (maintains patient-specific heterogeneity) | Low | High | 3-9 months |
Genetic Barcoding for Lineage Tracing
Application Note: Genetic barcoding enables quantitative measurement of phenotype dynamics and clonal trajectories during resistance evolution, distinguishing between pre-existing resistance and adaptive emergence [74].
Detailed Protocol: Experimental Evolution with Barcoded Cell Populations
Barcode Library Design and Cell Preparation:
- Design a complex lentiviral barcode library containing >10,000 unique sequences to ensure sufficient diversity for tracking large populations.
- Transduce target cell population (e.g., colorectal cancer lines SW620, HCT116) at low MOI (<0.3) to ensure most cells receive a single unique barcode.
- Culture transduced cells for 2-3 weeks under appropriate selection (e.g., puromycin) to establish a stable barcoded pool.
- Expand barcoded population to create a master cell bank with known diversity; aliquot and cryopreserve for consistent experimental starting material.
Experimental Evolution and Drug Treatment:
- Thaw barcoded cells and expand to desired population size (typically 10-100 million cells) in drug-free medium.
- Split expanded population into replicate subpopulations (3-4 technical replicates recommended) for parallel evolution under identical conditions.
- Apply periodic drug treatment cycles mirroring clinical regimens (e.g., 5-FU for colorectal models): 3-5 days treatment followed by 7-10 days recovery in drug-free medium.
- Maintain populations for multiple treatment cycles (typically 4-8 cycles) to observe evolutionary dynamics.
- Passage cells using standardized sampling bottlenecks (e.g., 100,000-500,000 cells per passage) to maintain logarithmic growth while tracking population bottlenecks.
Barcode Sequencing and Analysis:
- At each sampling timepoint, extract genomic DNA from ≥1×10⁶ cells using commercial kits.
- Amplify barcode regions using PCR with primers containing Illumina adapter sequences and unique dual indices.
- Sequence amplified libraries on Illumina platform (MiSeq or NextSeq) to achieve >100x coverage of estimated barcode diversity.
- Process raw sequencing data: demultiplex samples, align sequences to barcode reference library, and quantify barcode abundances.
- Apply mathematical framework to infer phenotype dynamics from barcode frequency changes [74].
Diagram 1: Genetic barcoding identifies phenotype switching paths. The workflow (top) shows experimental steps from library creation to data analysis. The inferred dynamics (bottom) illustrate transitions between phenotypic states: from sensitive to resistant (μ), resistant back to sensitive (σ), and from resistant to escape (α·f(D(t))) which is drug concentration-dependent [74].
Key In Vivo Model Systems
Syngeneic Models for Tumor-Immune Coevolution
Application Note: Syngeneic mouse models enable study of evolutionary dynamics within intact immune environments, particularly valuable for investigating immunotherapy resistance mechanisms [72] [75].
Detailed Protocol: Analyzing Myeloid-Mediated Resistance in Syngeneic Models
Model Establishment and Validation:
- Select appropriate syngeneic pair: MyC-CaP prostate cancer cells in C57BL/6 mice for prostate cancer studies [75], E0771 breast cancer cells in C57BL/6 mice for breast cancer.
- Culture tumor cells in appropriate medium, ensuring mycoplasma-free status and maintaining passage number <20 post-revival.
- Harvest cells in logarithmic growth phase, resuspend in PBS at 1-5×10⁶ cells/100µL for subcutaneous injection or 2.5×10⁵ cells/50µL for orthotopic implantation.
- Monitor tumor growth 3 times weekly by caliper measurements; randomize mice into treatment groups when tumors reach 100-150 mm³.
Therapeutic Intervention and Monitoring:
- For immunotherapy resistance studies: Administer anti-PD-1/PD-L1 antibodies (200µg per mouse, intraperitoneally, every 3-4 days for 3 cycles).
- For targeting myeloid-mediated resistance: Combine ICIs with A2AR inhibitors (e.g., ciforadenant, 25mg/kg, orally daily) [75].
- Monitor tumor volume and mouse body weight throughout study; define progression as ≥20% weight loss or tumor volume exceeding 1500 mm³.
Endpoint Analysis of Evolutionary Dynamics:
- Harvest tumors at endpoint (day 21-28 post-treatment initiation or when reaching ethical endpoints).
- Process tissue for single-cell RNA sequencing: create single-cell suspension using tumor dissociation kit, count viable cells, target 5,000-10,000 cells per sample for 10x Genomics platform.
- For flow cytometry: stain single-cell suspensions with antibodies against CD45, CD11b, F4/80, SPP1 to identify SPP1hi-TAM populations [75].
- Analyze T-cell exhaustion markers (PD-1, TIM-3, LAG-3) on CD8+ T cells to correlate with myeloid population changes.
Table 2: Research Reagent Solutions for Evolutionary Dynamics Studies
| Research Reagent | Specific Function | Application Notes | Key Evolutionary Insight |
|---|---|---|---|
| Extracellular Matrix Hydrogels (Matrigel, BME) | Provides 3D scaffold mimicking basement membrane | Optimal concentration varies by tumor type (typically 50-70%); keep liquid at 4°C during handling | Maintains tumor architecture enabling realistic cell-cell competition [73] |
| Lentiviral Barcode Libraries | Unique sequence tags for lineage tracing | Ensure library complexity >10,000 barcodes; use low MOI for single barcode per cell | Quantifies clonal dynamics and phenotype switching rates [74] |
| ROCK Inhibitor (Y-27632) | Enhances survival of stem/progenitor cells | Use at 10µM during initial plating and passaging; not required in established cultures | Preserves cellular diversity by reducing anoikis in vulnerable subpopulations [73] |
| A2AR Inhibitors (e.g., Ciforadenant) | Blocks adenosine-mediated immunosuppression | Administer at 25mg/kg daily orally in preclinical models; currently in clinical trials | Reverses SPP1hi-TAM-mediated T-cell suppression [75] |
| Anti-CSF1R Antibodies | Depletes specific macrophage populations | Limited efficacy against SPP1hi-TAMs due to low CSF1R expression [75] | Demonstrates subset-specific resistance mechanisms in tumor microenvironment |
Integrating Microenvironmental Pressures in Evolutionary Models
Application Note: The tumor microenvironment creates selective pressures that shape resistance evolution through multiple mechanisms including hypoxia, immune editing, and stromal interactions [71] [72].
Detailed Protocol: Modeling Hypoxia-Driven Angiogenesis and Resistance
Hypoxia Chamber Setup:
- Place organoid cultures or tumor spheroids in modular incubator chambers.
- Flush chambers with certified gas mixture containing 1% O₂, 5% CO₂, and balance N₂ for 10-15 minutes.
- Seal chambers and place in standard tissue culture incubator at 37°C for desired duration (typically 24-72 hours).
- For chronic hypoxia studies, maintain cultures in specialized hypoxia workstations at consistent low oxygen tensions (0.1-2% O₂).
Assessment of Hypoxia-Mediated Evolutionary Changes:
- Quantify HIF-1α stabilization via Western blot or immunofluorescence after hypoxia exposure.
- Measure transcript levels of hypoxia-responsive genes (VEGF, CA9, SLC2A1) by qRT-PCR.
- Profile endothelial cell chemotaxis in response to hypoxic tumor secretome using transwell migration assays.
- Analyze heterogeneous drug distribution in hypoxic vs normoxic regions using fluorescent drug analogs and confocal microscopy.
Diagram 2: Tumor microenvironment creates multidirectional selection. Microenvironmental pressures (red) induce molecular and cellular adaptations (yellow) that drive processes (green) leading to clonal expansion of resistant populations. HIF-1α: hypoxia-inducible factor 1-alpha; VEGF: vascular endothelial growth factor; PgP: P-glycoprotein; EMT: epithelial-to-mesenchymal transition; TAM: tumor-associated macrophage [71] [1] [72].
The model systems described herein provide a comprehensive toolkit for capturing the evolutionary dynamics of therapy resistance in cancer. The integration of 3D organoid cultures with genetic barcoding enables unprecedented resolution in tracking clonal dynamics, while sophisticated syngeneic and xenograft models reveal the critical role of tumor-immune coevolution in treatment failure. By implementing these protocols with attention to the quantitative analysis of population dynamics, researchers can bridge the gap between evolutionary theory and therapeutic innovation, ultimately contributing to more effective strategies for managing cancer as an evolutionary process.
The relentless evolution of therapy resistance remains a fundamental barrier to achieving durable remissions in advanced cancers. The standard-of-care paradigm of administering maximum tolerated dose (MTD) chemotherapy inevitably applies potent selection pressure, favoring the outgrowth of resistant cell clones and leading to treatment failure. Evolutionary cancer therapy (ECT) represents a transformative alternative that explicitly acknowledges and exploits the evolutionary dynamics within tumors. By strategically modulating treatment timing and dosing based on individual tumor response, ECT aims to suppress resistant populations by maintaining a pool of therapy-sensitive cells that can competitively inhibit their growth. This application note synthesizes the latest clinical trial data and experimental protocols for three major malignancies—metastatic castration-resistant prostate cancer (mCRPC), melanoma, and ovarian cancer—framed within the critical context of evolutionary modeling for cancer therapy resistance research.
Quantitative Clinical Trial Landscape
Table 1: Key Recent Clinical Trials in mCRPC, Melanoma, and Ovarian Cancer
| Cancer Type | Trial Name / Identifier | Phase | Intervention | Key Efficacy Findings | Evolutionary Rationale |
|---|---|---|---|---|---|
| Prostate (mCRPC) | PROpel [76] | III | Olaparib + Abiraterone vs Abiraterone | rPFS: 25.0 vs 16.4 months (HR 0.66) | Vertical combination to preempt resistance via dual pathway targeting (AR + DNA repair) |
| Prostate (mCRPC) | TALAPRO-2 [76] | III | Talazoparib + Enzalutamide vs Enzalutamide | rPFS benefit (data immature) | Synthetic lethality in HRR-deficient subpopulations within tumor ecosystem |
| Prostate (mCRPC) | ANZadapt (NCT05393791) [2] | II | Adaptive Abiraterone / Docetaxel | Ongoing | Direct testing of evolutionary principles: dose modulation based on PSA |
| Melanoma | PRISM-MEL-301 (NCT06112314) [77] | III | Brenetafusp + Nivolumab vs Nivolumab | Phase 1/2: 35% ORR in ICI-pretreated [77] | Bispecific ImmTAC bridges T-cells to PRAME+ tumor cells, redirecting immunity |
| Melanoma | TEBE-AM (NCT05549297) [77] | III | Tebentafusp ± Pembrolizumab vs Std Care | Phase 1/2: 41% tumor shrinkage rate [77] | Targets gp100, a highly specific melanoma antigen, sparing healthy tissue |
| Melanoma | IMA203/IMA203CD8 (NCT03686124) [77] | Ib | Anzutresgene autoleucel (PRAME TCR-T) | cORR: 67% in UM; mDoR: 11 mo [77] | Engineered cellular therapy forces tumor to evolve against a fixed, potent immune attack |
| Ovarian | ACTOv (NCT05080556) [78] [2] | II | Adaptive Carboplatin Chemotherapy | Preclinical: AT prolonged survival vs MTD in mice [78] | Exploits fitness cost of platinum resistance in absence of drug |
| Ovarian | Multiple [79] [80] | III | PARP inhibitors (Olaparib, Niraparib) | Significant PFS benefit in BRCA-mut/HRD populations [79] | Synthetic lethality creates a "double-bind" against HR-deficient clones |
Table 2: Key Adaptive Therapy Clinical Trials and Protocols
| Trial Name / Cancer | Primary Intervention | Adaptive Protocol Summary | Biomarker for Decision-Making | Reported Outcome |
|---|---|---|---|---|
| Moffitt mCRPC Trial [2] | Abiraterone | Treat until PSA ↓50% from baseline. Pause until PSA returns to baseline, then repeat. | Prostate-Specific Antigen (PSA) | Median TTP: 33.5 mo (AT) vs 14.3 mo (SOC); 47% drug reduction [2] |
| ANZadapt (mCRPC) [2] | Abiraterone or Docetaxel | Adaptive dosing algorithm informed by mathematical model of PSA dynamics. | Prostate-Specific Antigen (PSA) | Trial ongoing; results pending [2] |
| ACTOv (Ovarian) [78] [2] | Carboplatin | Model-informed adaptive dosing based on tumor response and resistance monitoring. | Tumor burden (Imaging) & cfDNA [78] | Preclinically: AT improved survival without increasing mean daily drug dose [78] |
| NCT03543969 (Melanoma) [2] | BRAF/MEK inhibitors | Dose adjustment or skipping based on tumor response. | Tumor burden (Imaging) | Trial ongoing; specific protocol not detailed in results. |
Experimental Protocols for Evolutionary Therapy
Protocol: Adaptive Therapy with Abiraterone in mCRPC
Principle: This protocol uses on-treatment and off-treatment cycles to maintain a population of drug-sensitive cells that suppress the growth of resistant clones through competition for resources [2].
Materials:
- Abiraterone acetate + Prednisone
- Prostate-Specific Antigen (PSA) test
- Mathematical model for PSA dynamics (e.g., Lotka-Volterra competition model)
Procedure:
- Baseline Assessment: Obtain baseline PSA level and radiographic tumor assessment.
- Initial Treatment Cycle: Initiate continuous abiraterone + prednisone.
- Monitoring: Monitor PSA levels at regular intervals (e.g., every 4 weeks).
- Treatment Pause Criterion: When PSA decreases by ≥50% from baseline, hold abiraterone treatment.
- Treatment-Free Monitoring: Continue to monitor PSA levels during the treatment holiday.
- Re-initiation Criterion: When PSA returns to the baseline level, re-initiate abiraterone + prednisone.
- Iteration: Repeat steps 3-6 until clinical progression (defined by radiographic or symptomatic progression, not PSA rise alone).
Considerations: This protocol requires close patient monitoring and clinician comfort with intentional treatment breaks. Patient education on the evolutionary rationale is crucial for adherence [2].
Protocol: Model-Informed Adaptive Carboplatin for Ovarian Cancer
Principle: Adaptive therapy exploits the fitness deficits of platinum-resistant ovarian cancer cells in the absence of the drug. Sensitive cells, which regrow faster when the drug is withdrawn, are used to suppress the resistant population [78].
Materials:
- Carboplatin
- CT imaging for tumor burden assessment
- Cell-free DNA (cfDNA) analysis for tracking resistant subclones
- Bioinformatics pipeline for quantifying resistance emergence via cfDNA copy number changes [78]
Procedure:
- Baseline Modeling: Quantify baseline tumor burden via imaging and establish cfDNA profile.
- Initial Dose: Administer initial cycle of carboplatin at standard dose.
- Response Assessment: Perform imaging and cfDNA analysis after a set number of cycles to assess response and quantify the emergence of resistant subpopulations.
- Dose Adaptation:
- If tumor burden is reduced and resistant clone levels are low, reduce or pause carboplatin dosing.
- If tumor burden increases and resistant clone levels rise, resume or increase carboplatin dosing.
- Iterative Calibration: The mathematical model is recalibrated with each new patient data point (imaging and cfDNA) to refine subsequent dosing recommendations.
- Endpoint: Continue adaptive cycling until disease progression as per standard RECIST criteria.
Considerations: This protocol is resource-intensive, requiring frequent imaging, advanced cfDNA analysis, and integrated mathematical oncology support [78] [2].
Signaling Pathways and Workflow Visualizations
Diagram 1: ImmTAC mechanism for melanoma immunotherapy.
Diagram 2: Logic of adaptive therapy dosing.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Reagents and Materials
| Reagent / Material | Function / Application | Specific Example in Context |
|---|---|---|
| ImmTAC (Immune-mobilizing monoclonal TCR Against Cancer) [77] | Bispecific protein that bridges T-cells to tumor cells via a peptide-HLA complex on the target. | Brenetafusp (targeting PRAME) and Tebentafusp (targeting gp100) in advanced melanoma trials [77]. |
| Engineered TCR-T Cells [77] | Patient-derived T-cells genetically modified to express a T-cell receptor (TCR) targeting a specific tumor antigen. | Anzutresgene autoleucel (IMA203), a PRAME-directed TCR-T therapy, in metastatic uveal melanoma [77]. |
| PARP Inhibitors [79] [80] | Small molecule inhibitors of Poly (ADP-ribose) polymerase; induce synthetic lethality in HRR-deficient tumor cells. | Olaparib, Niraparib, Rucaparib as maintenance therapy in BRCA-mutated and HRD-positive ovarian cancer [79]. |
| Cell-free DNA (cfDNA) Analysis [78] | Liquid biopsy for non-invasive monitoring of tumor dynamics and resistant subclone emergence. | Tracking copy number changes in cfDNA to quantify the growth of carboplatin-resistant populations in ovarian cancer adaptive therapy [78]. |
| Ga-PSMA-11 / FDG-PET/CT [81] | Theranostic imaging for patient stratification; identifies tumors with sufficient target (PSMA) expression. | Mandatory for enrollment in the TheraP trial (177Lu-PSMA-617 vs Cabazitaxel) for mCRPC [81]. |
| Mathematical Models (ODEs, PDEs, ABMs) [2] | In silico modeling of tumor eco-evolutionary dynamics to predict response and design adaptive therapy protocols. | Used in Moffitt Cancer Center trials to design dosing schedules for abiraterone in mCRPC and BRAF/MEKi in melanoma [2]. |
Cancer therapy has traditionally relied on a straightforward principle: administer the maximum tolerated dose (MTD) to kill the greatest number of tumor cells [82]. This approach forms the current standard of care for most cancers and is the primary endpoint of phase I clinical trials [83]. However, this aggressive strategy inevitably imposes intense Darwinian selection pressure, eliminating drug-sensitive competitors and creating ecological space for resistant clones to proliferate uncontrollably—a phenomenon known as "competitive release" [1].
Evolutionary-based therapeutic strategies, particularly Adaptive Therapy (AT), present a paradigm shift by leveraging competitive interactions between sensitive and resistant cell populations [2]. Instead of maximal cell kill, AT aims for long-term tumor control by maintaining a stable population of therapy-sensitive cells that can suppress the expansion of resistant clones through resource competition [84]. This approach applies treatment breaks or dose reductions based on real-time monitoring of tumor burden, dynamically adjusting therapeutic intensity to maintain the tumor in a stable state [85].
Time-to-progression (TTP) serves as a crucial efficacy endpoint for comparing these strategies, measuring the duration from treatment initiation until disease progression. This application note provides a structured comparison of TTP metrics between AT and MTD approaches, detailing experimental protocols and analytical frameworks for researchers investigating evolutionary-driven treatment strategies in oncology.
Quantitative Performance Comparison
Table 1: Clinical Time-to-Progression Outcomes from Published Trials
| Cancer Type | Therapy Strategy | Median TTP (Months) | TTP Extension with AT | Cumulative Dose Reduction | Citation |
|---|---|---|---|---|---|
| Metastatic Castrate-Resistant Prostate Cancer | MTD (Standard Care) | 14.3 - 16.5 | Reference | Baseline | [2] |
| Adaptive Therapy | 27 - 33.5 | 12.2 - 19 months (89-116% increase) | 53% reduction | [2] | |
| BRAF-mutant Melanoma | Continuous (MTD) | Not specified | Reference | Baseline | [86] |
| Intermittent/Adaptive | Not specified | Significant extension reported | Not specified | [86] |
Table 2: Model-Predicted Performance Under Different Competitive Scenarios
| Competitive Intensity Between Cell Populations | AT Performance vs. MTD | Key Determinants | Optimal AT Strategy | |
|---|---|---|---|---|
| Strong Competition | Uniform improvement in TTP | High competition coefficients (α, β); Significant fitness cost of resistance | Fixed threshold protocol sufficient | [84] |
| Weak Competition | Conditional improvement in TTP | Initial tumor burden; Resistant fraction at diagnosis | Requires personalized, time-varying thresholds | [85] [84] |
| Minimal Competition | No improvement or worsened TTP | No significant fitness cost of resistance; Independent growth dynamics | MTD preferred; AT not recommended | [84] |
Experimental Protocols
Clinical Implementation Protocol for Adaptive Therapy
Objective: To dynamically control tumor burden through treatment modulation that maintains a stable population of therapy-sensitive cells.
Materials:
- Validated Biomarker: Prostate-Specific Antigen (PSA) for prostate cancer [2] or alternative validated biomarker specific to cancer type
- Imaging Modality: CT, MRI, or other appropriate imaging for tumor burden quantification
- Therapeutic Agent: Cytotoxic or targeted agent with defined MTD
- Monitoring Schedule: Defined intervals for biomarker assessment (e.g., 4-8 weeks)
Procedure:
- Baseline Assessment:
- Quantify initial tumor burden using predefined biomarker
- Establish baseline value (B₀)
Initial Treatment Phase:
- Administer standard MTD until tumor burden decreases by 50% from baseline (0.5×B₀)
- Document time to response and toxicity profile
Treatment Pause:
- Withhold therapy upon reaching 50% reduction threshold
- Monitor biomarker at predefined intervals (e.g., monthly)
Treatment Re-initiation:
- Resume therapy when tumor burden returns to baseline (B₀)
- Continue treatment until 50% reduction is achieved again
Iterative Adaptation:
- Repeat cycles of treatment and pause based on thresholds
- Consider adjusting thresholds based on individual tumor dynamics [85]
Endpoint Evaluation:
- Record TTP as time from treatment initiation to:
- Biochemical progression (e.g., PSA increase >25% above baseline)
- Radiographic progression (RECIST criteria)
- Clinical progression (symptomatic deterioration)
Mathematical Modeling Protocol for AT Optimization
Objective: To develop patient-specific mathematical models for predicting optimal adaptive therapy schedules and thresholds.
Materials:
- Computational Software: MATLAB, Python, or R with ODE solver capabilities
- Clinical Data: Longitudinal tumor burden measurements from individual patients
- Parameter Estimation Algorithm: Maximum likelihood or Bayesian estimation methods
Procedure:
- Model Selection:
- Implement Lotka-Volterra competition equations [84]: where S = sensitive cells, R = resistant cells, α and β = competition coefficients, D(t) = drug dose
Parameter Calibration:
- Use initial tumor dynamics to estimate parameters (rS, rR, α, β)
- Incorporate prior distributions from population data where available
Threshold Optimization:
- Simulate TTP across range of treatment pausing thresholds (e.g., 0.3×B₀ to 0.7×B₀)
- Identify optimal threshold that maximizes TTP for individual patient parameters
Validation:
- Compare model-predicted TTP with observed clinical outcomes
- Refine model structure and parameters through iterative comparison
Personalized Protocol Design:
- Generate patient-specific treatment schedule with optimized thresholds
- Implement time-varying thresholds for patients with weak competition dynamics [85]
Signaling Pathways and Workflow Visualization
Figure 1: Therapeutic Impact Pathways. MTD therapy eliminates sensitive cells, leading to competitive release and rapid expansion of resistant populations. Adaptive therapy maintains ecological suppression by preserving sensitive cells that compete with resistant variants.
Figure 2: Adaptive Therapy Clinical Workflow. The operational protocol for implementing adaptive therapy in clinical practice, showing the cyclical nature of treatment based on tumor burden thresholds.
The Scientist's Toolkit: Research Reagent Solutions
Table 3: Essential Research Materials and Computational Tools
| Tool Category | Specific Solution | Research Application | Key Features | |
|---|---|---|---|---|
| Mathematical Modeling Frameworks | Lotka-Volterra Competition Models | Quantifying sensitive-resistant cell dynamics | Parameters: competition coefficients (α, β), growth rates (rS, rR) | [84] |
| Bayesian Dose-Response Models | Phase I trial design; MTD estimation | Stable DLT probability estimation in small samples | [87] | |
| Clinical Monitoring Tools | Serum Biomarkers (e.g., PSA) | Real-time tumor burden tracking | Non-invasive monitoring; High-frequency assessment | [2] |
| Medical Imaging (CT, MRI) | Tumor volume quantification | Anatomical assessment; RECIST criteria application | [2] | |
| Computational Resources | Ordinary Differential Equation Solvers | Model simulation and prediction | MATLAB, R, or Python with scipy.integrate | [85] [84] |
| Parameter Estimation Algorithms | Model personalization to patient data | Maximum likelihood methods; Bayesian inference | [85] |
The comparative analysis of TTP metrics demonstrates that adaptive therapy can significantly extend time to progression compared to MTD across multiple cancer types, with particularly promising results in metastatic castrate-resistant prostate cancer showing median TTP extensions of 12.2-19 months. However, the efficacy of AT is highly context-dependent, governed by the intensity of competitive interactions between sensitive and resistant cell populations and the accuracy of treatment threshold selection.
Successful implementation requires personalized approach that matches the model to individual tumor dynamics [85], with strong competition scenarios yielding the most favorable outcomes. The integration of mathematical modeling with clinical practice provides a robust framework for optimizing these evolutionary-based strategies, potentially transforming palliative cancer care from a reactive to a dynamically managed process that significantly prolongs disease control.
Cancer therapy resistance, driven by the evolutionary dynamics of diverse tumor cell populations, remains a primary cause of treatment failure [88] [63]. Over 50% of colorectal cancer patients develop resistance after a transient initial response, a challenge mirrored across many cancer types [88]. Evolutionary forecasting—using mathematical models to predict the dynamics of tumor resistance—has emerged as a transformative approach for personalizing oncology. These models move beyond static genetic snapshots to simulate how heterogeneous tumor populations evolve under therapeutic pressure. However, the translation of model predictions into clinically actionable insights requires rigorous validation against real-world patient outcomes [89]. This Application Note provides a structured framework for this critical validation process, equipping researchers with protocols to benchmark model performance and build the evidentiary foundation needed for clinical integration.
Quantitative Benchmarks from Clinical Validation Studies
Validation of evolutionary models requires demonstrating their statistical association with clinically relevant endpoints. The table below synthesizes key performance metrics from seminal studies that have quantified the predictive power of evolutionary modeling.
Table 1: Quantitative Benchmarks from Evolutionary Model Validation Studies
| Study Focus / Cancer Type | Model Type & Key Predictors | Cohort Size | Key Performance Metrics | Clinical Outcome Correlation |
|---|---|---|---|---|
| Metastatic Colorectal Cancer (mCRC) [88] | Stochastic Branching Model; Number of resistant subclones at diagnosis | 599 patients | Hazard Ratios for patients with ≥3 resistant subclones: PFS: 1.09 [0.79–1.49]; OS: 1.54 [1.01–2.34] | The number of pre-existing resistant subclones was a significant predictor of poorer Progression-Free Survival (PFS) and Overall Survival (OS). |
| Pancreatic Cancer & Precision Medicine [66] | N/A; ctDNA clearance as a dynamic biomarker | N/A | 73% of ctDNA-cleared patients were progression-free at 12 months. | Clearance of circulating tumor DNA (ctDNA) post-treatment correlated strongly with long-term PFS. |
| Solid Tumors (Various) [90] | Single-cell RNA-seq analysis via CellResDB; TME composition | 1,391 patient samples; 4.7 million cells | Database covers 24 cancer types; 56.58% samples from responders, 38.89% from non-responders. | Enables validation of model-predicted resistance mechanisms against real patient TME data. |
These studies underscore that model-derived parameters, such as the number of resistant subclones, and dynamic biomarkers, like ctDNA clearance, provide quantifiable links to patient survival [88] [66]. Furthermore, large-scale resources like CellResDB are invaluable as independent validation benchmarks for model predictions regarding the tumor microenvironment [90].
Core Protocols for Model Validation
Protocol: Calibrating a Stochastic Evolutionary Model with Longitudinal Clinical Data
This protocol details the process of calibrating a parsimonious stochastic branching model using longitudinal tumor size measurements, a method validated in mCRC [88].
Research Reagent Solutions:
- Clinical Trial Data Source: Data from platforms like Project Data Sphere (e.g., NCT00115760), containing longitudinal tumor measurements (e.g., longest lesion diameter from CT scans), PFS, and OS [88].
- Tumor Measurement Converter: Algorithm to convert imaging data into tumor cell counts. A standard formula is:
Cell number = (long axis) * (short axis)^2 / 2 * 10^9, assuming 1 cm³ contains ~10⁹ cells and a detection limit of 10⁷ cells [88]. - Software for NLME Modeling: Platforms such as MonolixSuite for performing Non-Linear Mixed Effect modeling using the SAEM algorithm [88].
Workflow:
- Data Preparation and Tumor Burden Calculation:
- Extract the longest diameters of target lesions (e.g., liver metastases) from all available CT scans for each patient.
- Calculate the short axis using an average long-to-short axis ratio (e.g., 1.31).
- Apply the tumor cell number conversion formula to transform all longitudinal measurements into a time series of total tumor cell burden [88].
Model Structuring:
- Define a model with one sensitive subclone (S) and a cascade of resistant subclones (e.g., R1, R2, R3).
- The system is described by ordinary differential equations (ODEs) where:
- Sensitive cells divide at rate
bsand die (including therapy-induced death) at rated + dtrt. They transition to the first resistant subclone at a rateμper cell division. - Resistant subclones divide at rate
brand die at rated. Each subsequent resistant subclone has a progressively reduced therapy-induced death rate (dtrt1>dtrt2>dtrt3) [88].
- Sensitive cells divide at rate
- The model is optimized to fit the longitudinal tumor cell count data.
Parameter Optimization via Deterministic Limits:
- Directly optimizing the stochastic model in a population framework (NLME) is computationally prohibitive. Therefore, optimize its deterministic approximation (the ODE system) using the NLME method.
- Use the SAEM algorithm in MonolixSuite to estimate population parameters and, crucially, individual empirical Bayes estimates (EBEs) for each patient's specific parameters (
bs,br,d,μ,dtrt) [88].
Extraction of Predictive Features:
- From the optimized individual patient models, extract quantitative features for survival analysis. The most significant feature is the number of resistant subclones present at diagnosis [88].
Diagram 1: Workflow for model calibration from imaging data.
Protocol: Correlating Model Outputs with Clinical Survival Data
This protocol validates the prognostic value of features derived from the evolutionary model.
Workflow:
- Feature and Outcome Matrix Construction:
- Create a dataset where each row corresponds to a patient.
- Columns include the model-derived features (e.g., number of resistant subclones at diagnosis, growth/death rate estimates) and key clinical covariates (e.g., treatment arm, number of metastatic sites, LDH levels, KRAS status) [88].
- Append the definitive clinical endpoints: Progression-Free Survival (PFS) and Overall Survival (OS) data.
- Statistical Modeling for Survival Analysis:
- Employ Cox proportional hazards models.
- To prevent overfitting and for robust feature selection, couple the Cox model with the Least Absolute Shrinkage and Selection Operator (LASSO) algorithm.
- The model will identify which combination of evolutionary parameters and clinical variables most strongly predicts PFS and OS, generating hazard ratios (like those in Table 1) for each significant predictor [88].
Diagram 2: Statistical validation of model features against survival.
The Scientist's Toolkit: Key Research Reagents & Databases
Successful validation relies on integrating robust models with high-quality data. The following table catalogues essential resources for evolutionary forecasting research.
Table 2: Essential Research Resources for Evolutionary Forecasting
| Item Name | Function / Utility | Key Features / Application Notes |
|---|---|---|
| Project Data Sphere | Source of raw, longitudinal clinical trial data for model calibration and testing. | Provides patient-level data, including tumor measurements, treatment history, and survival outcomes. Ideal for training and validating models like the stochastic branching model [88]. |
| CellResDB | Single-cell RNA-seq database for validating model-predicted TME mechanisms. | Contains nearly 4.7 million cells from 1,391 patient samples across 24 cancers. Use to confirm predicted cell-cell communication or shifts in TME composition linked to resistance [90]. |
| The Cancer Genome Atlas (TCGA) | Repository of multi-omics and clinical data for pan-cancer analysis. | Provides genomic, transcriptomic, epigenomic, and proteomic data for over 10,000 patients. Useful for initial model development and understanding baseline heterogeneity [91]. |
| NLME Software (e.g., MonolixSuite) | Platform for population parameter estimation in mixed-effect models. | Implements the SAEM algorithm, crucial for handling sparse, noisy longitudinal clinical data and deriving individual patient parameters from a population model [88]. |
| Cox-LASSO Model | Statistical framework for feature selection and survival prediction. | Prevents overfitting when correlating multiple model features and clinical covariates with survival outcomes. Identifies the most parsimonious, predictive feature set [88]. |
Advanced Validation: Integrating Single-Cell and Spatial Transcriptomics
The gold standard for validating evolutionary models is moving beyond bulk tumor metrics to single-cell and spatial resolution. Models predicting the emergence of a resistant subclone can be directly tested by analyzing pre- and post-treatment samples at the single-cell level.
Protocol: In Silico to In Vivo Model Validation with CellResDB
Workflow:
- Generate a Model Prediction: Simulate therapy response and output a prediction of a specific cellular change (e.g., "expansion of a SPP1+ macrophage population and exclusion of cytotoxic T-cells upon acquisition of resistance").
- Data Retrieval via CellResDB-Robot: Use the integrated AI agent, CellResDB-Robot, to conversationally query the database. For example: "Retrieve all pre- and post-treatment samples from non-responders with colorectal cancer treated with anti-PD-1 therapy" [90].
- Hypothesis Testing: Use the "Search by Cell" function to compare the proportions of the predicted cell populations between responders and non-responders. Use the "Search by Gene" function to validate the predicted gene expression signature (e.g.,
SPP1,TOX,ENTPD1) in the relevant cell types [90]. - Spatial Context Validation: If the model makes spatial predictions (e.g., formation of fibroblast barriers), correlate findings with spatial transcriptomic datasets to confirm the predicted geographical organization of resistant niches [92].
Validating evolutionary models against clinical outcomes transforms them from mathematical exercises into reliable tools for oncology. The framework presented here—combining quantitative benchmarking of survival correlations, rigorous calibration protocols, and validation with next-generation molecular datasets—provides a roadmap for this critical process. As these models become more integrated with AI and real-time data streams like ctDNA [66] [92], their predictive power will increase. Adherence to robust validation standards is the essential step to ensure these forecasts reliably guide drug development and personalize therapeutic strategies, ultimately improving patient survival.
Within the paradigm of evolutionary modeling for cancer therapy, a primary objective is to exploit the fitness costs of resistance mechanisms to suppress the outgrowth of treatment-resistant subclones. This approach often necessitates a departure from continuous maximum tolerated dose (MTD) strategies in favor of dynamic, adaptive dosing. These alternative schedules frequently result in a significant reduction in cumulative drug dose compared to standard regimens, which directly translates into improved toxicity profiles and economic benefits. This Application Note details the quantitative benefits and provides a protocol for implementing an adaptive therapy strategy based on evolutionary dynamics, using metastatic castrate-resistant prostate cancer (mCRPC) as a model system.
Key Data and Economic Outcomes
Clinical data from a pilot trial of adaptive abiraterone therapy in mCRPC demonstrates the tangible benefits of this approach. The table below summarizes the core quantitative outcomes comparing adaptive therapy to standard-of-care (SOC) continuous dosing [17].
Table 1: Economic and Clinical Outcomes of Adaptive vs. Standard Abiraterone Therapy
| Metric | Standard Continuous Therapy | Adaptive Therapy | Benefit |
|---|---|---|---|
| Median Time to Radiographic Progression | ~16.5 months [17] | ≥27 months [17] | Extended treatment efficacy |
| Reduction in Cumulative Drug Dose | Baseline (100%) | 53% average reduction [17] | Lower drug acquisition costs |
| Range of Drug Dose Reduction | Not Applicable | Up to >75% for some patients [17] | Significant cost-saving potential |
| Adverse Events (Grade ≥2) | Reported in literature | None necessitating drug discontinuation in the pilot cohort [17] | Reduced toxicity management costs |
These outcomes stem from the core protocol of adaptive therapy, which synchronizes drug administration with the evolutionary dynamics of the tumor, allowing for treatment holidays once a specific response threshold is met.
Experimental Protocol: Adaptive Therapy Based on Evolutionary Dynamics
This protocol outlines the methodology for implementing adaptive abiraterone therapy in mCRPC, as validated in a clinical trial [17]. The core principle is to forgo continuous MTD in favor of on/off treatment cycles guided by serum PSA levels, a biomarker of tumor burden.
Materials and Reagents
- Abiraterone acetate (Zytiga)
- Prednisone
- Leuprolide (or other GnRH agonist for continuous androgen deprivation)
- Equipment for PSA level quantification
Procedure
- Pre-treatment: Confirm patient diagnosis of mCRPC. Obtain baseline PSA level.
- Initiation Cycle: Begin continuous administration of abiraterone (e.g., 1000 mg daily) with prednisone.
- Monitoring: Measure serum PSA at regular intervals (e.g., monthly).
- Treatment Cessation (First Cycle): When the PSA level drops to 50% of the pre-treatment baseline value, discontinue abiraterone and prednisone. Note: Leuprolide is continued throughout.
- Treatment Holiday: Monitor PSA levels at regular intervals (e.g., monthly). Allow the tumor to regrow.
- Re-initiation of Therapy: When the PSA level returns to the original pre-treatment baseline value, restart abiraterone and prednisone.
- Subsequent Cycles: Repeat steps 4-6 for each subsequent cycle. The duration of treatment holidays will vary based on individual patient tumor dynamics.
- Endpoint: The cycle continues until radiographic or clinical progression is documented.
Underlying Evolutionary Game Theory Model
The protocol is informed by a mathematical model that frames the tumor as three competing cell types [17]:
- T+ cells: Androgen-dependent; require exogenous testosterone.
- TP cells: Androgen-producing; express CYP17A1 and create a testosterone source.
- T− cells: Androgen-independent; resistant to abiraterone.
Continuous MTD abiraterone eliminates T+ and TP cells, causing competitive release of resistant T− cells and rapid progression. The adaptive protocol, by allowing regrowth of therapy-sensitive T+ and TP cells during drug holidays, uses them to suppress the expansion of the less-fit T− populations in the absence of drug pressure.
Visualization of Adaptive Therapy Workflow and Dynamics
The following diagrams illustrate the logical workflow of the adaptive therapy protocol and the corresponding population dynamics of cancer cell subtypes.
Adaptive Therapy Protocol
Tumor Population Dynamics
The Scientist's Toolkit: Research Reagent Solutions
The following table lists essential reagents and models for researching evolutionary therapy and resistance mechanisms [17] [93].
Table 2: Key Research Reagents and Models for Evolutionary Therapy Research
| Item/Category | Function/Application | Specific Examples / Notes |
|---|---|---|
| Mathematical Modeling Software | Simulating evolutionary dynamics and predicting optimal adaptive therapy schedules. | Custom scripts using Lotka-Volterra equations or other ecological models [17]. |
| In Vivo Xenograft Models | Preclinical testing of adaptive therapy protocols in a controlled environment. | Mouse models implanted with a mix of therapy-sensitive and -resistant cancer cell lines [17]. |
| Circulating Tumor DNA (ctDNA) Analysis | Monitoring clonal evolution and emergence of resistance mutations non-invasively. | Targeted NGS panels to track allele frequencies of resistance-conferring mutations. |
| Drug-Resistant Cell Lines | Studying the fitness costs and competitive interactions of resistant subpopulations. | Generated via gradual exposure to increasing drug concentrations in vitro [93]. |
| Quantitative Systems Pharmacology (QSP) Models | Integrating PK/PD with a systems-level understanding of tumor biology and immune interactions. | Multi-scale models to simulate tumor growth and treatment response for in silico trials [94]. |
Conclusion
Evolutionary modeling represents a paradigm shift in cancer therapy, moving beyond the futile pursuit of complete eradication to the strategic management of resistance dynamics. The synthesis of Darwinian principles with computational oncology offers powerful frameworks for delaying progression through adaptive dosing, evolutionary steering, and rational drug sequencing. While clinical implementation faces challenges in monitoring, interdisciplinary collaboration, and addressing non-genetic resistance, early trials demonstrate significant improvements in progression-free survival with reduced toxicity. Future directions must focus on developing predictive biomarkers for evolutionary trajectories, personalizing adaptive algorithms through digital twins, and expanding clinical validation across cancer types. This evolution-informed approach promises to transform incurable cancers into chronically managed conditions, ultimately improving patient outcomes through biologically smarter, rather than merely more intensive, therapeutic strategies.
References
- 1. The Evolution and Ecology of Resistance in Cancer - PMC Therapy [https://pmc.ncbi.nlm.nih.gov/articles/PMC5830903/]
- 2. Bringing evolutionary cancer therapy to the clinic: a systems approach | npj Systems Biology and Applications [https://www.nature.com/articles/s41540-025-00528-8]
- 3. Preventing evolutionary rescue in cancer - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10690287/]
- 4. Evolutionary rescue model informs strategies for driving cancer cell populations to extinction - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11623570/]
- 5. Evolutionary Game Theory: Darwinian Dynamics and the G Function Approach [https://www.mdpi.com/2073-4336/12/4/72]
- 6. Beyondcell: targeting cancer heterogeneity in single-cell... therapeutic [https://genomemedicine.biomedcentral.com/articles/10.1186/s13073-021-01001-x]
- 7. Mathematical models of targeted cancer | British Journal of... therapy [https://www.nature.com/articles/6603310?error=cookies_not_supported&code=300b6868-4fe8-4ea4-9f85-6007439ead9b]
- 8. Decoding Drug Resistance in Cancer: Mechanisms , Clinical... [https://biomedres.us/fulltexts/BJSTR.MS.ID.009921.php]
- 9. Frontiers | Single-cell transcriptomics in metastatic breast cancer ... [https://www.frontiersin.org/journals/genetics/articles/10.3389/fgene.2025.1669741/full]
- 10. Integrating evolutionary dynamics into cancer therapy [https://www.nature.com/articles/s41571-020-0411-1?error=cookies_not_supported]
- 11. Breaking barriers: we need a multidisciplinary approach to tackle cancer drug resistance | BJC Reports [https://www.nature.com/articles/s44276-025-00129-2]
- 12. Frontiers | Emerging trends and knowledge networks in pan-cancer sorafenib resistance: a 20-year bibliometric investigation [https://www.frontiersin.org/journals/pharmacology/articles/10.3389/fphar.2025.1581820/full]
- 13. Frontiers | A bibliometric visualization of resistance to lung cancer immunotherapy: a decade of research progress (2014–2024) [https://www.frontiersin.org/journals/oncology/articles/10.3389/fonc.2025.1656967/full]
- 14. Acquired resistance in cancer: towards targeted therapeutic strategies - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12307123/]
- 15. Roadmap on plasticity and epigenetics in cancer - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9190291/]
- 16. Frontiers | Niche-specific epigenetic interventions in the spatially... [https://www.frontiersin.org/journals/molecular-biosciences/articles/10.3389/fmolb.2025.1704311/full]
- 17. Integrating evolutionary dynamics into... | Nature Communications [https://www.nature.com/articles/s41467-017-01968-5?error=cookies_not_supported]
- 18. Molecular mechanisms and therapeutic strategies in overcoming chemotherapy resistance in cancer | Molecular Biomedicine [https://link.springer.com/article/10.1186/s43556-024-00239-2]
- 19. Why Do Cancer Treatments Stop Working? - NCI [https://www.cancer.gov/about-cancer/treatment/research/drug-combo-resistance]
- 20. Eco‐oncology: Applying ecological to understand and... principles [https://pmc.ncbi.nlm.nih.gov/articles/PMC7452771/]
- 21. Frontiers | Ecology of Human Medical Enterprises: From Disease... [https://www.frontiersin.org/journals/ecology-and-evolution/articles/10.3389/fevo.2022.879130/full]
- 22. Tracking Treatment Resistance in Metastatic Breast Cancer - NCI [https://www.cancer.gov/news-events/cancer-currents-blog/2017/metastatic-breast-cancer-treatment-resistance-evolution]
- 23. Application of Evolutionary Principles to Cancer Therapy - PubMed [https://pubmed.ncbi.nlm.nih.gov/26527288/]
- 24. The Evolution and Ecology of Resistance in Cancer Therapy - PubMed [https://pubmed.ncbi.nlm.nih.gov/33139405/]
- 25. Mathematical Details on a Cancer Resistance Model - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7325889/]
- 26. A Review of Mathematical Models for Tumor Dynamics and Treatment... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6813171/]
- 27. Mathematical modeling in radiotherapy for cancer : a comprehensive... [https://ro-journal.biomedcentral.com/articles/10.1186/s13014-025-02626-7]
- 28. [2109.01849] A Case Study of Agent-Based Models for Evolutionary Game Theory [https://arxiv.org/abs/2109.01849]
- 29. the Gaming -immunity cycle by synchronizing treatment... cancer [https://viterbischool.usc.edu/news/2025/08/gaming-the-cancer-immunity-cycle-by-synchronizing-treatment-schedules/]
- 30. A survey of open questions in adaptive therapy: Bridging mathematics and clinical translation - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC10036119/]
- 31. Deriving Optimal Treatment Timing for Adaptive ... | medRxiv Therapy [https://www.medrxiv.org/content/10.1101/2025.04.01.25325056v1]
- 32. Adaptive Treatment Strategies in Chronic Disease - PMC [https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2739674/]
- 33. Integrating Mathematical Modeling into the Roadmap for Personalized Adaptive Radiation Therapy - PubMed [https://pubmed.ncbi.nlm.nih.gov/31421904/]
- 34. Exploiting evolutionary to induce steering drug collateral ... sensitivity [https://www.nature.com/articles/s41467-020-15596-z?error=cookies_not_supported&code=9363dce0-a201-4be7-8374-1971d8df7d88]
- 35. - Wikipedia Evolutionary therapy [https://en.wikipedia.org/wiki/Evolutionary_therapy]
- 36. Diverse evolutionary pathways challenge the use of collateral ... [https://elifesciences.org/articles/85023]
- 37. Integrative analysis of therapy and transcriptomic profiling... resistance [https://ro-journal.biomedcentral.com/articles/10.1186/s13014-022-02052-z]
- 38. Mathematical modeling and computational prediction of cancer drug... [https://pmc.ncbi.nlm.nih.gov/articles/PMC6402530/]
- 39. Eradicating Metastatic Cancer and the Eco-Evolutionary Dynamics of Anthropocene Extinctions - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC7771333/]
- 40. High potency of sequential therapy with only β-lactam antibiotics | eLife [https://elifesciences.org/articles/68876]
- 41. Rapid expansion and extinction of antibiotic resistance mutations... [https://pubmed.ncbi.nlm.nih.gov/35264582/]
- 42. measurement of phenotype dynamics during Quantitative ... cancer [https://www.nature.com/articles/s41467-025-59479-7?error=cookies_not_supported&code=e9782184-5fce-4ee2-b4e6-eb5e121e3a90]
- 43. Development of Drug-resistant Cell Lines for Experimental Procedures - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12404681/]
- 44. Emerging artificial intelligence-driven precision therapies in tumor drug ... [https://molecular-cancer.biomedcentral.com/articles/10.1186/s12943-025-02321-x]
- 45. Optimal control to reach eco- evolutionary stability in... | PLOS One [https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0243386]
- 46. Programming tumor with selection... | Nature Biotechnology evolution [https://www.nature.com/articles/s41587-024-02271-7?error=cookies_not_supported]
- 47. State-dependent evolutionary models reveal modes of solid tumour ... [https://www.nature.com/articles/s41559-023-02000-4?error=cookies_not_supported&code=c6b0a224-0298-4beb-99b2-c9ddb5f97fcd]
- 48. Enhancing detection and monitoring of circulating tumor cells... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12124603/]
- 49. Advancing precision medicine: the transformative role of artificial intelligence in immunogenomics, radiomics, and pathomics for biomarker discovery and immunotherapy optimization | Cancer Biology & Medicine [https://www.cancerbiomed.org/content/early/2025/01/02/j.issn.2095-3941.2024.0376]
- 50. Liquid biopsy – a narrative review with an update on current US governmental clinical trials targeting immunotherapy - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12333414/]
- 51. Frontiers | Addressing the current challenges in the clinical application of AI-based Radiomics for cancer imaging [https://www.frontiersin.org/journals/medicine/articles/10.3389/fmed.2025.1674397/full]
- 52. therapy: can Adaptive - cancer factors become its achilles... non genetic [https://www.nature.com/articles/s41388-025-03582-y?error=cookies_not_supported&code=7b7ed756-f13e-407a-8a77-5e52abf03b27]
- 53. - Non Drug Genetic in Adaptive Resistance Cancer [https://www.frontiersin.org/research-topics/20915/non-genetic-adaptive-drug-resistance-in-cancer/magazine]
- 54. Editorial: Non - genetic drug adaptive in resistance - PMC cancer [https://pmc.ncbi.nlm.nih.gov/articles/PMC9716313/]
- 55. Emerging insights of tumor heterogeneity and drug resistance mechanisms in lung cancer targeted therapy | Journal of Hematology & Oncology | Full Text [https://jhoonline.biomedcentral.com/articles/10.1186/s13045-019-0818-2]
- 56. Multilevel Mechanisms of Cancer Drug Resistance - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11594576/]
- 57. : Modulating Therapy conserved heat shock... resistance evolutionarily [https://pubmed.ncbi.nlm.nih.gov/39986370/]
- 58. Introduction | Cancer Cell Plasticity: Cracking the Code of Adaptation... [https://www.eacr.org/conference/cancercellplasticity2025]
- 59. Scientific Programme - ESC Cardio- Oncology [https://www.escardio.org/Congresses-Events/Cardio-Oncology/Scientific-sessions]
- 60. [2506.20684] A bibliometric study on mathematical ... oncology [https://arxiv.org/abs/2506.20684]
- 61. Cancer statistics, 2025 - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11745215/]
- 62. Application of evolutionary principles to cancer therapy - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC4693617/]
- 63. A theoretical quantitative for model of evolution ... cancer [https://biologydirect.biomedcentral.com/articles/10.1186/1745-6150-5-25]
- 64. of Combination Treatment Strategies To... Evolutionary Modeling [https://pmc.ncbi.nlm.nih.gov/articles/PMC3230244/]
- 65. Evolutionary drug scheduling models with different toxicity metabolism in cancer chemotherapy - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S1568494606001074]
- 66. Experts Forecast Cancer and Treatment Advances in Research 2025 [https://www.aacr.org/blog/2025/01/10/experts-forecast-cancer-research-and-treatment-advances-in-2025/]
- 67. Bringing evolutionary cancer therapy to the clinic : a systems... [https://pmc.ncbi.nlm.nih.gov/articles/PMC12117075/]
- 68. Stackelberg Evolutionary Games of Cancer Treatment: What... [https://link.springer.com/article/10.1007/s13235-024-00609-z]
- 69. Frontiers | Evolutionary Dynamics of Treatment-Induced Resistance in Cancer Informs Understanding of Rapid Evolution in Natural Systems [https://www.frontiersin.org/journals/ecology-and-evolution/articles/10.3389/fevo.2021.681121/full]
- 70. The evolutionary theory of cancer ... | Nature Reviews Cancer [https://www.nature.com/articles/s41568-024-00734-2?error=cookies_not_supported]
- 71. Multiscale Modeling of Tumor Angiogenesis and Resistance ... [https://www.preprints.org/manuscript/202507.2175/v1]
- 72. Masters of adaptation: How cancer and immune cell... | PLOS Biology [https://journals.plos.org/plosbiology/article?id=10.1371/journal.pbio.3003301]
- 73. methods of different tumor organoids and their application in... Modeling [https://www.oaepublish.com/articles/cdr.2025.34]
- 74. Quantitative measurement of phenotype dynamics during cancer drug resistance evolution using genetic barcoding | Nature Communications [https://www.nature.com/articles/s41467-025-59479-7]
- 75. of myeloid-mediated immunotherapy Evolution in... | Nature resistance [https://www.nature.com/articles/s41586-024-08290-3?error=cookies_not_supported&code=a2a7f803-b132-4696-a289-7f7348221de7]
- 76. What's the latest update on the ongoing clinical related to... trials [https://synapse.patsnap.com/article/whats-the-latest-update-on-the-ongoing-clinical-trials-related-to-metastatic-castration-resistant-prostate-cancer]
- 77. to Watch: October Melanoma - Clinical ... Trials 2025 Melanoma [https://www.curemelanoma.org/blog/melanoma-clinical-trials-to-watch-fall-2025]
- 78. Adaptive Therapy Exploits Fitness Deficits in Chemotherapy-Resistant Ovarian Cancer to Achieve Long-Term Tumor Control - PubMed [https://pubmed.ncbi.nlm.nih.gov/40299825/]
- 79. Therapeutic landscape of ovarian cancer: recent advances and emerging therapies - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12344919/]
- 80. Ovarian cancer targeted therapy: current landscape and future challenges - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC12088972/]
- 81. TheraP: a randomized phase 2 trial of 177 Lu-PSMA-617 theranostic... [https://pubmed.ncbi.nlm.nih.gov/31638341/]
- 82. Why maximum tolerated dose? - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC6783596/]
- 83. Model-guided determination of maximum tolerated dose in phase I clinical trials: evidence for increased precision - PubMed [https://pubmed.ncbi.nlm.nih.gov/8423626/]
- 84. Conditional success of adaptive : the role of treatment-pausing... therapy [https://arxiv.org/html/2502.09392v1]
- 85. Deriving Optimal Treatment Timing for Adaptive : Matching... Therapy [https://pubmed.ncbi.nlm.nih.gov/40921859/]
- 86. Evolutionary Dynamics and Intermittent Therapy for Metastatic Cancers - PubMed [https://pubmed.ncbi.nlm.nih.gov/37418680/]
- 87. [2502.14278] Improving Maximum Tolerated Dose Selection in Model-Assisted Designs for Phase I Trials through Bayesian Dose-Response Model [https://arxiv.org/abs/2502.14278]
- 88. tumor Modeling dynamics to evolutionary ... predict clinical outcomes [https://pmc.ncbi.nlm.nih.gov/articles/PMC7002273/]
- 89. of Mathematical : When to Models Novel Cancer ... Predict Therapies [https://link.springer.com/article/10.1007/s11538-019-00640-x]
- 90. Deciphering cancer therapy resistance via patient-level single-cell transcriptomics with CellResDB | Communications Biology [https://www.nature.com/articles/s42003-025-08457-2]
- 91. Big data in basic and translational cancer research - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC9443637/]
- 92. Report: Research of the Evolution Industry (2023– Cancer ) 2025 [https://www.onedaymd.com/2025/02/research-report-evolution-of-cancer.html]
- 93. Drug resistance in human cancers — Mechanisms and implications - ScienceDirect [https://www.sciencedirect.com/science/article/abs/pii/S0024320524004971]
- 94. Advancing Cancer Drug Development with Mechanistic Mathematical Modeling: Bridging the Gap between Theory and Practice - PMC [https://pmc.ncbi.nlm.nih.gov/articles/PMC11795844/]